Femoral neck trapdoor procedure and allograft for the chondroblastoma of the femoral head
Introduction
Chondroblastoma is a kind of infrequent benign bone tumor, which accounts for about 1–2.7% of primary bone tumors (1-3). It mainly arises from the epiphyseal plate of long bone at bone development stage (4). The proximal parts of humerus, tibia and femur, and the distal femur are frequently affected (1,3,5). Meanwhile the incidence of chondroblastoma arising from femoral head ranks the third of the most frequent bone tumor (6). The majority of patients age between 10 to 20 years old. The prevalence between male and female is 2:1 (7). Although chondroblastoma is classified as benign tumor, malignant transformation and neoplastic transplantation were reported (2,3).
Coxalgia is the main clinical manifestation of femoral head chondroblastoma. Patients could represent with claudication as a result of severe lesion, while tenderness on the Scarpa’s triangle could also be found (8). Trauma or sport injury history and limp neurovascular pathological changes usually could be excluded before diagnosis.
The treatments of femoral head chondroblastoma reported include acetabular osteotomies and osteochondral grafts (6) and vascularized fibular grafts (8-10). As a kind of benign tumor, adequate curettage of lesion and bone grafting are efficient. But the challenge is how to access the lesion, especially when it is located between the articular cartilage and epiphyseal plate. The ideal way is to find a safe and sufficient path that allows complete curettage, while preserving the joint function and development ability as far as possible.
Unfortunately, it’s unavoidable to transgress either the articular cartilage or the growth plate when the epiphysis is involved, because the proximal femoral head epiphysis is entirely included in the joint capsule. Thus there are only three choices: (I) an approach via a drill along the femoral neck which may damage the epiphyseal plate (11,12); (II) an approach directly through the surface of the femoral head, which do no harm to the growth plate but have the potential to damage the articular cartilage (6,8); (III) an open approach which includes capsulotomy and raising a “trapdoor” of the femoral neck (10).
The first approach would violate the physis of proximal femur. So that is not recommended for the skeletally immature patients. Although the second choice provides direct access to the subchondral lesion, it destroys the integrity of the femoral head articular cartilage, which may have negative impact on joint mechanical characteristics and activities later on. Mont et al. (13) used a trapdoor procedure for the treatment of late stage osteonecrosis of the femoral head and good results were reported in 1998. Trapdoor procedure is not a new approach for the femoral head chondroblastoma. Iwai et al. and Orlando-Díaz et al. both reported good surgical results of this technique in 2008 and 2014 respectively (6,8). But they both raised the trapdoor on the surface cartilage of femoral head, as a result of that, both the hip joint interface and the mechanical characteristics of femoral head were changed, which may lead to osteoarthritis and even collapse.
In order to avoid the damage of the articular cartilage and preserve the femoral head skeleton maximally, we apply a trapdoor procedure of the femoral neck for the management of the femoral head chondroblastoma.
Case presentation
A 23-year-old male was admitted to our hospital with the chief complaint of left coxalgia for 6 months. Mild claudication was represented after about 90 min of walking. Patient denied any use of steroid or history of trauma. Neither anchylosis nor clicking of joint was presented. And there were none radiative pain or sensory-motor disorders of lower limps found. Physical examination revealed tenderness of left Scarpa’s triangle and Fabere test(+) of left hip. Leg length discrepancy was not apparent, while the range of motion was normal.
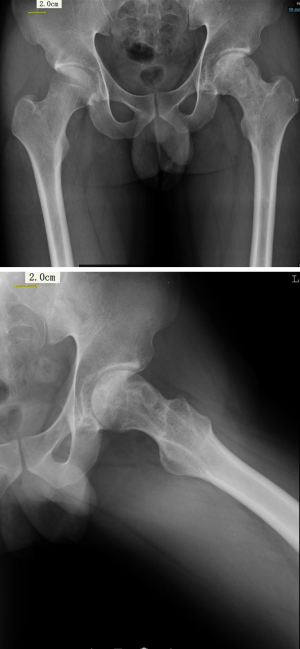
X-ray examination showed an osteolytic lesion about 3 cm × 4 cm with irregular embrace on the left femoral head. Normal joint space was seen on the plain radiograph, while neither collapse of the femoral head nor calcification inside the lesion were showed (Figure 1).

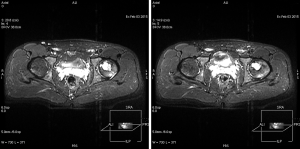
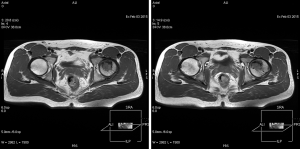
The left femoral head lesion was of relatively low signal on T1-weighted MRI, while mixed high signal and low signal of proximal lesion, and high signal of distal part were identified on T2-weighted MRI (Figures 2,3). Polycystic changes could be seen both on the coronal plane (Figure 4).

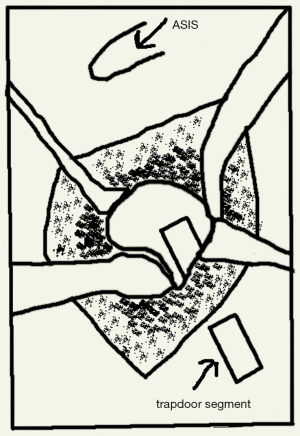
The patient took horizontal position with a comfort pad under the left hip after general anaesthesia. We performed a modified approach according to that described as Smith-Peterson path. An oblique skin incision about 10 cm was made on the anterolateral side of left hip. And then separated the tensor muscle of fascia lata and the rectus femoris along the interval to expose the capsule. On a flexion and abduction position of the hip, we opened the capsule from the anterior and posterior side so that could preserve the blood supply from the deep branch of the medial femoral circumflex artery. After that, a trapdoor segment was dissected with an osteotome. The cutting edges was about 1 cm below the femoral neck junction, about 3 cm long and 1.5 cm wide (Figure 5).
Cancellous bone of the neck was removed and soaked in normal saline in preparation for grafting. A sense of breakthrough was felt when reaching the lesion and dark red liquid was seen flowing out. Yellowish and grayfish tumor was snapped out. Intraoperative pathological diagnosis suggested tumor could not be excluded. So we thoroughly curetted along the circumference of what then flushed clean. Because of the large defect created by curettage, autologous and then allogeneic bone graft were undertaken. After that, the trapdoor segment was replaced without fixation.
After operation, walking with half weight bearing was encouraged on the second day. And the patient started full weight bearing after 6 weeks following surgery. At 3 and 16 months follow-up, this patient recovered with good joint function without pain. Limb shortening or angular deformities were not found. X-ray showed good bony union around the trapdoor. And no osteoarthritic change, femoral neck fracture, collapse of the femoral head or tumor recurrence was presented (Figure 6).
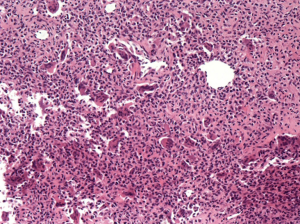
Intraoperative pathology: large amount of fibrocyte and short spindle cells were seen under the microscope, so did multinucleated giant cells. Postoperative diagnosis of paraffin sections suggested chondroblastoma. The results of immunohistochemistry were as below: S-100(+), CD1a and CD68(partly +), AE1/AE3(−), CD23(−), CD34(vessel +), Ki-67(index 5%),P53(−) and PTH(−) (Figure 7).
Discussion
Bone chondroblastoma tends to arise from the epiphyseal plate of long bone (4,14,15). In 1942, Jaffe and Lichtenstien firstly used the term “benign chondroblastoma”, which separated it from giant cell tumor of bone. The frequent locations are proximal humerus, proximal tibia, proximal and distal femur (1,3,5).
The imagining diagnosis of this case showed osteolytic changes surrounded by osteosclerosis on X-ray. Others reported that the lesion could be of mixed high signal and low signal, and of high signal on T2-weighted MRI, while relatively low signal on T1-weighted MRI (10). The diagnosis was indefinite base on the imaging examinations. Pathologic diagnosis revealed the lesion of femoral head was chondroblastoma.
There is no role for chemotherapy, and radiotherapy is contraindicated in the management of chondroblastoma. Complete curettage and bone grafting are sufficient for the treatment of femoral head chondroblastoma. The recurrence rate ranges from 10% to 40% (3,16-18). Seldom had cases been reported for local soft tissues seeding, and about 1% of cases had pulmonary metastasis (12,19).
According to this patient’s preoperative clinical symptoms and images, we could not reach the diagnosis of chondroblastoma because we could not exclude the possibility of bone tumor. The chief principle of the treatment was adequate curettage. As to the lesions located on the femoral head, posterolateral approach or direct anterior approach could be chosen for exposure of femoral head. Considering that the lesion was close to the anterior side of the femoral head, and that the patient is quite young and active, the direct anterior approach was chosen to save the greater trochanter, which avoided complications like bone healing defect, infection caused by internal fixation and lack of abductor forces. Moreover, a direct anterior approach not only provides adequate exposure which allows adequate curettage, but also protects the nerve, muscle and the articular cartilage.
As mentioned above, the minimally invasive approach which via a drill through femoral neck has an obvious limit of thorough curettage even with the use of endoscope or arthroscopy, because the long passage would restrict our operation. The second approach which through the surface of the femoral head would damage the articular cartilage though it provides good exposure. And it’s likely to affect the skeleton of femoral head. A trapdoor through the femoral neck may provide relatively good operation pathway and avoid damaging the articular cartilage. As for a 23 years old patient, a trapdoor procedure via the femoral neck not only provides relatively good visualization than the first one, but also avoids mal-development of epiphysis.
This procedure does not need to dislocate the hip joint; on the other hand, it can preserve the integrity of the articular cartilage. But the disadvantages still need our attention. This approach may destroy the growth plate which depends on the location of the lesion, thus may cause leg length discrepancy. Lin et al. reported that some patients who were treated before skeletal maturity had been reached, they had a growth disturbance, but no one developed avascular necrosis (18). Strong et al. (10) also reported no necrosis of the femoral head after the trapdoor procedures. But two of five patients were reported to have recurrence at the follow-up time of 4 and 16 months respectively. Tumor recurrence maybe because the limit of visualization during operation. Besides, thin path also limits the curettage of the lesion. Pathological fracture and angular deformity have also been reported by Grimer et al. who performed curettage through the base of the femoral neck (20). To deal with these problems, great patience and meticulousness are necessary for good results. Patient’s selection is important too, according to recent reports, recurrence tends to happen in skeletal immature patients (1); so an approach up the femoral neck is much more safer when the patient has reached skeletal maturity.
Although a trapdoor procedure on the femoral neck may have complications mentioned above, we consider that it grants better access to subchondral lesions of the femoral head than an approach which uses a drill along the femoral neck and it does no harm the articular cartilage. However, more cases are needed to prove whether this procedure could render good post-operative outcome. In skeleton mature patients with femoral head chondroblastoma, we consider the femoral neck trapdoor procedure as a good option for surgical treatment.
Acknowledgments
Funding: This work was supported by Surface project of National Natural Science Foundation of China (No. 81572110).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.01.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huvos AG, Marcove RC. Chondroblastoma of bone. A critical review. Clin Orthop Relat Res 1973;300-12. [Crossref] [PubMed]
- Xu A, Xu W, Liu J. Diagnosis of CT and MRI on Bone and Joint. Jinan: Shandong Science and Technology Press, 2002:157-60.
- Ramappa AJ, Lee FY, Tang P, et al. Chondroblastoma of bone. J Bone Joint Surg Am 2000;82-A:1140-5. [Crossref] [PubMed]
- Fletcher CD, Unni KK, Mertens F. Pathology and Genetics of Tumours of Soft Tissue and Bone. World Health Organization Classification of Tumours. Lyon: International Agency for Research on Cancer (IARC) Press, 2002:241-2.
- Springfield DS, Capanna R, Gherlinzoni F, et al. Chondroblastoma. A review of seventy cases. J Bone Joint Surg Am 1985;67:748-55. [Crossref] [PubMed]
- Orlando-Díaz C, Guzmán-Vargas R, Rincon-Cardozo DF, et al. Femoral head chondroblastoma and reconstruction with osteochondral allograft. Case report. Acta Ortop Mex 2014;28:378-81. [PubMed]
- van der Eijken JW. Strategy in the treatment of benign bone tumors: an overview. J Pediatr Orthop B 1998;7:249-52. [Crossref] [PubMed]
- Iwai T, Abe S, Miki Y, et al. A trapdoor procedure for chondroblastoma of the femoral head: a case report. Arch Orthop Trauma Surg 2008;128:763-7. [Crossref] [PubMed]
- Givissis P, Agathangelidis F, Christodoulou E, et al. Chondroblastoma of the femoral head disrupting the articular cartilage. Description of a novel surgical technique. Acta Orthop Belg 2012;78:414-7. [PubMed]
- Strong DP, Grimer RJ, Carter SR, et al. Chondroblastoma of the femoral head: management and outcome. Int Orthop 2010;34:413-7. [Crossref] [PubMed]
- Stricker SJ. Extraarticular endoscopic excision of femoral head chondroblastoma. J Pediatr Orthop 1995;15:578-81. [Crossref] [PubMed]
- Thompson MS, Woodward JS Jr. The use of the arthroscope as an adjunct in the resection of a chondroblastoma of the femoral head. Arthroscopy 1995;11:106-11. [Crossref] [PubMed]
- Mont MA, Einhorn TA, Sponseller PD, et al. The trapdoor procedure using autogenous cortical and cancellous bone grafts for osteonecrosis of the femoral head. J Bone Joint Surg Br 1998;80:56-62. [Crossref] [PubMed]
- Xu S, Ge B, Xu Y. Practical Orthopedics. IV Edition. Beijing: People's Military Medical Press, 2012:1731-3.
- Xu W, Li F. Tumors of Bone and Soft Tissues. Beijing: People's Medical Publishing House, 2008:421-3.
- Schuppers HA, van der Eijken JW. Chondroblastoma during the growing age. J Pediatr Orthop B 1998;7:293-7. [Crossref] [PubMed]
- Suneja R, Grimer RJ, Belthur M, et al. Chondroblastoma of bone: long-term results and functional outcome after intralesional curettage. J Bone Joint Surg Br 2005;87:974-8. [Crossref] [PubMed]
- Lin PP, Thenappan A, Deavers MT, et al. Treatment and prognosis of chondroblastoma. Clin Orthop Relat Res 2005;103-9. [Crossref] [PubMed]
- Elek EM, Grimer RJ, Mangham DC, et al. Malignant chondroblastoma of the os calcis. Sarcoma 1998;2:45-8. [Crossref] [PubMed]
- Grimer RJ, Tillman RM, Carter SR. Local recurrence of chondroblastoma. J Bone Joint Surg Am 2001;83-A:623-4. [Crossref] [PubMed]
Cite this article as: Ye C, Qian W, Jiang C, Zhu S, Chen X. Femoral neck trapdoor procedure and allograft for the chondroblastoma of the femoral head. Ann Joint 2017;2:5.