Percutaneous femoroplasty with perioperative nursing consultation relieves pain in patients with metastatic hip tumor
Introduction
The most frequent skeletal site of cancer metastasis is the pelvis (20%), followed by the lumbar spine (14%) and long bones (13%) (1,2). Cancer metastasis to the proximal femoral bone can cause severe pain and pathologic fracture, which significantly compromises patients’ quality of life (QoL) (3). Percutaneous vertebroplasty has been shown to be effective in the treatment of bone weakness caused by cancer metastasis in the cervical, thoracic, and lumbar vertebra (4), and was effective in treating vertebral fractures caused by malignant metastases (5). With percutaneous vertebroplasty, bone pain due to cancer metastasis can be relieved in approximately 80–95% of patients (3,4).
Percutaneous femoroplasty (PFP) through percutaneous perfusion of bone cement was developed first in China to treat proximal femoral lesions due to metastatic tumor. This PFP technique has been used to good therapeutic effect in patients with metastatic cancer (6).
It is well known that perioperative nursing is crucial for successful operative outcomes (7), especially when a new procedure is applied. In these cases, it is necessary to explain the surgical procedure in detail to patients and their families. Furthermore, patients with metastatic cancer require humanistic and psychological care, and early psychological intervention is particularly important.
In the present study, we investigated the effect of perioperative nursing and PFP with regard to the pain of patients with cancer metastasis in the proximal femoral bone.
Methods
The clinical study was approved by the Ethical Committee of The Fourth Hospital of Hebei Medical University (No. 2017), and all participants signed an exhaustive informed consent form after being informed of the benefits and risks of the procedure.
Inclusion and exclusion criteria
Inclusion criteria (8): moderate to severe pain rated 5 or more on the 10 point visual analogue scale (VAS), due to metastasis in the proximal femur (trochanter, neck, or head) or a high risk of fracture according to Mirels scale (>8 points) or severe osteoporosis according to the WHO and a Karnofsky score of more than 50%. Osseous metastatic disease was diagnosed by pelvis radiography and pelvic computed tomography (CT). Exclusion criteria: femoral fracture or image by CT demonstrating loss of the cortical bone, patients with coagulation disorders, and those who were not eligible for interventional procedures after an anesthetic and cardiology pre-assessment.
Preoperative nursing
Pre-surgical consultation was provided to all patients to assess their psychological readiness, help patients and their family members understand the operation, and alleviate anxiety and fear of the operation. Perfusion of bone cement through percutaneous puncture in the treatment of proximal femoral metastatic tumor is a new technology in China. Therefore, we thoroughly explained the procedural process to patients and their families, with the help of radiographs and surgical instruments. All patients underwent physical examination and lab tests before surgery, including a bleeding test and history of drug allergy.
Appropriate nursing care before surgery
The nurse was responsible for checking the accuracy of patient information, filling out the institutional operation room safety form, preparing the infusion port, and positioning the patient on the operating table, with the affected lower limb extended and the contralateral limb slightly flexed. The fluoroscopy and monitoring equipment were set up in preparation for puncturing and injecting bone cement. All patients were given 5 mg intravenous dexamethasone and blood oxygen saturation was monitored before perfusion with the bone cement.
Surgical protocol
The bone cement was prepared before surgery in accordance with the manufacturer’s instructions. The bone cement was loaded into a pressurized syringe to ensure that enough material would be injected into the proximal femoral osteolytic lesion. After administration of local anesthesia, the bone cement was injected into the proximal femur, from a site 2–3 cm inferior to the greater trochanter. Fluoroscopy was used to adjust the needle angle until it entered into the site of cancer metastasis within the proximal femur. The volume of bone cement injected was from 6 to 12 mL, depending on the area of the lesion area. After the bone cement injection was completed, the needle was extracted.
Patients were requested to maintain the original surgical position for 15 minutes, to allow the bone cement to solidify before they returned to the wards. Two patients felt dysesthesia after the operation. After proper treatment, the dysesthesia subsided.
Evaluation of pain relief and QoL
The nurse asked patients to judge the pain level of the lower limb. Pain intensity was evaluated according to the VAS. VAS scores were from 0 to 10 (0= absence of pain, 10= unbearable pain). Barthel Index of Activities of Daily Living (BIADL) was used to evaluate QoL, respectively. Both scales were recorded before the operation, and afterward at 1 week, and 3 and 6 months.
Data analysis
The data were recorded in a Microsoft Excel 2010 spreadsheet and analyzed. Mean and standard deviation values are reported for quantitative variables. To analyze the association between the main results of clinical effectiveness (pain relief according to VAS scores and improved functionality according to BIADL scores) at different time points, a generalized linear model with analysis of variance for repeated measures was applied. Statistical analyses were completed using SPSS 21.0 software (SPSS, Inc., Chicago, IL, USA). The patient-reported pain levels before and after the operation were compared using t-tests. P values less than 0.05 were considered to indicate statistically significant differences.
Results
Thirty patients with different primary cancers were recruited, including 13 men and 17 women. Their ages ranged from 35 to 65 years. Primary cancers involved the lung in 10 patients, breast in 9, esophagus in 7, liver in 2, and 2 had cervical cancer. All these primary cancers were diagnosed upon pathological examination. All 30 patients had cancer metastasized to the hip joint, 24 with proximal femoral metastases and 6 with the acetabulum involved.
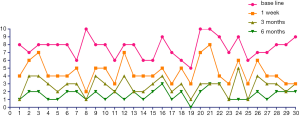
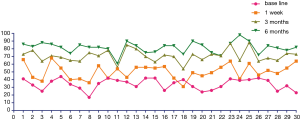
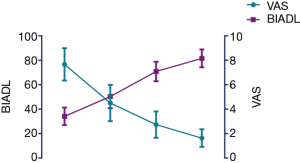
Several patients were nervous about this novel operation. However, they were comforted after the nurse consultation, suggesting the essential appropriate care of nursing in patient care before surgery. Prior to the PFP procedure, patients’ proximal femoral pain was moderate-to-severe, with a mean VAS score of 7.09±1.10, BIADL score of 34.15±7.15 (Table 1). The PFP intervention was associated with a significant reduction in pain at one week (4.42±1.36; P<0.05). The pain indices were further decreased at 3 months (2.62±0.94) and 6 months (1.60±0.66) (Figure 1). The mean BIADL score increased significantly from 34.15±7.15 preoperatively to 50.46±9.43 at 1 week postoperatively and 70.87±7.97 at 3 months, 81.68±7.26 at 6 months postoperatively (both P<0.01) (Figure 2). Figure 3 showed a remarkable improvement of QOL as the pain released.

Full table
No patient experienced severe complications after the PFP and prior to discharge from the hospital. All of the patients, with proximal femoral cancer metastases, walked well 6 months after PFP.
Discussion
The present study assessed the effectiveness of PFP with perioperative nursing in relieving the hip joint pain and improving QOL of patients with cancer metastasis. We found that this combination of treatment significantly reduced the levels of pain and in this regard improved patients’ QoL. Supporting patients’ emotional and psychological conditions are the major goals of perioperative nursing, and these have been to have an important role in the successful outcome of surgery (9,10). Our study is in agreement with these studies.
The proximal femur is rich in vasculature and the second most common site of bone metastasis (11). PFP represents a promising treatment option for alleviating the pain and weakness associated with metastatic lesions of the femur. Kaneko et al. proposed that certain cases of proximal femora with metastases could be repaired by removal of the lesion and filling the resulting defect with PMMA (12). Plancarte et al. applied a percutaneous technique for repairing metastatic sites in the head, neck, and proximal femur with bone cement in a retrospective and non-uniform case series involving 15 patients who were monitored for 2 months (13). And consistent with the results previously in our previous research (6). The following recommendations should ensure success, based on our experience.
Firstly, the psychological issues of the patient should be addressed. We found in the present study that patients with proximal femoral bone metastases are unwilling to cooperate, which was likely due to psychological vulnerability, as reported previously (14). Therefore, adequate nursing care must be provided to the patient. Secondly, the intraoperative fluoroscopy of the PFP procedure is different from that in percutaneous vertebroplasty. PFP treatment requires adjustment of the patient’s position. Because the patient’s bone is fragile, caution must be taken to avoid bone fracture when positioning the patient. Thirdly, because the amount of bone cement injected is large, it should be mixed to a semi-liquid consistency before it is loaded into pressurized syringes. Finally, the patient’s pulse oximetry should be closely monitored during surgery. If side effects appear, hormonal treatment must be given immediately to reduce the risk of pulmonary embolism.
Proximal femoral metastases can cause severe pain (3,15), and render patients bedridden for a long time. If the patient has bone pain for more than 2 weeks, muscle atrophy may occur due to limited movement. Therefore, functional exercise should be recommended. We propose the following guidelines for functional exercise. Firstly, ankle pump-like movement such as flexion, extension, and rotation of the ankles should be on the schedule within 24 h of PFP. Secondly, there should be exercise of the quadriceps and femoris muscles by opposing resistance to extend knees 48 h after the PFP operation. Thirdly, patients should be encouraged to stand by the bedside or walk with crutches in the presence of a nurse 72 h after the PFP. The amount of activities can be gradually increased, based on the patient’s condition.
The present study only compared the outcomes before and after PFP surgery in patients with cancer metastases to the proximal femur. Although PFP was found effective in relieving pain caused by cancer, we cannot draw a conclusion as to whether the PFP procedure is better than other modalities. To do this, we would need to compare the outcomes among patient groups who underwent different operative procedures. In addition, we only performed the PFP procedure in a small number of patients. A larger population or more studies in different clinical settings are needed to validate the results before PFP can be widely used in China.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.04.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethical Committee of The Fourth Hospital of Hebei Medical University (No. 2017) and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Seo HJ, Kim GM, Kim JH, et al. 18F-FDG PET/CT in hepatocellular carcinoma: detection of bone metastasis and prediction of prognosis. Nucl Med Commun 2015;36:226-33. [Crossref] [PubMed]
- Feng H, Wang J, Guo P, et al. CT-Guided percutaneous femoroplasty (PFP) for the treatment of proximal femoral metastases. Pain Physician 2016;19:E767-73. [PubMed]
- Piccioli A, Rossi B, Scaramuzzo L, et al. Intramedullary nailing for treatment of pathologic femoral fractures due to metastases. Injury 2014;45:412-7. [Crossref] [PubMed]
- Shimony JS, Gilula LA, Zeller AJ, et al. Percutaneous vertebroplasty for malignant compression fractures with epidural involvement. Radiology 2004;232:846-53. [Crossref] [PubMed]
- Yang Z, Yang D, Xie L, et al. Treatment of metastatic spinal tumors by percutaneous vertebroplasty versus percutaneous vertebroplasty combined with interstitial implantation of 125I seeds. Acta Radiol 2009;50:1142-8. [Crossref] [PubMed]
- Feng H, Feng J, Li Z, et al. Percutaneous femoroplasty for the treatment of proximal femoral metastases. Eur J Surg Oncol 2014;40:402-5. [Crossref] [PubMed]
- Sjöstedt L, Hellström R, Stomberg MW. Patients' need for information prior to colonic surgery. Gastroenterol Nurs 2011;34:390-7. [Crossref] [PubMed]
- Plancarte R, Guajardo J, Meneses-Garcia A, et al. Clinical benefits of femoroplasty: a nonsurgical alternative for the management of femoral metastases. Pain Physician 2014;17:227-34. [PubMed]
- Emotional WJ. Emotional and psychological preoperative preparation in adults. Br J Nurs 2002;11:567-75. [Crossref] [PubMed]
- Wang K. Nursing as a first surgical assistant. Nurs N Z 2014;20:26-7. [PubMed]
- Mundy GR. Mechanisms of bone metastasis. Cancer 1997;80:1546-56. [Crossref] [PubMed]
- Kaneko TS, Skinner HB, Keyak JH. Feasibility of a percutaneous technique for repairing proximal femora with simulated metastatic lesions. Med Eng Phys 2007;29:594-601. [Crossref] [PubMed]
- Plancarte-Sanchez R, Guajardo-Rosas J, Cerezo-Camacho O, et al. Femoroplasty: a new option for femur metastasis. Pain Pract 2013;13:409-15. [Crossref] [PubMed]
- Gold JI, Douglas MK, Thomas ML, et al. The relationship between posttraumatic stress disorder, mood states, functional status, and quality of Life in oncology outpatients. J Pain Symptom Manage 2012;44:520-31. [Crossref] [PubMed]
- Feng H, Wang J, Xu J, et al. The surgical management and treatment of metastatic lesions in the proximal femur: A mini review. Medicine (Baltimore) 2016;95:e3892 [Crossref] [PubMed]
Cite this article as: Li J, Wang J, Xu J, Zhang J, Feng H. Percutaneous femoroplasty with perioperative nursing consultation relieves pain in patients with metastatic hip tumor. Ann Joint 2017;2:14.