
Identification and treatment of RAMP lesions in anterior cruciate ligament-injured knees
Introduction
The medial meniscus acts as a secondary stabilizer to anterior tibial translation. Part of this stabilization stems from the meniscotibial ligament that attaches the posterior margin of the medial meniscus to the tibial plateau as well as the link between the posteromedial meniscus and the knee capsule (1,2). With anterior cruciate ligament (ACL) injury, concomitant lesions of the medial meniscus occur in approximately 47% to 61% of cases (3,4). In 1982, Strobel et al. initially coined the term “Ramp Lesion” to describe a tear in the attachment between the posteromedial meniscus and knee capsule in ACL deficient knees (5). Since that time, multiple authors have described similar injuries to the posteromedial meniscocapsular attachment in conjunction with ACL injury. The reported incidence of ramp lesions varies between 9.3–17% in the published literature (6,7). Further, it is hypothesized that in a chronically ACL deficient knee, the medial meniscus experiences increased loads with repetitive anterior tibial subluxations and rotation as it engages with the medial femoral condyle to block anterior translation of the tibia. This repeated stress across the posterior meniscocapsular attachment can lead to tears in the posterior horn of the medial meniscus or the development of ramp lesions. The chronicity of the ACL injury in conjunction with the mechanism of injury is supported by multiple studies. First, Sonnery-Cottet intraoperatively identified significantly more ramp lesions in ACL deficient knees repaired after 6 weeks compared to acute ACL reconstruction before 6 weeks (8). In agreement, Song et al. observed significantly more ramp lesions in knees undergoing ACL reconstruction greater than 6 months from the time of injury (9). These publications suggest that earlier treatment for ACL injury may help prevent the development of meniscal ramp lesions. But, despite increasing publications and diagnosis of ramp lesions, the biomechanical role of the soft tissue attachments to the posteromedial meniscus has yet to be firmly established.
Clinical tests
There are no specific clinical tests for diagnosing ramp lesions. Other common physical examination tests for diagnosing meniscal tears are not sensitive nor specific for identifying ramp lesions. Tests for rotatory knee laxity and anterior tibial subluxation may suggest an increased risk for the development of a meniscal ramp lesion, but this has not been reported in the literature.
Imaging
Plain films likely are to be normal, however, one may see tibial subluxation in a very unstable knee. MRI is important in evaluating the posteromedial meniscocapsular junction as physical exam findings are non-specific. However, the literature is limited in its assessment of the evaluation of ramp lesions on MRI. Studies have not reported specific statistical parameters or methods of evaluation in evaluation of ramp lesions on MRI. In the limited studies, reported sensitivity ranges from 0% to 77% (6,7,10). At the 2015 American Academy of Orthopaedic Surgery (AAOS) Annual Meeting, one abstract found 44 ramp lesions in 337 patients (13.1% incidence), 33 being identified on MRI (77% sensitivity). One possible weakness of this study is the authors made their conclusions by reviewing MRI reports only, and many times meniscocapsular injuries are not closely evaluated on routine MRI and can be missed (10). An ePoster at the 2013 ISAKOS Biennial Congress found 23 ramp lesions on arthroscopy in 92 knees (25%) by using a posteromedial portal. Fourteen of these 23 knees (61%) had meniscocapsular separation on MRI. This group found that T2*-weighted gradient-echo sagittal image was best in identifying this pathology. The study also reported that younger patients more commonly have ramp lesions and recommend routine evaluation with a posteromedial viewing portal, as implications in missing a ramp lesion may be significant (11). In both studies, the methods of evaluation on MRI were not presented and no other parameters or statistics (i.e., specificity, positive predictive value, or negative predictive value) were reported.
Direct evaluation of the posteromedial meniscus and capsule is the gold standard in diagnosis. However, studies evaluating the most accurate arthroscopic technique to identify ramp lesions are limited. One study of 302 ACL reconstructions investigated the use of a posteromedial portal and found a prevalence of ramp lesions to be 40% of all medial meniscal injuries. The authors also found a high rate (16.8%) of missed meniscocapsular injury before the addition of a posteromedial portal. They therefore recommend the addition of a posteromedial portal for viewing as well as debridement of the posteromedial meniscocapsular region as lesions can also be “hidden” under a membrane-like structure (8). One study of 39 patients who underwent ACL reconstruction had the posteromedial meniscus evaluated sequentially with an anterolateral portal, intercondylar view, and a posteromedial portal. This study found that the addition of the intercondylar view identified 4 more lesions not seen from the anterolateral portal, while the posteromedial portal found 2 additional lesions not seen on either previous view. The authors therefore conclude that both the intercondylar view as well as a posteromedial portal should be routine during ACL reconstruction, particularly in delayed surgery (12). While MRI is good in identifying posterior medial meniscocapsular injuries, arthroscopic evaluation remains the gold standard, as the implications of untreated meniscocapsular injuries are unknown.
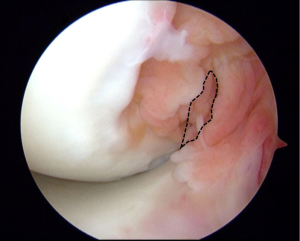
Arthroscopic diagnosis
Visualization of meniscal ramp lesions is challenging during standard diagnostic arthroscopy, hence the moniker, “hidden lesion” (8). The posteromedial compartment of the knee must be fully visualized and thoroughly inspected to avoid a missed diagnosis. Multiple techniques are described to achieve adequate visualization of ramp lesions. The Gilchrist view is the most common. The arthroscope is inserted through the anterolateral portal through a narrow triangular space bordered inferiorly by the posterior cruciate ligament (PCL), medially by the femoral condyle, and laterally by the tibial spine (Figure 1). Applying a valgus force to the knee first in flexion, then in extension will bring the posteromedial corner of the knee into view with a 30° arthroscope. In some cases, a 70° may be necessary. In a series of 125 medial meniscus tears associated with ACL injury, Sonnery-Cottet et al. found that 40% (50) of these medial meniscal tears were ramp lesions. Of these 50 lesions, 29 were diagnosed during exploration of the posteromedial compartment after standard arthroscopic exploration. The remaining 21 were diagnosed after minimal debridement and probing of the posteromedial compartment (8). This group concludes that establishing a posteromedial portal is essential in order to completely identify zone 3 meniscal body tears and ramp lesions. Additional exploration of the posteromedial compartment after standard diagnostic arthroscopy should be considered in all knees, specifically in chronic ACL deficient knees.
Self-healing potential
The posterior knee capsule and zone 3 of the posterior horn of the medial meniscus maintain a good vascular supply that increases self-healing potential. Eliminating rotatory and sagittal instability of the knee with ACL reconstruction alleviates shear stress across the meniscus suggesting repair of a ramp lesion is no longer required and can be treated with simple abrasion and trephination (13).
Biomechanical studies
The biomechanical literature regarding ramp lesion is sparse. Peltier et al. described the biomechanical behavior of ACL deficient cadaveric knees after transection of the meniscocapsular attachment of the knee followed by additional transection of the meniscotibial ligament (14). Transection of the meniscocapsular junction did not significantly influence the kinematics of the ACL deficient knee. In contrast, transection of the meniscotibial ligament increased anterior-posterior translation and internal-external rotation in all degrees of flexion.
Stephens and Amis et al. demonstrated the biomechanical relevance of the posterior meniscocapsular attachments in nine cadaveric knees (15). The anterior translation and external rotation of the tibia were significantly increased with ACL deficiency and a posteromedial meniscocapsular tear. But, in the ACL deficient knee with a posteromedial meniscocapsular tear, anterior and external rotational laxity was not restored with ACL reconstruction alone. Only after repair of the posteromedial meniscocapsular injury did knee kinematics return to the intact, native knee state. This study emphasizes the biomechanical importance of the posterior meniscocapsular junction for stabilizing persistent tibiofemoral laxity with ACL deficiency. Further biomechanical studies should investigate the influence of ramp lesions on ACL grafts, tibiofemoral laxity, and articular cartilage contact pressure changes.
Repair techniques
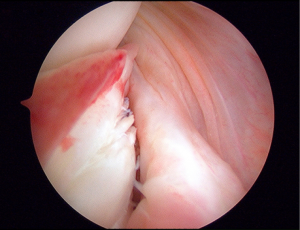
All-inside repair technique
The arthroscopic all-inside suture repair of ramp lesions of the medial meniscus through a posteromedial portal is a commonly utilized repair technique for meniscal ramp lesions. A trans-notch view through the anterolateral portal allows sufficient visualization of the posteromedial corner of the knee. This view can be enhanced with flexion of the knee to 90° and internal rotation of the tibia in order to posteriorly sublux the medial compartment of the knee and bring the posteromedial meniscus into greater view. A needle is introduced just above the hamstring tendons, 1 cm posterior to the medial tibiofemoral joint line to establish the posteromedial portal. Transillumination helps to avoid nerves and veins. The needle must be introduced from outside to inside, in the direction of the lesion, under arthroscopic visualization to avoid damage to nearby neurovascular structures. After establishing the posteromedial portal, superficial debridement and trimming of the tissue should be performed to appropriately visualize the lesion, along with rasping of the posterior meniscus to promote vascularization and a healing response.
A suture hook device loaded with non-absorbable braided composite suture is inserted through the posteromedial portal into the knee capsule at the area of the ramp lesion. In chronic cases where the knee capsular tissue has become attenuated, the suture hook can be used to plicate the capsule to the level of the meniscus. The suture hook is then inserted through the peripheral zone of the meniscus, and the suture shuttled through. Starting along the lateral margin of the ramp lesion and working medially maintains better visualization of the posteromedial meniscus until the last suture is tied. A sliding knot is cinched down with the knot pusher to the posterior border of the meniscus and cut. A distance of 5 mm between sutures is adequate for fixation.
In a case series of 132 patients, Thaunat et al. reported that arthroscopic meniscal repair of ramp lesions during ACL reconstruction with a suture hook device through a posteromedial portal is a safe procedure with a low rate of revision surgery and a high rate of meniscus healing, especially in tears limited size (16). This study is limited because no second look arthroscopy was performed and there was no control group for comparison. Outcome variables were limited to clinical examination findings and patient reported outcomes. Unfortunately, there are limited publications reporting patient outcomes after all-inside arthroscopic ramp lesion repair. More level I evidence is required before further recommendations can be provided.
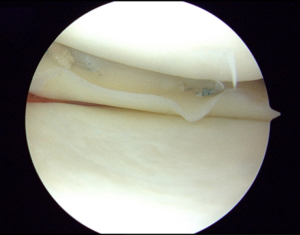
Ramp repair with meniscal repair systems
In contrast to the all-inside repair technique, ramp lesion repair with meniscal repair systems, such as the arthroscopic FasT-Fix device (Smith & Nephew Endoscopy, Andover, MA, USA), is performed through the anterolateral portal for visualization and anteromedial portal for instrumentation (Table 1). Initially, the first implant is inserted into joint capsule, traversing underneath the meniscus. The second implant is then inserted into zone 3 of the undersurface of the posterior horn of the medial meniscus. In chronic cases with attenuated capsular tissue, a curved applicator can be used to lift the knee capsule back to the level of the meniscus. With this technique, it is necessary to switch between direct visualization of the anteromedial compartment of the knee and a trans notch view of the posteromedial corner of the knee through the anterolateral portal. Li et al. described this repair technique and reported significant increases in clinical outcome scores in a sample size of 23 patients with simultaneously meniscal ramp lesion repair and ACL reconstruction (17).
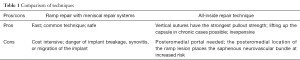
Full table
A combination of both techniques is performed by the senior author (VM) in select cases and combined the advantages of both techniques (Figures 2-4).

Postoperative restrictions
There is no standardized postoperative rehabilitation protocol for ramp lesion repair. In the setting of an ACL reconstruction, standard protocol for ACL reconstruction rehabilitation is recommended. For isolated ramp repair or in conjunction with other meniscal repair, restricting passive knee flexion to less than 90° is recommended in order to alleviate shear stress and compression across the posterior horn of the medial meniscus body. Partial weight bearing in a knee immobilizer for the first 6 weeks should be enforced.
Conclusions
Meniscal ramp lesions continue to be an evolving pathology in orthopaedics. Whereas the mechanism of injury has been more clearly defined in the recent literature, the proper protocol for diagnosis and treatment remains a question. MRI has demonstrated a strong potential ability to adequately identify meniscal ramp lesions, but arthroscopic diagnosis remains the gold standard. The posteromedial portal and Gilchrist view provide good visualization for identifying meniscal ramp lesions intraoperatively. Both the meniscal repair system and all-inside repair technique have shown good clinical outcomes in patients undergoing ACL reconstruction and ramp lesion repair. But, this literature remains limited and cannot be used to draw definitive conclusions for treatment recommendations. More high level of evidence studies must be completed to determine optimal diagnosis and treatment algorithms.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Freddie H. Fu and Jeremy M. Burnham) for the series “Trends in ACL Reconstruction” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: The series “Trends in ACL Reconstruction” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Thompson WO, Fu FH. The meniscus in the cruciate-deficient knee. Clin Sports Med 1993;12:771-96. [PubMed]
- Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am 1979;61:56-62. [Crossref] [PubMed]
- Ahldén M, Samuelsson K, Sernert N, et al. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med 2012;40:2230-5. [Crossref] [PubMed]
- Noyes FR, Chen RC, Barber-Westin SD, et al. Greater than 10-year results of red-white longitudinal meniscal repairs in patients 20 years of age or younger. Am J Sports Med 2011;39:1008-17. [Crossref] [PubMed]
- Strobel MJ. Knee Joint — Special Part. Manual of Arthroscopic Surgery. Berlin: Springer Berlin Heidelberg, 2002;97-669.
- Liu X, Feng H, Zhang H, et al. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med 2011;39:832-7. [Crossref] [PubMed]
- Bollen SR. Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: a previously unrecognised association. J Bone Joint Surg Br 2010;92:222-3. [Crossref] [PubMed]
- Sonnery-Cottet B, Conteduca J, Thaunat M, et al. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med 2014;42:921-6. [Crossref] [PubMed]
- Song GY, Liu X, Zhang H, et al. Increased Medial Meniscal Slope Is Associated With Greater Risk of Ramp Lesion in Noncontact Anterior Cruciate Ligament Injury. Am J Sports Med 2016;44:2039-46. [Crossref] [PubMed]
- Edgar C, Ware JK, Obopilwe E, et al. Posteromedial meniscocapsular tear: prevalence, detection sensitivity, biomechanics, and repair technique. Available online: http://aaos2015.conferencespot.org/58906-aaos-1.1965581/t004-1.1971711/f004-1.1971712/a096-1.1971713/se81-1.1971728 [Accessed October 13, 2016].
- Hatayama K, Kimura M, Ogoshi A, et al. Ramp Lesion Associated with Anterior Cruciate Ligament Rupture. Available online: https://www.isakos.com/meetings/2013congress/onsite/AbstractView?EventID=7751 [Accessed October 13, 2016].
- Peltier A, Lording TD, Lustig S, et al. Posteromedial meniscal tears may be missed during anterior cruciate ligament reconstruction. Arthroscopy 2015;31:691-8. [Crossref] [PubMed]
- Liu X, Zhang H, Feng H, et al. Is It Necessary to Repair Stable Ramp Lesions of the Medial Meniscus During Anterior Cruciate Ligament Reconstruction? A Prospective Randomized Controlled Trial. Am J Sports Med 2017;45:1004-11. [Crossref] [PubMed]
- Peltier A, Lording T, Maubisson L, et al. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc 2015;23:2967-73. [Crossref] [PubMed]
- Stephen JM, Halewood C, Kittl C, et al. Posteromedial Meniscocapsular Lesions Increase Tibiofemoral Joint Laxity With Anterior Cruciate Ligament Deficiency, and Their Repair Reduces Laxity. Am J Sports Med 2016;44:400-8. [Crossref] [PubMed]
- Thaunat M, Jan N, Fayard JM, et al. Repair of Meniscal Ramp Lesions Through a Posteromedial Portal During Anterior Cruciate Ligament Reconstruction: Outcome Study With a Minimum 2-Year Follow-up. Arthroscopy 2016;32:2269-77. [Crossref] [PubMed]
- Li WP, Chen Z, Song B, et al. The FasT-Fix Repair Technique for Ramp Lesion of the Medial Meniscus. Knee Surg Relat Res 2015;27:56-60. [Crossref] [PubMed]
Cite this article as: Pfeiffer TP, Murphy CI, Arner JW, Musahl V. Identification and treatment of RAMP lesions in anterior cruciate ligament-injured knees. Ann Joint 2017;2:17.


