Association of knee range of motion and continuous passive motion following total knee arthroplasty: a meta-analysis
Introduction
Arthroplasty is an orthopedic surgery done to restore the integrity and function of a joint, which can be restored by resurfacing the bones or be replaced by an artificial joint (1-3). Total knee arthroplasty (TKA) is considered a clinically effective intervention in recent years with high rates of success in treatment of chronic knee pain and disability (4,5). Due to knee stiffness after TKA, rehabilitation therapy plays an important role during the following treatments, which often includes continuous passive motion (CPM) (6).
In 1926, Von Riemke firstly stated that movement should be conducted slowly and continuously from the first day after surgery (7). Then, Salter invented the concept of CPM based on a series of experiments and theories (8). CPM is a way to provide regular movement by a machine (7), and is usually identified to increase knee range of motion (ROM) (9). Hill et al. conducted a study to determine the effects of a CPM device on knee ROM after operation of intra-articular fractures around knee on 40 patients within 48 hours after surgery. They found that range of knee flexion was significant greater at 48 hour in CPM group than in non-CPM group (10). Moreover, CPM was also considered to decrease narcotic analgesics uses, to reduce the length of hospital stay (11) and to improve muscle strength (12). However, a randomized, controlled trial (including 160 patients) of CPM following TKA showed that CPM provided no benefit to patients recovering from TKA (13). Since CPM had a lot of uncertainties about the treatment effects after TKA, it is necessary to determine the effectiveness of CPM. Although many studies had been performed to evaluate the effectiveness of CPM following TKA, the results of these studies always seem inconsistent and inconclusive because of small sample size and uncertainties of the research subjects (14). Thus a meta-analysis is needed to integrate these data to better evaluate the therapeutic effect of CPM following TKA.
In present review, a series of randomized controlled trials (RCTs) were retrieved to determine the association between CPM and ROM (including both active knee flexion and active knee extension) following TKA before May 2014 and a meta-analysis was performed to evaluate the effectiveness of CPM following TKA.
Materials and methods
Literature search
Under the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement (15), a searching strategy was developed for present meta-analysis. Publications related to CPM and TKA were retrieved by searching the electronic databases of PubMed, Cochrane library and Excerpt Medical Database (EMBASE) up to May 2014. The search was based on combinations of the following items: continuous passive motion (or CPM), total knee arthroplasty, range of motion and range of movement.
Inclusion and exclusion criteria
Two investigators reviewed titles and abstracts matching the inclusion criteria independently. The inclusion criteria were as follows: (I) RCTs about the impact of CPM on ROM following TKA; (II) indexes such as active knee flexion ROM and active knee extension ROM; (III) papers including corresponding mean value and standard deviation; (IV) control groups treated by non-CPM measures (conventional measures such as motion, standard physical therapy and fixation). Studies were excluded if one of the following existed: (I) studies such as reviews, meeting summaries, case reports and comments; (II) studies only had mean value without corresponding standard deviation; (III) studies with repeated reporting articles and unclear described data; (IV) non-English literatures.
Data extraction
Data extraction was performed independently by two reviewers from all eligible studies according to the criteria listed above. Any disagreements were resolved by discussion with a third person. For each selected article in present study, the following characteristics were collected: the first author, year of publication, sample size, mean and standard deviation of active knee flexion in CPM group and non-CPM group respectively, mean and standard deviation of active knee extension in CPM group and non-CPM group respectively, and non-CPM treatments used in control groups.
Quality assessment
The Jadad scoring system was used to evaluate the quality of studies included in this meta-analysis (16). Jadad scores are based on the description of randomization (maximum score: 2 points), double blinding (maximum score: 2 points), and withdrawals and dropouts (maximum score: 1 points) and can range from 0 to 5 points. Higher score of Jadad indicates better methodological quality.
Statistical analysis
The statistical analysis was conducted using Stata 12.0 statistical software package. The effect sizes of continuous outcomes were measured as standardized mean differences (SMD) with 95% confidence intervals (CIs). A random-effect model was used to calculate the pooled SMD. Heterogeneity was examined by using the I2 statistic (17) and P value <0.1 or I2 >50% was considered heterogeneous. Subgroup analyses were performed between CPM group and standard physiotherapy group. Results which cannot perform the meta-analysis were narrated descriptively. Finally, publication bias was assessed using the weighted regression tests described by Egger et al. (18). P<0.05 was considered statistically significant.
Results
Characteristics of selected literatures
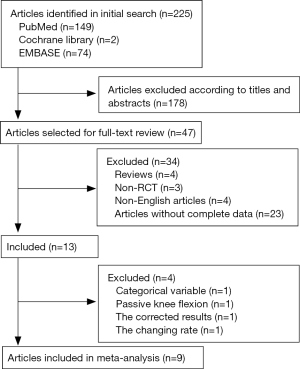
A total of 225 articles were searched according to the key words, including 149 articles in PubMed, two articles in Cochrane library, and 74 articles in EMBASE. The titles and abstracts of these 225 articles were studied and 47 articles were selected for further analysis. Based on the full texts of the 47 articles, 13 articles were finally chosen, excluding four reviews, 23 articles without complete data, three non-RCTs, and four non-English articles. Among all the 13 articles, Davies’s study (19) was removed because its outcome was a categorical variable; Chen’s study (20) was removed because the outcome was based on passive knee flexion; Ritter’s study (21) was removed because its results were corrected by repeated measures; Chiarello’s study (22) was removed because the indexes used in this article were the change rate of ROM before and after the intervention (Figure 1). Finally, nine studies providing mean and standard deviation of active knee flexion and active knee extension respectively were included in this systematic review (23-31).
Table 1 summed up the characteristics of the selected literatures which were all RCTs from 1997 to 2014. The number of patients ranged from 53 to 210. Measurements of control groups were various. Among all the nine articles, five used standard physiotherapy (23-25,29,30); one used standard exercise (26); one used immobilization (28); one used active exercise (31); and one integrated immobilization and standard exercise (27).

Full table
The influence of CPM on active knee flexion at different time following TKA
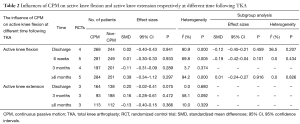
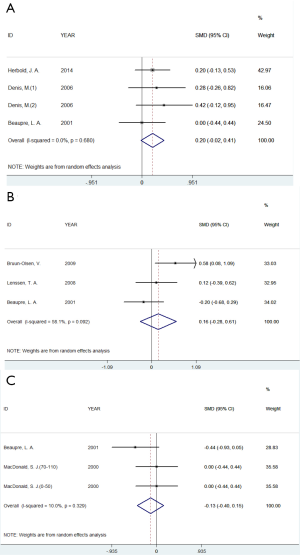
Meta-analysis was performed to examine the association between CPM and active knee flexion ROM at different time following TKA (Table 2). For the outcomes of active knee flexion, there were no significant differences observed between CPM group and non-CPM group (including standard physiotherapy, standard exercise, immobilization, and active exercise) at the time of discharge from hospital (SMD =0.02, 95% CI: −0.40 to 0.43, P=0.941), 6 weeks (SMD =0.01, 95% CI: −0.30 to 0.33, P=0.933), 3 months (SMD =−0.11, 95% CI: −0.31 to 0.09, P=0.289), and more than 6 months (SMD =0.39, 95% CI: −0.34 to 1.12, P=0.297) respectively (Figure 2). Besides, statistically significant heterogeneity was observed at discharge (I2 =80.9%, P=0.000, Figure 2A), 6 weeks after discharge (I2 =69.8%, P=0.005, Figure 2B), and more than 6 months after discharge (I2 =94.2%, P=0.000, Figure 2D), respectively. After subgroup analyses performed between CPM group and standard physiotherapy group (23-25,29,30), no heterogeneity was observed in the 3 times mentioned above respectively (Table 2, Figures 2E-G).
Full table

The influence of CPM on active knee extension at different time following TKA
For the outcomes of active knee extension, no significant differences were observed between CPM group and non-CPM group at the time of discharge from hospital (SMD =0.20, 95% CI: −0.02 to 0.41, P=0.075), 3 months (SMD =−0.13, 95% CI: −0.40 to 0.15, P=0.366), and more than 6 months (SMD =−0.13, 95% CI: −0.40 to 0.15, P=0.366) respectively. Meanwhile, heterogeneity also had no statistical differences at the 3 times respectively (Figure 3). The detailed information was shown in Table 2.
Publication bias
For both active knee flexion and active knee extension, there were no significant differences between CPM group and non-CPM group at time of discharge from hospital, 6 weeks, and 3 months respectively (active knee flexion: P=0.436 for discharge, P=0.107 for 6 weeks after discharge, and P=0.861 for 3 months after discharge. Active knee extension: P=0.599 for discharge and P=0.438 for 3 months after discharge). However, the analyses of active knee flexion at 6 months after discharge showed publication bias (P=0.015), and no significance was observed after subgroup analysis (P=0.582).
Discussion
In present meta-analysis, a total of nine studies were included. For both active knee flexion ROM and active knee extension ROM, there were no significant differences between CPM group and non-CPM group at the time of discharge from hospital, 6 weeks, 3 months, and more than 6 months respectively. Thus it was concluded that CPM had no significant effects on active knee flexion and active knee extension of patients undergoing TKA, and the effectiveness was not changed by the therapy time (short-term or long-term).
Some other systematic reviews have been reported in previous studies. For example, Brosseau et al. conducted a meta-analysis to examine the effectiveness of CPM following TKA (14 studies containing 952 patients). Their results showed significant improvements in active knee flexion with the combined use of CPM and physiotherapy compared to physiotherapy alone. Meanwhile, length of hospital stay and time for knee manipulations were significant decreased in CPM group compared with those in physiotherapy group (32). Similarly, a meta-analysis by Lenssen et al. (including 15 articles) demonstrated that CPM, combining with standardized physical therapy after TKA, showed moderate, positive and short-term effects on postoperative recovery, but no relevant long-term effects (33). Du Plessis et al. performed a meta-analysis combining three RCTs and revealed that CPM can improve shoulder ROM (12). However, present analyses demonstrated that CPM had no effects on active knee flexion ROM and active knee extension ROM compared with the non-CPM therapy. Harvey et al. got the similar conclusion that the effects of CPM on knee ROM were too small to justify its use (20 RCTs containing 1,335 participants) (34). Because rehabilitation therapy following TKA was associated with various factors, many factors should be taken into account comprehensively to evaluate the effectiveness of CPM. In present review, only active knee flexion and active knee extension were performed meta-analysis, other indexes such as bleeding volume (35), degree of pain (36), swollen degree (37) and venous thrombus (38) were not included. Thus to be better understand the effectiveness of CPM following TKA, further studies should be proposed by integrating all the related indicators.
Some limitations should be discussed in present meta-analysis. Language, publication and the CPM machine were considered the majority biases in this study. First, only literatures published English were included. Second, fewer articles about negative results were published due to researchers, subsidized unit and publishers. Third, the differences of CPM machines used in various studies may contribute to biases in this study. Additionally, significant heterogeneity was detected in analyses of active knee flexion at time of discharge from hospital, 6 weeks and more than 6 months, which caused by different measurements of the control groups. Thus subgroup analyses were conducted between CPM-treated group and normal standard physiotherapy-treated group and the results were the same as the overall analyses.
Conclusions
In present study, a meta-analysis was conducted to determine the association between CPM and ROM after TKA. Through establishing strict inclusion and exclusion criteria, outcomes of active knee flexion ROM and active knee extension ROM between CPM-treated patients and non-CPM treated patients were summarized to obtain more scientific and accurate results. The results showed that CPM had little effects on the recovery after TKA in terms of active knee flexion and active knee extension ROM. Given the limitation of our study, further analyses should be conducted to determine the effects of CPM following TKA by integrating other related indexes.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2016.04.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lavigne MJ, Sanchez AA, Coutts RD. Recurrent dislocation after total hip arthroplasty: treatment with an Achilles tendon allograft. J Arthroplasty 2001;16:13-8. [Crossref] [PubMed]
- Lygre SH, Espehaug B, Havelin LI, et al. Failure of total knee arthroplasty with or without patella resurfacing. A study from the Norwegian Arthroplasty Register with 0-15 years of follow-up. Acta Orthop 2011;82:282-92. [Crossref] [PubMed]
- Jennings LM, Al-Hajjar M, Brockett CL, et al. (iv) Enhancing the safety and reliability of joint replacement implants. Orthop Trauma 2012;26:246-252. [Crossref] [PubMed]
- Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 2010;468:45-51. [Crossref] [PubMed]
- Wylde V, Dieppe P, Hewlett S, et al. Total knee replacement: is it really an effective procedure for all? Knee 2007;14:417-23. [Crossref] [PubMed]
- Roos EM. Effectiveness and practice variation of rehabilitation after joint replacement. Curr Opin Rheumatol 2003;15:160-2. [Crossref] [PubMed]
- O'Driscoll SW, Giori NJ. Continuous passive motion (CPM): theory and principles of clinical application. J Rehabil Res Dev 2000;37:179-88. [PubMed]
- Salter RB. The biologic concept of continuous passive motion of synovial joints. The first 18 years of basic research and its clinical application. Clin Orthop Relat Res 1989;12-25. [PubMed]
- Walsh M, Woodhouse LJ, Thomas SG, et al. Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Ther 1998;78:248-58. [PubMed]
- Hill AD, Palmer MJ, Tanner SL, et al. Use of Continuous Passive Motion in the Postoperative Treatment of Intra-Articular Knee Fractures. J Bone Joint Surg Am 2014;96:e118 [Crossref] [PubMed]
- Colwell CW Jr, Morris BA. The influence of continuous passive motion on the results of total knee arthroplasty. Clin Orthop Relat Res 1992;225-8. [PubMed]
- Du Plessis M, Eksteen E, Jenneker A, et al. The effectiveness of continuous passive motion on range of motion, pain and muscle strength following rotator cuff repair: a systematic review. Clin Rehabil 2011;25:291-302. [Crossref] [PubMed]
- Boese CK, Weis M, Phillips T, et al. The efficacy of continuous passive motion after total knee arthroplasty: a comparison of three protocols. J Arthroplasty 2014;29:1158-62. [Crossref] [PubMed]
- Zintzaras E, Ioannidis JP. Heterogeneity testing in meta-analysis of genome searches. Genet Epidemiol 2005;28:123-37. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264-9, W64.
- Halpern SH, Douglas MJ, editors. Evidence-based obstetric anesthesia. John Wiley & Sons, 2008.
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [Crossref] [PubMed]
- Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [Crossref] [PubMed]
- Davies DM, Johnston DW, Beaupre LA, et al. Effect of adjunctive range-of-motion therapy after primary total knee arthroplasty on the use of health services after hospital discharge. Can J Surg 2003;46:30-6. [PubMed]
- Chen B, Zimmerman JR, Soulen L, et al. Continuous passive motion after total knee arthroplasty: a prospective study. Am J Phys Med Rehabil 2000;79:421-6. [Crossref] [PubMed]
- Ritter MA, Gandolf VS, Holston KS. Continuous passive motion versus physical therapy in total knee arthroplasty. Clin Orthop Relat Res 1989;239-43. [PubMed]
- Chiarello CM, Gundersen L, O'Halloran T. The effect of continuous passive motion duration and increment on range of motion in total knee arthroplasty patients. J Orthop Sports Phys Ther 1997;25:119-27. [Crossref] [PubMed]
- Lenssen TA, van Steyn MJ, Crijns YH, et al. Effectiveness of prolonged use of continuous passive motion (CPM), as an adjunct to physiotherapy, after total knee arthroplasty. BMC Musculoskelet Disord 2008;9:60. [Crossref] [PubMed]
- Herbold JA, Bonistall K, Blackburn M, et al. Randomized controlled trial of the effectiveness of continuous passive motion after total knee replacement. Arch Phys Med Rehabil 2014;95:1240-5. [Crossref] [PubMed]
- Denis M, Moffet H, Caron F, et al. Effectiveness of continuous passive motion and conventional physical therapy after total knee arthroplasty: a randomized clinical trial. Phys Ther 2006;86:174-85. [PubMed]
- Beaupré LA, Davies DM, Jones CA, et al. Exercise combined with continuous passive motion or slider board therapy compared with exercise only: a randomized controlled trial of patients following total knee arthroplasty. Phys Ther 2001;81:1029-37. [PubMed]
- Lau SK, Chiu KY. Use of continuous passive motion after total knee arthroplasty. J Arthroplasty 2001;16:336-9. [Crossref] [PubMed]
- Yashar AA, Venn-Watson E, Welsh T, et al. Continuous passive motion with accelerated flexion after total knee arthroplasty. Clin Orthop Relat Res 1997;38-43. [PubMed]
- MacDonald SJ, Bourne RB, Rorabeck CH, et al. Prospective randomized clinical trial of continuous passive motion after total knee arthroplasty. Clin Orthop Relat Res 2000;30-5. [Crossref] [PubMed]
- Worland RL, Arredondo J, Angles F, et al. Home continuous passive motion machine versus professional physical therapy following total knee replacement. J Arthroplasty 1998;13:784-7. [Crossref] [PubMed]
- Bruun-Olsen V, Heiberg KE, Mengshoel AM. Continuous passive motion as an adjunct to active exercises in early rehabilitation following total knee arthroplasty - a randomized controlled trial. Disabil Rehabil 2009;31:277-83. [Crossref] [PubMed]
- Brosseau L, Milne S, Wells G, et al. Efficacy of continuous passive motion following total knee arthroplasty: a metaanalysis. J Rheumatol 2004;31:2251-64. [PubMed]
- Lenssen AF, Koke AJ, De Bie RA, et al. Continuous passive motion following primary total knee arthroplasty: short- and long-term effects on range of motion. Physical Therapy Reviews 2003;8:113-21. [Crossref]
- Harvey LA, Brosseau L, Herbert RD. Continuous passive motion following total knee arthroplasty in people with arthritis. Cochrane Database Syst Rev 2010;CD004260 [PubMed]
- Pope RO, Corcoran S, McCaul K, et al. Continuous passive motion after primary total knee arthroplasty. Does it offer any benefits? J Bone Joint Surg Br 1997;79:914-7. [Crossref] [PubMed]
- Reinecke SM, Hazard RG, Coleman K. Continuous passive motion in seating: a new strategy against low back pain. J Spinal Disord 1994;7:29-35. [Crossref] [PubMed]
- Ververeli PA, Sutton DC, Hearn SL, et al. Continuous passive motion after total knee arthroplasty. Analysis of cost and benefits. Clin Orthop Relat Res 1995;208-15. [PubMed]
- He ML, Xiao ZM, Lei M, et al. Continuous passive motion for preventing venous thromboembolism after total knee arthroplasty. Cochrane Database Syst Rev 2014;7:CD008207 [PubMed]
Cite this article as: Wu J, Lv M, Zhou Y. Association of knee range of motion and continuous passive motion following total knee arthroplasty: a meta-analysis. Ann Joint 2016;1:5.