
What can we learn from Australian Orthopaedic Association National Joint Replacement Registry 2016 annual report?
The Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) publish their report every year, we have previously analyzed the 2014 annual report, which contained 410,767 hip replacements and 480,440 knee replacements (1). This year is the 15th year for AOANJRR. Therefore, they have now published 15-year data for hip and knee replacements. It is also the first year they have published shoulder replacements, which contains 32,406 shoulder procedures (2).
The aim of national registries is to decrease the revision rates of arthroplasties by detecting outlier implant performance earlier. Through 15 years of work, we can see the effect of the registry data, with the proportion of revision hip procedures reported to the registry declining from 12.9% of all hip procedures in 2003 to 9.6% in 2015. Revision knee procedures declined from a peak of 8.8% in 2004 to 7.4% in 2015. These are now the lowest proportions ever reported to the registry.
The AOANJRR annual report always presents the data and results they have collected but does not offer to explain the meaning of the data and results. They encourage surgeons to interpret the data using their own experience and understanding. We have analyzed the new data which we are most interested in and review the different results in comparison to our last editorial (1). We must emphasize that our following analysis and interpretation of the AOANJRR 2016 report are based on the authors’ personal understanding and clinical experience. All the data presented is from AOANJRR 2016 annual report, which can be found on the official website. We encourage all readers to download their free copy and check the data against your own interests and experience. We are happy to discuss differences of opinion if the reader has some alternative interpretations of the data.
In this article, we continue to put our focus on hip and knee replacements because this is our area of interest and it is not very common for total or reverse shoulder replacements to be performed in Chinese hospitals. The 2016 annual report contains 498,660 hip replacements and 592,577 knee replacements, with an additional 87,983 (17.62%) hip and 112,137 (18.92%) knee replacements compared to the 2014 annual report. Compared to our last article, the cases of total hip arthoplasty (THA) or total knee arthroplasty (TKA) have increased almost 20%, furthermore, some of the data have shown different results which may change our clinical considerations. Hence, we analyze the annual report again to give some further insights to our readers.
Hip and knee replacements in younger patients
The focus of the 2016 annual report is on the outcome of hip and knee replacements in younger patients (those aged less than 55 years). In our experience, Chinese patients receiving primary THA are relatively younger than Australian patients due to the increased incidence of avascular necrosis of femoral head, developmental dysplasia of the hip (DDH) and ankylosing spondylitis. Therefore the current data is of very important references for our prostheses choice.
The revision rate of hip and knee arthroplasty in younger patients is a major focus of 2016 AOANJRR annual report. It is believed that younger patients have higher rates of revision. The purpose of this analysis is to provide information on how best to optimize the outcome of these procedures in this patient population (aged less than 55 years).
In the 2016 AOANJRR annual report, there are 43,380 patients whose age was less than 55 years up to and including 31 December 2015, which constitutes about 13.1% of cases for all primary THA. Compared to the data from 2003, the total number of THA procedures has increased by 96.2%, while the percentage of cases aged under 55 increased from 11.7% to 13.1%. From these data, we can infer that the growth of THA’s has not been due to broadening the operative indications.
The major indications for THA in the less than 55-year old age group are osteoarthritis (OA) (78.04%), avascular necrosis of the femoral head (8.71%) and DDH (6.41%). The revision rates over 10 and 15 years in the less than 55-year age group (with the primary diagnosis of OA) are 5.8% and 9.9%, compared to 5.1% and 8.0% revision rate for all age groups (with the same primary diagnosis of OA). We feel that age does not have a significant impact on the revision rate. For femoral neck fractures in young patients, some surgeons choose THA as first line treatment when the fracture is comminuted and displaced where the surgeon feels that nonunion and necrosis of femoral head are highly likely. The data implies that it should not be the first line treatment as the revision rates over 3 and 10 years are 6.2% and 15.5% respectively. This implies the results of THA for femoral neck fractures is not as good as perhaps some surgeons believe and possibly could be deferred following a trial of less invasive treatments.
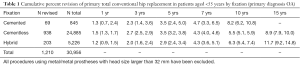
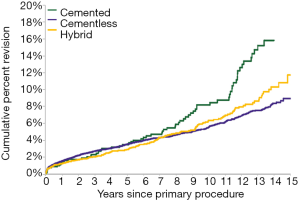
In this group of patients, most THA are cementless (80.4%), Hybrid and cemented THA are performed less frequently (16.9% and 2.7% respectively) (Table 1). The revision rate at 10 years was 5.5% for cementless, 6.3% for hybrid and 8.2% for cemented and the revision rate at 15 years was 8.9% for cementless and 11.7% for hybrid (Table 1,Figure 1). Interestingly, there is no difference in the revision rate with different types of fixation when non-XLPE (cross-linked polyethylene) is excluded from the analysis (Table 2,Figure 2). This result implies non-XLPE may be the major problem in THA, XLPE is more important than the fixation choice. Considering the situation in China, we strongly recommend all total hip replacements not to use non-XLPE bearing.
Full table
Full table
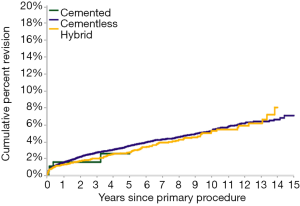
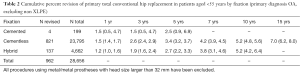
In the 2016 AOANJRR report, there are 2,579 THA in the less than 55-year age group with the primary indication being DDH. The revision rate after 10 and 15 years in this group was 5.7% and 9.9% respectively (Table 3, Figure 3), compared to 5.8% and 9.9% revision rates in the same age group with a primary indication being OA. This result implies that while the procedure is technically challenging for the surgeon, the outcomes are comparable to other that for primary OA (Table 4,Figure 4). We interpret this data as an indication for THA for all patients who have met the operative indications for THA, following maturation of the osteoepiphysis, with age not being a direct contraindication.

Full table
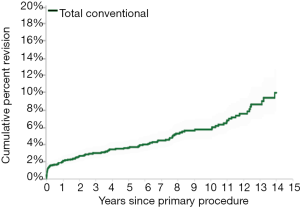
Full table
In the 2016 AOANJRR annual report, there are 33,897 TKA patients who were less than 55 years of age up to and including 31 December 2015, which is about 7.0% of the total cases for primary TKA. Compared to the data from 2003, the total number of TKA cases has increased 130.4%, but the percentage in this age group only increased from 6.8% to 7.0%. From this data, we can again infer that the growth of overall TKA was not from broadening the surgical indications.
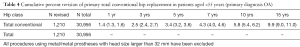
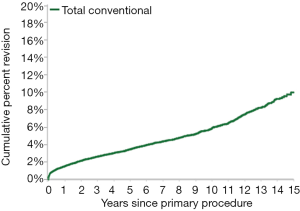
The major indications for TKA were OA (93.7%) and rheumatoid arthritis (3.6%) (Table 5). The revision rate after 10 and 15 years in the less than 55 years age group with OA as the primary diagnosis was 10.9% and 15.7% respectively (Table 6). This is in comparison to 5.3% and 7.3% for 10 and 15 year revision rates in all age groups (Table 7). Unlike the results for THA, age appears to have a greater impact on revision rates. The long-term results of TKA in younger patients are not as promising as the results for THA, meaning greater work should be done to prevent of delay the requirement for TKA in the young age groups.
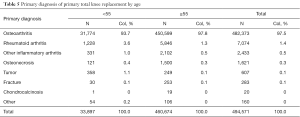
Full table
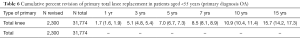
Full table
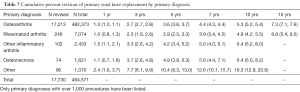
Full table
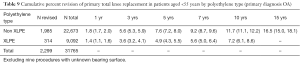
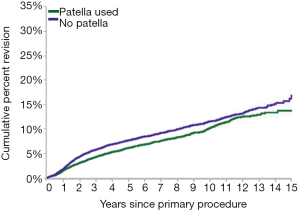
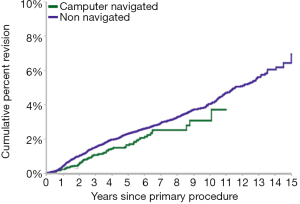
In this age group, there are four factors which will affect the revision rate. Minimally stabilized prostheses (Table 8,Figure 5), XLPE (Table 9,Figure 6), patellar resurfacing (Table 10,Figure 7) and computer navigation (Table 11,Figure 8) were associated with lower rates of revision. Other factors such as prostheses fixation, bearing mobility, image derived instrumentation (IDI) have no difference in 10-year survivorship. Of course, prostheses choice also highly affects the revision rate. There are 17 prosthesis combinations which have 10-year revision rate data, only three of the 17 combinations have less than 10% revision rate at the 10-year follow-up. They are Nexgen CR with Nexgen, Nexgen CR Flex with Nexgen and PFC Sigma PS with MBT.
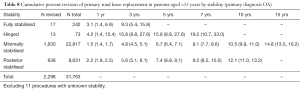
Full table
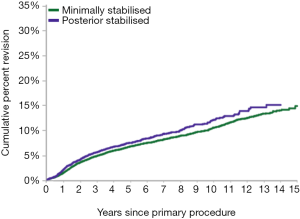
Full table

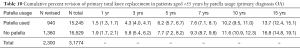
Full table
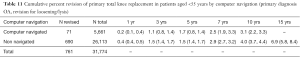
Full table
Ten- and 15-year prosthesis outcomes
This year is the 15th year for the AOANJRR. They have now published 15 years of data for hip and knee replacements and their revisions. In these reports, the number of individual combinations of femoral and acetabular hip prostheses with 10-year outcomes has increased by 20.3%. There are 71 femoral and acetabular combinations with 10-year outcome data; these prosthesis combinations account for 62.3% of all primary THA. Checking the 10-year outcome data, we find only seven combinations with a revision rate less than 3%, they are the Alloclassic with Trilogy (1.9%), Exeter V40 with Mallory-Head (2.9%), MS 30 with Fitmore (2.5%), MS 30 with Low Profile Cup (2.4%), Natural Hip with Allofit (1.9%), Summit with Pinnacle (2.8%) and Synergy with Trident (Shell) (3.0%). In these seven prosthesis combinations, Natural Hip with Allofit and Synergy with Trident (Shell) have not had any reported use in primary THA in the 2015 annual report, this also means these two combinations have achieved only 10-year outcome data.
There are 46 total knee replacement combinations with 10-year outcome data, these prosthesis combinations accounts for 78.9% of all primary TKA. Checking the 10-year outcome data, we find only six combinations with revision rates less than 4%, they are the Nexgen CR with Nexgen (3.0%), Nexgen CR Flex with Nexgen (2.9%), Nexgen CR Flex with Nexgen TM CR (3.1%), PFC Sigma CR with AMK Duofix (3.2%), PFC Sigma CR with PFC Sigma (3.5%), and Triathlon CR with Triathlon (3.4%). In these six combinations, PFC Sigma CR with AMK Duofix has only outcome data for the previous 10 years.
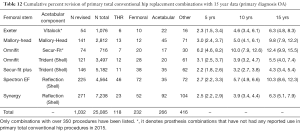
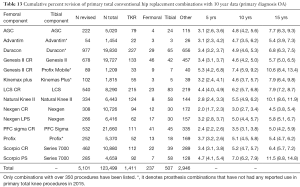
There are 7 hips (Table 12) and 14 knees (Table 13) prosthesis combinations with 15-year outcome data, only Secur-Fit Plus with Trident (Shell) (4.3%) in THA and Nexgen CR with Nexgen (4.5%) in TKA have less than a 5% revision rate. Interestingly, the 10-year revision rate for the combination of Secur-Fit Plus with Trident (Shell) is 3.2%, was not the best combination in the 10-year outcome data.
Full table
Full table
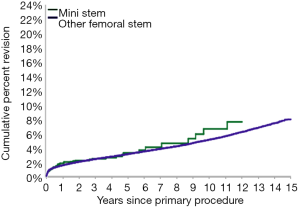
New prostheses choice
Some surgeons prefer short femoral stems for the patients because it is thought to preserve the proximal femur bone. These types of femoral stems are called mini stems in AOANJRR reports. There have been 2,102 procedures using mini stems undertaken for OA, which is less than 1% of all THA. The 10-year revision rate for a mini stem is 6.6% compared to 5.1% for other femoral stems. However, there is not yet a difference in outcomes when a mini stem is used (Figure 9). This result means that mini stems can still be used in patients who meet the indications.
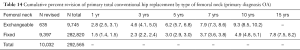
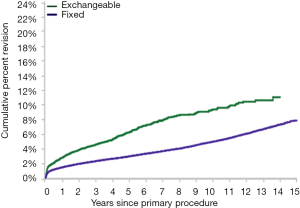
Modular femoral stems are widely used for some difficult cases especially in DDH patients because it enables the surgeons to have increased choice with femoral neck version, offset and leg length. This type of femoral stem is called femoral stems with exchangeable necks in the AOANJRR reports. There have been 9,745 procedures using femoral stems with exchangeable necks undertaken for OA. The 10-year revision rate for this type of stem is 9.3% compared to 4.9% for fixed neck stems, which is almost twice the revision rate compared to fixed neck stems (Table 14,Figure 10). These results indicate that we should use these types of stems cautiously unless it is necessary.
Full table
We have analyzed the results that we find interesting, and the analysis and interpretations are based on our personal understanding and clinical experience. There are more details in the annual report, we strongly recommend all our readers to check the results that they find interesting and try to find the answers or references to their clinical questions. We are also happy to answer any questions or discuss variations in interpretation of the AOANJRR reports.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.02.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang T, Wang W, George D, et al. What can we learn from AOANJRR 2014 annual report? Ann Transl Med 2015;3:131. [PubMed]
- Australian Orthopaedic Association National Joint Replacement Registry 2016. Hip Knee and Shoulder Arthroplasty Annual Report 2016. Available from: https://aoanjrr.sahmri.com/documents/10180/275066/Hip%2C%20Knee%20%26%20Shoulder%20Arthroplasty
Cite this article as: Huang T, Wang W, George D, Mao X, Graves S. What can we learn from Australian Orthopaedic Association National Joint Replacement Registry 2016 annual report? Ann Joint 2017;2:11.


