
Functional assessments for anterior cruciate ligament reconstruction return to sport
Introduction
Re-ruptures of a reconstructed anterior cruciate ligament (ACL) are frequently observed with an incidence of 5% to 18%, or more, depending on the follow-up (1-3). Half of these re-ruptures can be observed within the first twelve postoperative months (1,3). Of note, many studies found an even higher incidence of contralateral ACL injuries, with a reported extraordinarily high incidence of 16% or higher (1-3). Even the implementation of various prevention programs has not substantially reduced this risk (4). Factors associated with graft failure or contralateral ACL injuries are younger age (1,3), male gender (1,2), technical errors (i.e., poor bone tunnel placement) and graft choice (i.e., allografts, hamstring tendons) (5), the biomechanical properties of the graft during the ligamentization process (6), as well as return to pivoting activities (1). Further, it has been shown that muscular and proprioceptive deficits may be observed for more than one year following ACL reconstruction (7,8). Therefore, many surgeons prefer to postpone the return to sport until six months or later. However, most sports medicine specialists do not utilize functional tests that may provide more accurate feedback regarding the optimal timing for “safe” return to sport. Reasons for this could be that the athlete is under pressure to return to competition as soon as possible, the high time commitment associated with performing many functional tests, or unawareness of functional tests and lack of evidence especially regarding normative values. Currently, patients usually return to sports within 6 to 12 months following ACL reconstruction (9,10) and most of the surgeons rely solely on physical exams, although some surgeons also utilize more objective measures such as Lysholm and International Knee Documentation Committee scores.
When applying functional performance tests (11), many of the sports medicine specialists perform isolated tests. Hop tests are the most commonly used performance tests (12-14). However, these tests have been criticized for not being sufficient to properly evaluate the patients´ functional capability following ACL reconstruction (15). Even commonly available isokinetic muscle strength tests do not necessarily correlate with knee function, suggesting that they should not be used in isolation (16-18). Based on these facts, functional assessment following ACL reconstruction should consist of multiple tests to properly evaluate the functional abilities of the patient to determine a safe return to sport.
Different test batteries do exist (19-21). However, the utility of these tests to adequately predict readiness for return to sport is limited (15). Further, the test batteries do not compare the obtained data with normative values and were generally performed not before one year after surgery. However, functional assessment following ACL reconstruction should not only be used as a tool to determine the readiness to return to sport, but also to evaluate the progress over time during the rehabilitation in order to properly address possible functional and sports specific deficits.
Demands on functional assessment
Functional assessment to determine return to sport following ACL reconstruction requires time, personnel, infrastructure, equipment and finally money. The ideal functional assessment includes movement analyses (either two dimensional or three dimensional) to detect abnormal motion patterns (i.e., dynamic valgus landing), strength tests, agility tests, proprioception and postural tests. The ideal test battery including all of these tests would have low cost, time, and personnel efficiency. Therefore, such a test battery with the highest quality standards is clinically not practicable.
To date, little evidence regarding normative values for different tests exists (22,23), with most of the sports medicine specialists relying on limb symmetry indices (LSI). However, it has been shown, that the clinically acceptable LSI of >90% does not necessarily detect sufficiently functional deficits, since both limbs are negatively affected by an ACL reconstruction (24). Further, studies evaluating the LSI often do not take into account limb-dominance when interpreting the results. A recently published study on healthy subjects by Hildebrandt et al. (23) has shown that clinically relevant side-to-side differences between the dominant and non-dominant leg exist, especially for the single-legged counter movement jump. In that study the LSI was found to be up to 124%, on average, for the counter movement jump, indicating a 24% better performance in the dominant leg. Therefore, it is questionable whether a LSI >90% for such a test is clinically acceptable.
In summary, functional assessment following ACL reconstruction should cover the status of the knee, as well as motoric skills in a clinically applicable setting. Further, data analysis must be efficient and the results should be compared to normative values to allow for proper interpretation. Ideally, functional assessment should be performed more than once following ACL reconstruction to address functional deficits during the rehabilitation.
What do we need to assess?
Physical examination
Before any functional assessment is begun, a standard physical exam to evaluate ligament laxity, range of motion and effusion needs to be performed. Normal laxity and an inflammation-free knee are prerequisites for any return to sport. Especially, quantitative laxity measures could help to detect even subtle side-to-side differences (25).
Muscle strength
Muscle strength can be evaluated with either isokinetic strength measurements or jumping tasks, such as plyometric jumps, counter movement jumps or different hop tests.
Muscle strength testing with an isokinetic dynamometer (i.e., Contrex® MJ; CMV AG, Zurich, Switzerland) for the flexor and extensor apparatus can be a useful tool to evaluate the rehabilitation progress and to determine return to sport. Usually, peak extensor and flexor torque (Nm) are obtained at different angular velocities. Since it has been shown that muscle strength deficits continue to persist for more than one year postoperatively (18,26-28), it is recommended to perform muscle strength tests more than once during rehabilitation. Data can be interpreted based on the pre-injury state (longitudinally), or more commonly using the LSI. As mentioned above, a LSI >90% is a commonly accepted threshold for return to play. However, it has been shown that the hamstring to quadriceps ratio might be a more important predictor for muscular imbalances around the knee than the maximum isokinetic torque (29). A decreased hamstring to quadriceps ratio was also found to be a risk factor for further knee injuries (30). Kyritsis et al. reported a hazard ratio of 10.6 for subsequent ACL re-ruptures per 10% difference in the hamstring to quadriceps ratio (31). Thus, restoration and evaluation of both extensor and flexor muscle strength is of high importance following ACL reconstruction and the hamstring to quadriceps ratio might represent a good parameter for decision-making regarding return to sport. Ideally, the hamstring to quadriceps ratio should be around 80% (29,30). In addition to knee extension and flexion strength, hip and trunk muscle strength should be considered in either screening programs or functional assessments following ACL reconstruction, as they are associated with an increased ACL injury risk and inferior performance during functional tasks (i.e., single leg step-down test) (32,33).
Hop tests are commonly used as functional outcome measures following ACL reconstruction, since they indicate muscle strength and dynamic muscle co-activation. Clinically, single-leg hop performance correlates with self-reported knee function return to play (13,17). Amongst the different available jump tests, the vertical jump, jump for distance and the side hop have been shown to have the highest sensitivity in detecting functional deficits following ACL reconstruction (34). The tests should be performed with one and two legs, since it has been shown that deficits might not be evident during bipedal tasks (21). Besides height and distance, the power (W/kg) as well as ground contact time can be obtained with an acceleration sensor (i.e., Myotest SA, Sion, Switzerland). However, care should be taken when interpreting the hop test results. It has been shown that hop test performance correlates strongly with fatigue (12). Therefore, the tests should be performed under non-fatigued and fatigued test conditions. Also, the time point of testing during the rehabilitation is of high importance. In the early phases, subjects might not be able to perform any jumping tests, whereas in very late phases the sensitivity to detect functional deficits might be decreased. However, it has been shown that hop test performance is significantly decreased up to 9 months following ACL reconstruction (35). Video analyses or visual feedback from a supervisor can be added to screen for abnormal motion patterns during the jumping task such as functional knee valgus as a secondary ACL injury prevention (36).
Even though, hop test performance does correlate moderately with isokinetic quadriceps strength (37), such tests cannot replace muscle strength testing.
Speed and agility
Speed (i.e., running speed, ground contact time during plyometric jumps) and agility (i.e., ability to perform cutting maneuvers) are prerequisites for many competitive sports and should therefore be included in any functional assessment following ACL reconstruction. Such movements (cutting/pivoting maneuvers, deceleration) are commonly related to non-contact ACL injuries and proper intervention with motion modification can decrease the injury risk (38). Therefore, various prevention programs are designed to screen for deficits regarding speed and agility.
Speed and agility can be assessed in different ways, such as with a speedy test, quick feet test, shuttle run, the agility T-test (21) or different consecutive jump patterns (39). Of note, the assessment should include single leg as well as bipedal tests to properly screen for potential deficits (21). All of these tests have in common, that the subjects need to perform the task as fast as possible without losing control over the trunk. Thus, besides agility and speed, also coordination, balance, and concentration are required and tested.
Neuromuscular/postural control
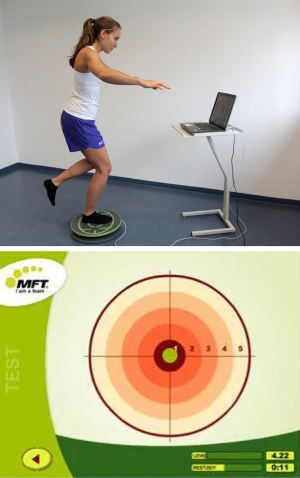
Decreased neuromuscular control of the knee, hip and trunk are associated with a higher ACL (re-) injury risk (40,41). Therefore, many ACL injury prevention programs include different screening tests to detect and correct such deficits. In a meta-analysis by Hewett et al., it has been shown, that such prevention programs can effectively reduce the injury risk (42). Of note, most of the screening tests for neuromuscular deficits are highly demanding and include two-dimensional or three-dimensional video analyses to evaluate joint angles during different task (such as step-down test or jumping tests). Therefore, their clinical applicability is questionable and simpler tests have been established to assess for postural control. Balance tests are easy and time efficient and are representative for hip, trunk, knee and ankle neuromuscular control and can therefore be used for functional assessment following ACL reconstruction (43). Different tests and devices exist. The Biodex Stability System (Biodex Medical Systems, Shirley, New York, USA) can assess dynamic postural stability in a closed-chain manner. The foot platform has different resistance levels and the subject is instructed to maintain the level position during a test (8). Another device to assess dynamic balance is the MFT Challenge Disc (TST Trendsport, Grosshöflein, Austria), which is connected to a laptop or personal computer. The disc is free to move and a software provides instant feedback regarding disc position while the subjects tries to maintain the balance on the disc (23). Alternatively to dynamic balance tests, postural control can also be assessed in a static manner, such as the participant is instructed to maintain the balance with open and closed eyes and the motion and excursion of the lower and upper body are registered (8).
Development of a new test battery
A new test battery (Back in Action, CoRehab, Trento, Italy) consisting of seven subtests has been developed and clinically established (22,23). The different subtests provide data on strength, jumping power, speed and agility as well as balance. The test battery can be accomplished within one hour and needs only little equipment and space and can therefore be performed in one room. A software program provides fast evaluation and feedback and compares the subjects´ performance with normative data from 434 participants (23). All data are evaluated using the absolute values as well as the limb symmetry index for one-legged tests. The results of the participants are classified from “very weak” to “very good” based on age and gender specific normative values. The test battery should be performed at least twice following ACL reconstruction or once if the participant meets the return to sport criteria (22).
Jump tests
The participants must perform a counter movement jump (one- and two-legged) as well as plyometric jumps. For the counter movement jump, the subjects are instructed to quickly bend their knees followed by an immediate upward jump. The arms have to be placed on the hips. For the plyometric jumps subjects must perform three consecutive bipedal jumps. In contrast to the counter movement jump, the arms can be used to assist with the jump. The outcome variables include maximum height (cm), power (W/kg), ground contact time (ms) and reactivity (mm/ms). All tests are performed using Myotest (Myotest SA, Sion, Switzerland).
Speed and agility
The participants must accomplish a jump coordination path (Speedy jump; one-legged) (Figure 1). The path includes forward, backward and sideway jumps and the subjects should be as fast as possible without a rest between the hurdles, touching the hurdles or twisting of the hip. The outcome variable is time in seconds.

For the Quick feet test (Figure 2), the same equipment same equipment is used as for the Speedy jump. The participant has to step in and out by alternating the foot without touching the poles or reversing the order of the steps. The time between the beginning and the point where 15 repetitions are completed is measured (seconds). One repetition is considered completed when the starting leg returns to its initial position.

Postural control
The tests are performed on a MFT Challenge Disc (TST Trendsport, Grosshöflein, Austria). A software program provides instant feedback about the disc position while the subject is balancing on the disc (either one- or two-legged). The participant is asked to maintain the balance for 30 seconds and the outcome variable is the level of stability index (Figure 3).
In addition to the Back in Action test battery (Back in Action, CoRehab, Trento, Italy), subjects complete isokinetic quadriceps and hamstring muscle strength tests.
Future perspective
The key for any functional testing is the comparison to normative data, or ideally to the pre-injury state (longitudinal design). For our test battery, age and gender specific normative data were obtained from 434 healthy subjects. However, to individualize the rehabilitation and return to sport criteria, sports specific normative data need to be obtained. Further, clinical studies investigating the effectiveness of such functional tests are needed.
Conclusions
Functional assessment following ACL reconstruction should be incorporated in the rehabilitation process. Individual tests are not sensitive enough to detect functional deficits, therefore test batteries including muscle strength, hop/jump tests, agility and neuromuscular control should be established. While prevention programs might reduce the ACL injury risk there is a lack of evidence whether functional assessment following ACL reconstruction can reduce the incidence of graft failures.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Freddie H. Fu and Jeremy M. Burnham) for the series “Trends in ACL Reconstruction” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.06.13). The series “Trends in ACL Reconstruction” was commissioned by the editorial office without any funding or sponsorship. CF reports personal fees from Medacta (Switzerland) and Karl Storz (Germany), outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Webster KE, Feller JA, Leigh WB, et al. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med 2014;42:641-7. [Crossref] [PubMed]
- Wright RW, Magnussen RA, Dunn WR, et al. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am 2011;93:1159-65. [Crossref] [PubMed]
- Webster KE, Feller JA. Exploring the High Reinjury Rate in Younger Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2016;44:2827-32. [Crossref] [PubMed]
- Alentorn-Geli E, Mendiguchia J, Samuelsson K, et al. Prevention of non-contact anterior cruciate ligament injuries in sports. Part II: systematic review of the effectiveness of prevention programmes in male athletes. Knee Surg Sports Traumatol Arthrosc 2014;22:16-25. [Crossref] [PubMed]
- Magnussen RA, Trojani C, Granan LP, et al. Patient demographics and surgical characteristics in ACL revision: a comparison of French, Norwegian, and North American cohorts. Knee Surg Sports Traumatol Arthrosc 2015;23:2339-48. [Crossref] [PubMed]
- Pauzenberger L, Syre S, Schurz M. "Ligamentization" in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy 2013;29:1712-21. [Crossref] [PubMed]
- Konrath JM, Vertullo CJ, Kennedy BA, et al. Morphologic Characteristics and Strength of the Hamstring Muscles Remain Altered at 2 Years After Use of a Hamstring Tendon Graft in Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2016;44:2589-98. [Crossref] [PubMed]
- Mattacola CG, Perrin DH, Gansneder BM, et al. Strength, Functional Outcome, and Postural Stability After Anterior Cruciate Ligament Reconstruction. J Athl Train 2002;37:262-8. [PubMed]
- Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2010;40:141-54. [Crossref] [PubMed]
- Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med 2004;34:269-80. [Crossref] [PubMed]
- Abrams GD, Harris JD, Gupta AK, et al. Functional Performance Testing After Anterior Cruciate Ligament Reconstruction: A Systematic Review. Orthop J Sports Med 2014;2:2325967113518305 [Crossref] [PubMed]
- Augustsson J, Thomee R, Karlsson J. Ability of a new hop test to determine functional deficits after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2004;12:350-6. [Crossref] [PubMed]
- Logerstedt D, Grindem H, Lynch A, et al. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med 2012;40:2348-56. [Crossref] [PubMed]
- Reid A, Birmingham TB, Stratford PW, et al. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther 2007;87:337-49. [Crossref] [PubMed]
- Narducci E, Waltz A, Gorski K, et al. The clinical utility of functional performance tests within one-year post-acl reconstruction: a systematic review. Int J Sports Phys Ther 2011;6:333-42. [PubMed]
- Ageberg E, Thomee R, Neeter C, et al. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two to five-year followup. Arthritis Rheum 2008;59:1773-9. [Crossref] [PubMed]
- Ardern CL, Webster KE, Taylor NF, et al. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med 2011;45:596-606. [Crossref] [PubMed]
- Neeter C, Gustavsson A, Thomee P, et al. Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Knee Surg Sports Traumatol Arthrosc 2006;14:571-80. [Crossref] [PubMed]
- Björklund K, Sköld C, Andersson L, et al. Reliability of a criterion-based test of athletes with knee injuries; where the physiotherapist and the patient independently and simultaneously assess the patient's performance. Knee Surg Sports Traumatol Arthrosc 2006;14:165-75. [Crossref] [PubMed]
- Björklund K, Andersson L, Dalén N. Validity and responsiveness of the test of athletes with knee injuries: the new criterion based functional performance test instrument. Knee Surg Sports Traumatol Arthrosc 2009;17:435-45. [Crossref] [PubMed]
- Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther 2011;41:377-87. [Crossref] [PubMed]
- Herbst E, Hoser C, Hildebrandt C, et al. Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part II: clinical application of a new test battery. Knee Surg Sports Traumatol Arthrosc 2015;23:1283-91. [Crossref] [PubMed]
- Hildebrandt C, Muller L, Zisch B, et al. Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part I: development of a new test battery. Knee Surg Sports Traumatol Arthrosc 2015;23:1273-81. [Crossref] [PubMed]
- Zwolski C, Schmitt LC, Thomas S, et al. The Utility of Limb Symmetry Indices in Return-to-Sport Assessment in Patients With Bilateral Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2016;44:2030-8. [Crossref] [PubMed]
- Arilla FV, Rahnemai-Azar AA, Yacuzzi C, et al. Correlation between a 2D simple image analysis method and 3D bony motion during the pivot shift test. Knee 2016;23:1059-63. [Crossref] [PubMed]
- Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med 2008;27:405-24. vii-ix. [Crossref] [PubMed]
- Xergia SA, McClelland JA, Kvist J, et al. The influence of graft choice on isokinetic muscle strength 4-24 months after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2011;19:768-80. [Crossref] [PubMed]
- Lautamies R, Harilainen A, Kettunen J, et al. Isokinetic quadriceps and hamstring muscle strength and knee function 5 years after anterior cruciate ligament reconstruction: comparison between bone-patellar tendon-bone and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc 2008;16:1009-16. [Crossref] [PubMed]
- Kannus P. Isokinetic evaluation of muscular performance: implications for muscle testing and rehabilitation. Int J Sports Med 1994;15:S11-8. [Crossref] [PubMed]
- Kim HJ, Lee JH, Ahn SE, et al. Influence of Anterior Cruciate Ligament Tear on Thigh Muscle Strength and Hamstring-to-Quadriceps Ratio: A Meta-Analysis. PLoS One 2016;11:e0146234 [Crossref] [PubMed]
- Kyritsis P, Bahr R, Landreau P, et al. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med 2016;50:946-51. [Crossref] [PubMed]
- Burnham JM, Yonz MC, Robertson KE, et al. Relationship of Hip and Trunk Muscle Function with Single Leg Step-Down Performance: Implications for Return to Play Screening and Rehabilitation. Phys Ther Sport 2016;22:66-73. [Crossref] [PubMed]
- Khayambashi K, Ghoddosi N, Straub RK, et al. Hip Muscle Strength Predicts Noncontact Anterior Cruciate Ligament Injury in Male and Female Athletes: A Prospective Study. Am J Sports Med 2016;44:355-61. [Crossref] [PubMed]
- Gustavsson A, Neeter C, Thomeé P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2006;14:778-88. [Crossref] [PubMed]
- Xergia SA, Pappas E, Zampeli F, et al. Asymmetries in functional hop tests, lower extremity kinematics, and isokinetic strength persist 6 to 9 months following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2013;43:154-62. [Crossref] [PubMed]
- Carlson VR, Sheehan FT, Boden BP. Video Analysis of Anterior Cruciate Ligament (ACL) Injuries: A Systematic Review. JBJS Rev 2016;4: [Crossref] [PubMed]
- Petschnig R, Baron R, Albrecht M. The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 1998;28:23-31. [Crossref] [PubMed]
- Silvers HJ, Mandelbaum BR. Prevention of anterior cruciate ligament injury in the female athlete. Br J Sports Med 2007;41:i52-9. [Crossref] [PubMed]
- Keays SL, Bullock-Saxton J, Keays AC. Strength and function before and after anterior cruciate ligament reconstruction. Clin Orthop Relat Res 2000;174-83. [Crossref] [PubMed]
- Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 2010;38:1968-78. [Crossref] [PubMed]
- Zazulak BT, Hewett TE, Reeves NP, et al. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med 2007;35:368-73. [Crossref] [PubMed]
- Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: Part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med 2006;34:490-8. [Crossref] [PubMed]
- Zouita Ben Moussa A, Zouita S, Dziri C, et al. Single-leg assessment of postural stability and knee functional outcome two years after anterior cruciate ligament reconstruction. Ann Phys Rehabil Med 2009;52:475-84. [Crossref] [PubMed]
Cite this article as: Herbst E, Wierer G, Fischer F, Gföller P, Hoser C, Fink C. Functional assessments for anterior cruciate ligament reconstruction return to sport. Ann Joint 2017;2:37.


