Multiple joint reconstructions in one patient: computer-assisted simultaneous procedures
Introduction
Multiple joint reconstructions were found to be an effective treatment improving patients’ general health but with variable complications and outcomes (joint function) (1). Patients undergoing multiple joint replacements are usually found with sort of disability and it is important to assess treatment expectancy and credibility to perform distinguishable surgical procedure(s) (2). Comprehensive assessment and accurate selection of surgical technique and treatment philosophy have good impact on the clinical results of joint arthroplasty. In addition, identifying the risk factors for poor outcome, such as obesity, low immunity and other serious comorbidities, is also essential for successful arthroplasty (3). Multiple joint replacements require adequate systemic treatment before surgery, that is, patients must be aware of the possible complications, especially those who have comorbidities such as osteoporosis and rheumatoid arthritis (4).
Patients with neglected juvenile polyarthritic diseases are subject to complications and dysfunctions of multiple joints because of the disease itself or the associated irreversible deformities such as ankylosis and soft-tissue contracture (5). In young age, prior to any intervention, patients need to have emotional stability and motivation through family and social support; they also need to reduce their weight and general physical activity (6). Initial management of these patients could start with soft tissue release and synovectomies followed by joint reconstruction with frequently cemented fixation and bone grafting to prevent further bone and joint deformities. The main goal of arthroplasty in this case is to relieve pain, to correct deformity and to restore limb function, mechanical axis and alignment (7). However, multiple joint replacements in juvenile polyarthritic patients were found to have less implant endurance due to the higher stresses on implants in addition to the poor bone stock, osteoporosis and rheumatoid cysts (5).
The aim of this work is to present a patient with juvenile idiopathic arthropathy (JIA) that underwent replacement of six joints with 4-year follow-up.
Patients and methods
A 32-year-old male presented with unsound, fused six joints with deformities (both hips, both knees, right ankle and subtalar joints). The patient was found to have JIA. He was no-walker for 4 months. This patient had his condition started at 6 years old when he could not move his joints normally. His hip joint became painful while moving, walking and playing. Then, he started to feel back pain which prevented him from binding his shoes or lifting any think from ground and at that time he was diagnosed as ankylosing spondylitis.
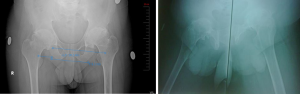
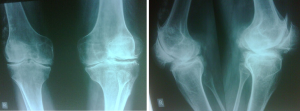
Deformity of hips was flexion with average 35–45° (Figure 1). Deformity of knees was 35° flexion deformity (Figure 2). The patient had severe valgus right ankle and hind foot (Figure 3).
He was denied for surgical intervention by the anesthetist because of insufficient intubation and/or spinal anesthesia.
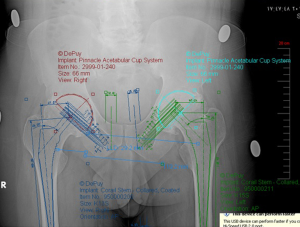
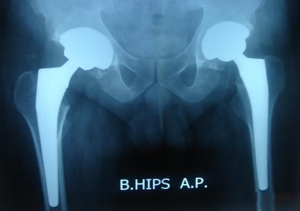
After multidisciplinary consultation, a decision was made to do multiple joint reconstructions in three sessions. That is, bilateral simultaneous total hip arthroplasty (THA) using preoperative digital hip templating and minilateral approach (Figures 4,5). After 1 year, on the second session, bilateral simultaneous total knee arthroplasty (TKA) was done, using patient-specific templates (PST). Another year later, on the final session, ankle replacement and pan talar arthrodesis nail were done using transfibular approach (Figure 6). All operations were done under general anesthesia.
Results
In this work, deformities were corrected and the patient was able to walk and go back to work as an IT manager. Postoperative long leg film showed good alignment of both limbs (Figure 7). After 4-year follow-up, the only complication was late skin problem related to one of the distal locking screws in the right ankle. This has improved after removal of the arthrodesis nail.
Discussion
Little literature had focused on the applicability of multiple joint replacements although the procedure is urged for disabled patients. To the authors’ knowledge, no previous literature described ankle procedures along with THA and TKA.
Mulhall et al. found that early and aggressive intervention could result in good long-term functional outcomes in young patients with juvenile rheumatoid arthritis, significant disability and pain from previous conservative management (5). Papanikolaou et al. had no significant difference in complications’ rate between the single TKA and the multiple joint replacements when considering thromboembolism, infection, aseptic loosening and patellar problems (6).
This condition requires thorough diagnosis and accurate planning for surgery(s). Patients must be encouraged to do surgeries on the planned timelines, especially those with bad history of previous surgeries or other therapies. With the current advancements in computer-assisted orthopedic surgery (CAOS), these patients could benefit from bilateral simultaneous surgery using minimally invasive technique with its high accuracy to improve function and restore mechanical axes of lower limbs.
Similarly with other literature, our patient has regained good activity, especially in capacity of walking, after multiple arthroplasty. Patients with JIA need to have light bodyweight and less physical activity as the initial joint replacement is not easy because of abnormal hip development, brittle bone and thin cortex. Preoperative surgical plan could be changed and modified during the replacement, while small-sized reamers/implants and bone graft must be steadily in the operative theater during surgery to ensure stable joint (8).
Our treatment plan was designed in accordance with Shrinand et al., that is, multiple arthroplasty for juvenile polyarthritis patients with severe hip/knee deformities must start with hip reconstruction followed by knee replacement as TKA requires balanced mechanical axis and position of the hips to ascertain alignment of the lower limbs. Our decision for secondary reconstruction (ankle procedures) is also in line with their conclusion, that is, other orthopaedic surgeries could be frequently required (e.g., foot osteotomies) and these surgeries could be done combinable to each other to help the patients to gain their full mobility. It is worth mentioning that deformities of the upper limb and spine are unnecessarily an indication for joint replacement but could endanger the overall functional outcome (9).
This work describes how bilateral simultaneous procedures were done with PST and CAOS. The techniques were useful as they were minimally invasive, especially in the presented patient who had difficulty having either general or spinal anesthesia and been transferred to different hospitals declining his anesthesia and surgery. Thus, he was advised to do bilateral simultaneous joint replacements as he had no chance for further anesthesia.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.04.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Ethical approval was obtained from the Institutional Review Board (IRB), Faculty of Medicine, October 6 University and written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Liu J, Wu J, Dou Y, et al. Assessment of quality of life after multiple arthroplasty. Beijing Da Xue Xue Bao 2015;47:285-8. [PubMed]
- Haanstra TM, Tilbury C, Kamper SJ, et al. Can Optimism, Pessimism, Hope, Treatment Credibility and Treatment Expectancy Be Distinguished in Patients Undergoing Total Hip and Total Knee Arthroplasty? PLoS One 2015;10:e0133730 [Crossref] [PubMed]
- Mittag F, Leichtle CI, Schlumberger M, et al. Clinical outcome after infected total knee and total hip arthroplasty. Acta Ortop Bras 2016;24:43-7. [Crossref] [PubMed]
- Shinomiya F, Mima N, Hamada Y, et al. Long-term outcome of patients with rheumatoid arthritis treated by multiple arthroplasty. Mod Rheumatol 2005;15:241-8. [Crossref] [PubMed]
- Mulhall KJ, Saleh KJ, Thompson CA, et al. Results of bilateral combined hip and knee arthroplasty in very young patients with juvenile rheumatoid arthritis. Arch Orthop Trauma Surg 2008;128:249-54. [Crossref] [PubMed]
- Papanikolaou A, Droulias K, Nikolaides A, et al. Results of a single total knee prosthesis compared with multiple joint replacement in the lower limb. Int Orthop 2000;24:80-2. [Crossref] [PubMed]
- Lachiewicz PF, McCaskill B, Inglis A, et al. Total hip arthroplasty in juvenile rheumatoid arthritis. Two to eleven-year results. J Bone Joint Surg Am 1986;68:502-8. [Crossref] [PubMed]
- Goodman SB, Oh KJ, Imrie S, et al. Revision total hip arthroplasty in juvenile chronic arthritis: 17 revisions in 11 patients followed for 4-12 years. Acta Orthop 2006;77:242-50. [Crossref] [PubMed]
- Vaidya SV, Aroojis A. Multiple joint replacement in chronically neglected polyarthritic patients: Two case reports. J Orthop Surg (Hong Kong) 2000;8:75-81. [Crossref] [PubMed]
Cite this article as: Hafez M, Hamza H, Essa RA. Multiple joint reconstructions in one patient: computer-assisted simultaneous procedures. Ann Joint 2017;2:12.