
Immediate unrestricted versus graduated weight bearing following primary cementless total hip arthroplasty: a randomized controlled trial
Introduction
Total hip arthroplasty (THA) is the standard surgical intervention for most of hip disorders. The aim of the surgery is to restore the function and eliminate the pain in patients with severe hip osteoarthritis (1,2) Improving the understanding of the biomechanics of the hip joint helps in reducing the loads on it during daily activities and restoring normal function while decreasing failure rate (3).
Cemented THA was the standard surgical option several years ago, but uncemented implants are now growing more popular. There is no issue about immediate unrestricted weight bearing (UWB) for uncomplicated cemented THA, which is the main concern for cementless THA.
Stability of cementless femoral components is such a key element for successful THA. This stability was evaluated by the measurement of relative micromotion on a few simultaneous locations around the stem in cadaveric experiments (4).
It is questionable whether immediate UWB following cementless THA could result in better prognosis on the long and the short terms (i.e., early recovery and independency in day activities) (5). Immediate rehabilitation with UWB could have the advantage of shortening the hospital stay following THA and getting the patient quickly involved in daily-life activities after such major surgery (6). Protected weight-bearing rehabilitation after cementless THA has also been reported to decrease micromotion of the stem component, especially when using two crutches for at least 6 weeks postoperatively (7,8). Full or UWB immediately after surgery has been reported to prevent deep venous thrombosis (9). However, early weight bearing may result in micromotion of the femoral stem with increasingly fibrous growth around the hip prosthesis (10-12).
The aim of this study is to assess the effect of immediate and graduated UWB on the clinical outcome of primary cementless THA and to assess the amount of micromotion associated with this rehabilitation protocol.
Methods
Twenty subjects participated in this study with primary cementless THA and mean age 57.5 years (range, 50–65 years). They were randomly divided into two groups (group A and group B); see Table 1. Although subjects were non-computationally randomized (by admission), the randomization gave some consistent results in terms of gender division. Written consent was obtained for all patients who were involved in this study. This study has obtained an ethical committee approval (135/2015) from the Faculty of Physical Medicine, Cairo University. of gender division. Written consent was obtained for all patients who were involved in this study.

Full table
Group A (10 subjects) started rehabilitation program with immediate UWB gait training, and group B (10 subjects) started with graduated weight bearing (GWB) gait training. Both groups were tested immediately after surgery and 6 and 12 weeks postoperatively.
All subjects selected for this study had either unilateral or bilateral and primary cementless THA and had a referral including medical report and clarifying medical status stability. They all have followed their entitled physical therapy program. Subjects of group A under UWB have been allowed to use a cane or one crutch in the first week or within the hospital stay only for balance not for weight bearing.
Morbid, obese subjects or subjects with hip implant due to rheumatoid disease, tumors, developmental dysplasia, musculoskeletal disorders or deformities were excluded from this study. Also, subjects who require special footwear or foot/leg prosthesis pre- or postoperatively were also excluded.
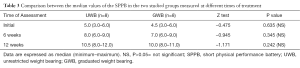
Clinical evaluations have been performed 1 week after surgery (initial) and 6 and 12 weeks postoperatively and yearly thereafter. Harris hip score (HHS) and short physical performance battery (SPPB) were used to evaluate the outcome of the operations. Changes in HHS, SPPB and micromotion of the femoral stem vertically have been measured and statistically analyzed with ANOVA test.
The axial migration (micromotion) of the stem was measured on digital radiographs through calculating the distance from the tip of the greater trochanter to a reference point in the stem. The vertical distance between the two points is calculated on each film and the difference was considered as a measure of the subsidence of the prosthesis. The intraobserver error has been considered, and the immediate postoperative and last follow-up X-rays were evaluated (Figure 1).
Results (findings) were expressed as median value or percentage. The variables in the two groups were compared through Mann Whitney test, while the different assessments within the same group were compared through Friedman ANOVA followed by Wilcoxon sign rank test for pair wise comparison. Categorical data were compared through Z test. The data were considered significant if P value was ≤0.05 and highly significant if P value <0.01. Statistical analysis was performed through SPSS (version 16 windows).
All subjects in both groups have been operated with THA recently with the postoperative manifestations of functional impairments after hip arthroplasty were investigated by the use of HHS and SPPB (Tables 2,3). A physical examination was conducted for each subject prior to acceptance to enrollment in this study. All subjects have been inspected for postural asymmetry and deformities. The examination consisted of checking any muscle weakness, possible joint instability, leg discrepancy ≤1 inch, balance impairment, sensory abnormalities, vascular trouble or other conditions that may affect the lower and upper extremities as well as any related body segments.

Full table
Full table
Results
Group A had a mean age of 54.5 (range, 50.0–65.0) years, and a female to male ratio of 5:5, while group B had a mean age of 56.0 (range, 51.0–65.0) years and a female to male ratio of 5:5.
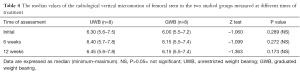
In group A, there was no statistically significant difference in median values of the radiological vertical micromigration of femoral stem measured at 6 weeks post-assessment (median 6.15; range, 5.5–7.4) and their corresponding at 12 weeks post-assessment (median 6.15; range, 5.5–7.4; P=0.317) as shown in Figure 2 and Table 4. In group B, there was no statistically significant increase in median values of the radiological vertical micromigration of femoral stem measured at both 6 weeks post-assessment (median 6.15; range, 5.5–7.4; P=0.028) and 12 weeks post-assessment (median 6.15; range, 5.5–7.4; P=0.018) when compared with initial time of assessment (median 6.0; range, 5.5–7.2).

Full table
Discussion
THA is currently one of the most widely performed procedures in orthopedic practice. Although the use of cementless THA has rapidly spread, it should be remembered that problems specific for cementless THA do occur, as with cemented THA.
No marked evidence was found that makes cementless THA less desirable than cemented type despite potential complications in the mechanical stem (13). In cementless THA, early weight bearing is common although it is still not evident enough to replace other protocols. Immediate rehabilitation with protected weight bearing after uncemented THA can be performed by gait pattern using crutches or by stair climbing (13). No adverse effect was found regarding micromotion or osteointegration of the femoral stem with immediate UWB following uncemented THA. There was also no correlation between immediate UWB and failure of osseointegration or implant loosening.
In this study, we evaluated the effect of partial and full weight bearing after cementless THA with different types of hip prostheses (ABG; Stryker-Howmedica, USA) using radiostereometric analysis (RSA). Both groups had primary cementless THA and were tested immediately after surgery and 6 and 12 weeks postoperatively. All patients were operated in a standardized way by three experienced surgeons and they were randomized to partial or full weight bearing during the first 6 weeks after surgery. Subjects of group A started immediate UWB gait training within rehabilitation program and group B started with GWB gait training. No adverse effect was found between the two groups, which justifies using this regimen after uncemented THA (14). Hol et al. give a moderate to strong evidence for immediate UWB after primary uncemented THA, that is, patients started their rehabilitation as soon as possible after surgery with immediate weight bearing as tolerated (6).
Götze et al. have collected clinical and radiographic findings of 46 patients who underwent 50 consecutive primary THA using porous-coated femoral components with 2-years follow-up period. Twenty five patients had performed full weight bearing immediately after THA. The authors compared the results with a previous control group that performed UWB (≤50 lb) for 6 weeks and they found that the femoral components in both groups had radiographic evidence of bone ingrowth fixation at the final follow-up. Thus, it seems that bone ingrowth occurs whether partial or full weight-bearing protocol is followed for postoperative rehabilitation (15).
Only two studies found significant increase in subsidence after full weight bearing during the first 6 weeks after surgery as a result of all previous findings and clinical research results regarding the significance of weight bearing on postoperative THA patients (16,17).
The novelty of this study comes as we study the effect of immediate UWB and how it affects the function, mobility and restoration (especially gait performance and independency) and, at the same time, how weight bearing affects the micromotion of THA prosthetic stem vertically. Limitations of this study are the number of patients which is relatively low, and that RSA markers were not used to measure the amount of subside (migration).
In this work, immediate UWB was found to have the same effect as GWB on hospital stay, rehabilitation process, gait parameters and independency after primary cementless THA.
Conclusions
In comparison to graduate weight-bearing protocol, immediate unrestricted rehabilitation following cementless THA had similar clinical outcome in terms of HHS and axial micromotion of the prostheses.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.01.03).The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study has obtained an ethical committee approval (135/2015) from the Faculty of Physical Medicine, Cairo University and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Harkness JW. Arthroplasty of hip. In: Canale ST. editor. Campbell’s operative orthopaedics. 9th ed. St Louis: Mosby, 1998:296-471.
-
Swedish Hip Arthroplasty Register - Stansfield BW, Nicol AC. Hip joint contact forces in normal subjects and subjects with total hip prostheses: walking and stair and ramp negotiation. Clin Biomech (Bristol, Avon) 2002;17:130-9. [Crossref] [PubMed]
- Gortchacow M, Wettstein M, Pioletti DP, et al. Simultaneous and multisite measure of micromotion, subsidence and gap to evaluate femoral stem stability. J Biomech 2012;45:1232-8. [Crossref] [PubMed]
- Roos EM. Effectiveness and practice variation of rehabilitation after joint replacement. Curr Opin Rheumatol 2003;15:160-2. [Crossref] [PubMed]
- Hol AM, van Grinsven S, Lucas C, et al. Partial versus unrestricted weight bearing after an uncemented femoral stem in total hip arthroplasty: recommendation of a concise rehabilitation protocol from a systematic review of the literature. Arch Orthop Trauma Surg 2010;130:547-55. [Crossref] [PubMed]
- Mont MA, Yoon TR, Krackow KA, et al. Clinical experience with a proximally porous-coated second-generation cementless total hip prosthesis: minimum 5-year follow-up. J Arthroplasty 1999;14:930-9. [Crossref] [PubMed]
- Zernicke R, MacKay C, Lorincz C. Mechanisms of bone remodeling during weight-bearing exercise. Appl Physiol Nutr Metab 2006;31:655-60. [Crossref] [PubMed]
- Buehler KO, D'Lima DD, Petersilge WJ, et al. Late deep venous thrombosis and delayed weightbearing after total hip arthroplasty. Clin Orthop Relat Res 1999;123-30. [Crossref] [PubMed]
- Berzins A, Sumner DR, Andriacchi TP, et al. Stem curvature and load angle influence the initial relative bone-implant motion of cementless femoral stems. J Orthop Res 1993;11:758-69. [Crossref] [PubMed]
- Jasty M, O'Connor DO, Henshaw RM, et al. Fit of the uncemented femoral component and the use of cement influence the strain transfer the femoral cortex. J Orthop Res 1994;12:648-56. [Crossref] [PubMed]
- Wirtz DC, Heller KD, Niethard FU. Biomechanical aspects of load-bearing capacity after total endoprosthesis replacement of the hip joint. An evaluation of current knowledge and review of the literature. Z Orthop Ihre Grenzgeb 1998;136:310-6. [Crossref] [PubMed]
- Zwartelé RE, Witjes S, Doets HC, et al. Cementless total hip arthroplasty in rheumatoid arthritis: a systematic review of the literature. Arch Orthop Trauma Surg 2012;132:535-46. [Crossref] [PubMed]
- Thien TM, Ahnfelt L, Eriksson M, et al. Immediate weight bearing after uncemented total hip arthroplasty with an anteverted stem: a prospective randomized comparison using radiostereometry. Acta Orthop 2007;78:730-8. [Crossref] [PubMed]
- Götze C, Steens W, Vieth V, et al. Primary stability in cementless femoral stems: custom-made versus conventional femoral prosthesis. Clin Biomech (Bristol, Avon) 2002;17:267-73. [Crossref] [PubMed]
- Bottner F, Zawadsky M, Su EP, et al. Implant migration after early weightbearing in cementless hip replacement. Clin Orthop Relat Res 2005;132-7. [Crossref] [PubMed]
- Rao RR, Sharkey PF, Hozack WJ, et al. Immediate weightbearing after uncemented total hip arthroplasty. Clin Orthop Relat Res 1998;156-62. [Crossref] [PubMed]
Cite this article as: Shabana M, Hafez MA, Ayad K, Abd Elfatah M, Zaky LA. Immediate unrestricted versus graduated weight bearing following primary cementless total hip arthroplasty: a randomized controlled trial. Ann Joint 2017;2:6.



