Outcome after treatment of Vancouver B2 peri-prosthetic femoral fractures: revision arthroplasty and compression cerclage system fixation
Introduction
As the functional results after total hip arthroplasty (THA) improved and daily activities increased, the number of patients with joint arthroplasty is rising year by year. Due to low/high energy trauma and osteoporotic bones, the incidence of peri-prosthetic femur fractures has been gradually increasing all over the world. The incidence reported is 0.1% to 2.1% in THA and rises with the continual increase in hip arthroplasty performed (1). Peri-prosthetic fractures (PPF) may be associated with poor bone stock, trauma, advanced age, and potential prosthetic instability. These fractures are challenging for limited fracture fixation options both proximally and distally. In addition, patients experiencing inter-prosthetic fractures are generally older and suffer from osteoporotic bone, which further increases the difficulty of providing effective treatment. Fractures are typically classified and managed according to the Vancouver classification system (2). Overall, the incidence of interprosthetic fractures is rare (3-5). Femur fractures between ipsilateral hip and knee prostheses have less bone available for fracture fixation secondary to the presence of hardware both proximal and distal to the fracture. The Vancouver classification, focusing on implant stability, bone stock, and fracture fixation, is an effective guide for the treatment of peri-prosthetic hip fractures (2). However, the medical literature has little information providing recommendations for the appropriate treatment of interprosthetic femoral fractures. The purpose of this report was to describe our experience with the treatment of interprosthetic femoral fractures and emphasize treatment principles and specific intraoperative management.
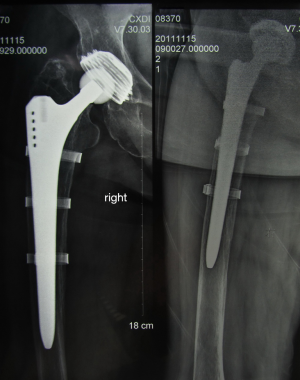
Vancouver type B2 fractures are those occurring at the tip of the THA stem in which the hip implant is loose (as opposed to type B1, hip implant is stable and B3 hip implant is loose and there is loss of bone), and are considered the most complex to manage (Figure 1) (2). Surgical management is usually recommended with the goal being to preserve implant survival and achieve successful union; however, the most appropriate treatment is a matter of debate.
To date, lots of strategies for Vancouver B2 fracture were reported with debating outcomes. A retrospective study was conducted to analyze the outcome of revision arthroplasty and compression cerclage system (CCS) fixation.
Methods
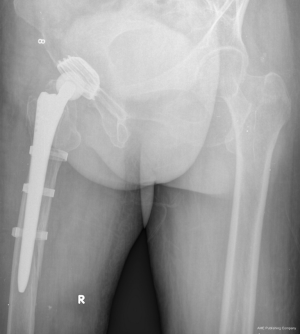
All the patients eligible had sustained a PFF with loose implant after hip arthroplasty treated at our institution between 2002 and 2013. The study was approved by the ethical committee of the Medical School of Nanjing University, and informed consent was obtained from patients. Patients were treated by revision arthroplasty and open reduction internal fixation (ORIF) via CCS (Figure 2). For assessment of functional outcome and follow-up visits only patients that gave informed consent and had adequate cognitive ability to participate were included; thus, deceased patients and patients suffering from dementia were excluded. Types of PPF were confirmed by both radiographic finding and loosen prosthesis during the operation.
CCS system
The CCS from Smith & Nephew was primarily developed for conical bones, notably the proximal and distal ends of the femur. The rough blasted surface has a mean roughness of 3–5 μm which supports osteointe gration of the band. With a length of 27 cm, the CCS cerclage is long enough to go around the greater trochanter as well as thinner bones. The continuous adjustability allows application for all diameters of long bones which contributes to a substantial simplification of inventory. A cementless prosthesis is to be replaced by an SLR-PLUS™ stem and a BICON-PLUS™ cup. CCS bands are fitted to protect the bone from splitting; cerclage of greater trochanter and closure of the fenestration.
After surgery, same rehabilitation procedures were performed. Angiography was conducted 3 days post operation. Demographic data, surgical related data and HSS score were recorded for all the patients.
Results
Due to low energy trauma, of all the 14 female patients with mean age at 67.6 years old (from 61 to 84 years old) were type B2 Vancouver PPF. BMI of the patients were from 18.7 to 27.6 (mean BMI was 22.4). Outcomes following treatment were at a mean follow-up of 5.2 years. The mean HHS was 37.4 and 83.0 pre- and post-operation. HHS was recorded for all patients available for follow-up; all the patients had bony union at 6.5 months (Figure 3). The mean duration of the surgeries was 83.6 minutes.
No dislocation, non-union, and deep vein thrombosis were detected.
Discussion
Strategy treatment algorithms for PPF were controversial. Based on Vancouver classification, treatment of isolated PPF of the femur should depend on fracture location, implant stability, and quality of the surrounding bone stock. These concepts are applied to our treatment of PPF. For Vancouver B2 PPF, long stemmed revision was suggested with good clinical outcome. Bone quality around the fracture site and prosthesis is also critical for decision making. The results of this study demonstrated successful fracture union in those patients selected for long stemmed revision and CCS system, supporting the efficacy of these treatment principles.
As the band fastener is rotatable the band can be shaped to fit conical bones shape with minimal surface compression. Revision hip arthroplasty for loosening is becoming an ever-increasing part of the orthopedic surgeons’ practice. These devices obtain fixation by osseous integration into the host bone. The use of non-cemented implants at revision surgery seemed a natural progression; however, all too often negative trade offs had to be accepted. Compare to the plating, CCS had several advantages, like anti-rotation, easy to conduct, less invasive and unnecessary to expose the tip of fracture et al.
The non-cemented revision devices previously available were suitable only for very straightforward or for very difficult cases. Now, at long last, there is a system to suit the middle range of hip revision arthroplasty: the SLR-PLUS revision stem can be used to manage many of the revision patients. The new geometry of the SLR-PLUS stem makes use, above all, of the sound distal bone stock to obtain implant fixation. Together with the new design (with stem lengths to suit the revision situation), this feature makes for immediate stable fixation. Secondary fixation through osseo-integration and, hence, long-term clinical success is brought about by the use of a forged titanium-niobium alloy component with surface roughness that has stood the test of time.
Conclusions
Long stemmed revision with CCS system has a good clinical outcome for type B2 PPF.
Acknowledgments
Funding: This work was funded by National Nature Science Foundation of China (81101338 and 81125013) (to DQ Shi and Q Jiang).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2016.03.01). DQS serves as an unpaid Executive Editor-in-Chief of Annals of Joint from Mar 2016 to Feb 2021. QJ serves as an Editor-in-Chief of Annals of Joint from Mar 2016 to Feb 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethical committee of the Medical School of Nanjing University, and informed consent was obtained from patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am 1999;30:183-90. [Crossref] [PubMed]
- Parvizi J, Rapuri VR, Purtill JJ, et al. Treatment protocol for proximal femoral periprosthetic fractures. J Bone Joint Surg Am 2004;86-A:8-16. [PubMed]
- Kenny P, Rice J, Quinlan W. Interprosthetic fracture of the femoral shaft. J Arthroplasty 1998;13:361-4. [Crossref] [PubMed]
- Fink B, Fuerst M, Singer J. Periprosthetic fractures of the femur associated with hip arthroplasty. Arch Orthop Trauma Surg 2005;125:433-42. [Crossref] [PubMed]
- Ricci WM, Loftus T, Cox C, et al. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma 2006;20:190-6. [Crossref] [PubMed]
Cite this article as: Shi DQ, Xu ZH, Xu XQ, Chen DY, Yuan T, Weng WJ, Xiong J, Jiang Q. Outcome after treatment of Vancouver B2 peri-prosthetic femoral fractures: revision arthroplasty and compression cerclage system fixation. Ann Joint 2016;1:2.