
Individual anatomical risk factors for patellar instability
Over the last two decades the management of patellofemoral instability has changed with the advent of the ability to define the variation in the anatomy of the patellofemoral joint and to put a number onto that variation. From this we are able to agree what is “normal” and what is pathological. The review by Dietrich et al. (1) looks at the key method for doing this, namely imaging. The problem with the patellofemoral joint is that there is little consensus internationally on terminology, details of the history, the relevant examination techniques (which to do, how to do them, and how to report them) (2), but there is consensus on which are the important anatomical abnormalities, how to image and what to measure (1,3). As a consequence there is a better understanding about the surgical interventions needed to correct the abnormalities, although not necessarily which patients require an operation and the timing of it (4).
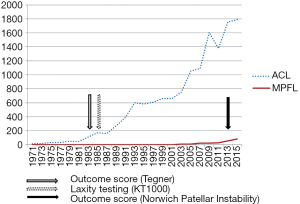
If reconstruction of the medial patellofemoral ligament (MPFL) is taken as an example, then the current evidence base is about 30 years behind that for the anterior cruciate ligament (ACL). The key drivers to research on the ACL were the development of the KT-1000 so that the amount of displacement due to a rupture could be measured consistently, and the development of a valid outcome measure (the Tegner activity level) so that treatments could be compared across multiple centers (Figure 1). There is no clinical measurement tool for mechanical instability of the patella. Attempts have been undertaken but the problem is the degree of displacement e.g., the mediolateral glide of the patella, varies from patient to patient and includes whether they have constitutional ligament laxity and age. We know that there is poor inter-observer agreement for clinical examination and that qualitative descriptions e.g., “normal” or “abnormal” correlate reasonably well, whereas the clinicians’ opinion on the amount of displacement (as measured by the width of the patella) does not. Recently there have been two patient reported outcomes measures for patellar instability, the Norwich Patellar Instability score, a 17-item instrument that list various activities, where only those activities actually undertaken are included in the measurement e.g., cutting and running when playing sports (5). The final score is calculated as a percentage; 0% being perfectly stable and 100% the worst score. The NPI score is now validated (6). Another score is nearing completion of its validation, the Banff Patella Instability Instrument (BPII) (7). This is a 31-item questionnaire with five sections covering “symptoms and physical complaints”, “work related concerns”, “sport/recreation/competition”, “lifestyle” and “social & emotional”. Therefore there are available patient reported outcome measures for patellofemoral instability that should result in more meaningful studies being reported in the future.
The paper by Dietrich et al. (1) covers well the anatomical abnormalities that can affect the stability of the patellofemoral joint. Henri Dejour described four main ones; patellar height (PH), type of trochlear dysplasia, patellar tilt angle (PTA), and tibial tubercle to trochlear groove (TTTG) distance (8). Prior to his work, the dominant operative strategy for stabilizing the patella (certainly in the UK) was lateral release, medial reefing, and Roux-Goldthwaite medialization of the insertion of the patellar ligament (or medialization of the tibial tubercle). Neither the assessment of the patient’s anatomical abnormalities, nor the actual technical details of the operation produced numbers that could be used for comparative data, quality assurance, or statistical analysis. Henri Dejour’s system provided numbers and so one was able to assess the degree of abnormality, have an operative plan to correct it, and then check how good a correction had been achieved, and whether this correlated with a successful outcome. It is still the basis for decision making in the techniques to be used when considering stabilising the extensor mechanism of the knee operatively.
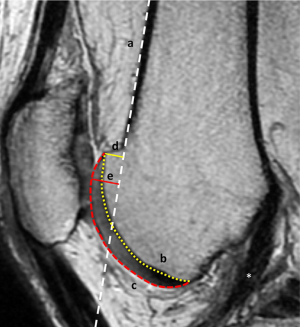
Henri Dejour’s other contribution was to stress that patellar instability involves both sides of the patellofemoral joint; the extensor mechanism and the trochlear groove (9). It is clear that the term “patellar instability” implies that there is a “problem” with the patella. However it should be considered as the marker within the whole extensor mechanism that describes the soft tissue envelope. If the patella is too high then the patellar ligament is overlong. If it is tilted and lying laterally, the MPFL is stretched. If it tracks laterally then the trochlea is dysplastic. The importance of trochlear dysplasia as a major factor in patellar instability is now well recognized. Controversy still exists on whether correction of the dysplasia should be directly with a trochleoplasty, or indirectly with an anteromedialization of the tibial tubercle. It is fair to say that European surgeons favor the direct approach whereas in North America this is not generally accepted. Being European my view is that in significant trochlear dysplasia it is not logical to try and balance a tennis ball on a soccer ball. This begs the question, how do you define significant trochlear dysplasia? Using Henri Dejour’s son David’s classification it is Type B or D where there is a supratrochlear spur (10). I have preferred to call this the trochlear boss (11). Henri Dejour defined this by the boss height in a complex calculation. I prefer to simplify the method of measurement as a distance between the perpendicular of the maximum anterior position of the trochlear groove relative to the line of the anterior femoral cortex. A significant trochlear dysplasia is present when the trochlear boss height (TBH) measures more than 4 mm in the presence of a type B, C or D dysplasia. Even this figure needs to consider the height of the patient. The boss height is measured from the lateral plain radiograph. We have correlated this with the MRI scan where it is measured from the mid-sagittal cut where the ACL is visible (12). Since this is a two-dimensional image of a three-dimensional problem the MRI scan can measure both the subchondral and chondral heights but may not be at the maximum anterior displacement which is usually laterally (Figure 2). The logic of the mid-sagittal cut is that this is where the normal groove should lie and, when followed proximally, run smoothly and directly into the anterior femoral cortex. The MRI TBH for subchondral bone is less than when measured from plain lateral radiograph (mean 3 mm instead of 4 mm) but it also gives the cartilaginous TBH (mean 5 mm) as well as information about the soft tissues and three-dimensional anatomy not available on plain film.
Although I stated earlier that the patella is not the problem in the majority of patients with patellar instability, abnormalities of shape may be a factor. The shape of the posterior surface of the patella usually matches the shape of the trochlea. This means that the more significant the trochlear dysplasia the more abnormal the patella shape should be. Patella types are well known from Wiberg’s work (13). Recently an abnormality associated with patellar instability is the inferomedial patellar protuberance (IPP) which may be a healed avulsion of the origin of the medial patellotibial ligament (14). Interestingly it was also noted that the medial ossicle seen on skyline views in patellar instability tends to be inferior and not related to the MPFL whose origin is in the upper medial half of the patella. The importance of the IPP is that it may create an incongruency between the patella and the dysplastic trochlea which as the patella engages the groove at around 20 to 30 degrees flexion there is a sudden movement associated with a clunk which is obvious clinically. The smooth engagement of the patella into the new groove when performing a trochleoplasty may require the patella to be re-shaped; obtaining patellofemoral congruency is a key component of trochleoplasty.
Finally there are important factors associated with a successful outcome in the management of patients with patellar instability that are not radiographic. The most important is the presence of hypermobility, usually assessed using the Beighton score (15). Few papers report the score within the cohort, yet the outcome of soft tissue procedures depends directly on their elasticity and may be the most significant factor in failure of operations such as an MPFL reconstruction, rather than, say, the position to the femoral tunnel. Other factors include muscle function and control (core strength, pelvic stability and hip rotator muscle control, especially gluteus maximus) as weakness causes instability (16), as well as the body mass index, since increasing weight requires increased muscle strength for stabilization.
In conclusion, the evidence base for managing patellofemoral instability is far behind that for the ACL but has progressed enormously over the last decade with the advent of imaging techniques and methodologies that measure the anatomical variations within the extensor mechanism of the knee, both on the patella, but also the femoral side of the joint. This has allowed logical and tailored interventions in the surgical management of patellofemoral instability.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Executive Editor-in-Chief, Dongquan Shi, MD, PhD (Department of Sports Medicine and Adult Reconstruction, Drum Tower Hospital, Medical School, Nanjing University, Nanjing, China).
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2016.07.04). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dietrich TJ, Fucentese SF, Pfirrmann CW. Imaging of Individual Anatomical Risk Factors for Patellar Instability. Semin Musculoskelet Radiol 2016;20:65-73. [Crossref] [PubMed]
- Smith TO, Clark A, Neda S, et al. The intra- and inter-observer reliability of the physical examination methods used to assess patients with patellofemoral joint instability. Knee 2012;19:404-10. [Crossref] [PubMed]
- Smith TO, Cogan A, Patel S, et al. The intra- and inter-rater reliability of X-ray radiological measurements for patellar instability. Knee 2013;20:133-8. [Crossref] [PubMed]
- Smith TO, McNamara I, Donell ST. The contemporary management of anterior knee pain and patellofemoral instability. Knee 2013;20:S3-S15. [Crossref] [PubMed]
- Smith TO, Donell ST, Clark A, et al. The development, validation and internal consistency of the Norwich Patellar Instability (NPI) score. Knee Surg Sports Traumatol Arthrosc 2014;22:324-35. [Crossref] [PubMed]
- Smith TO, Chester R, Hunt N, et al. The Norwich Patellar Instability Score: Validity, internal consistency and responsiveness for people conservatively-managed following first-time patellar dislocation. Knee 2016;23:256-60. [Crossref] [PubMed]
- Hiemstra LA, Kerslake S, Lafave MR, et al. Initial validity and reliability of the Banff Patella Instability Instrument. Am J Sports Med 2013;41:1629-35. [Crossref] [PubMed]
- Dejour H, Walch G, Nove-Josserand L, et al. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 1994;2:19-26. [Crossref] [PubMed]
- Dejour H, Walch G, Neyret P, et al. Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot 1990;76:45-54. [PubMed]
- Dejour D, Saggin P. The sulcus deepening trochleoplasty-the Lyon's procedure. Int Orthop 2010;34:311-6. [Crossref] [PubMed]
- McNamara I, Bua N, Smith TO, et al. Deepening Trochleoplasty With a Thick Osteochondral Flap for Patellar Instability: Clinical and Functional Outcomes at a Mean 6-Year Follow-up. Am J Sports Med 2015;43:2706-13. [Crossref] [PubMed]
- MacKay JW, Godley KC, Toms AP, et al. Trochlear boss height measurement: a comparison of radiographs and MRI. Knee 2014;21:1052-7. [Crossref] [PubMed]
- Donell ST, Shepherd K, Ali K, McNamara I. The inferomedial patellar protuberance and medial patellar ossicle in patellar instability. Knee Surg Sports Traumatol Arthrosc 2015; [Epub ahead of print]. [Crossref] [PubMed]
- Wiberg G. Roentgenographic and anatomic studies on the femoro-patellar joint. Acta Orthop Scand 1941;12:319-410. [Crossref]
- Beighton P, Horan F. Orthopaedic aspects of the Ehlers-Danlos syn000drome. J Bone Joint Surg Br 1969;51:444-53. [PubMed]
- Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther 2010;40:42-51. [Crossref] [PubMed]
Cite this article as: Donell ST. Individual anatomical risk factors for patellar instability. Ann Joint 2016;1:13.


