Total knee arthroplasty after osteotomies around the knee
Introduction
Osteotomies around the knee are procedures that have shown excellent results to treat unicompartmental arthritis in young patients. In the majority of these patients, these techniques achieve success in pain relief and increasing knee function with preservation of proprioception and native joint delaying the need for knee replacement by a decade or more (1,2). Despite the good results that the literature has reported, the satisfaction of patients generally deteriorates with time and some of these inevitably require further treatment with total knee arthroplasty (TKA) for progression of osteoarthritis and involvement of the other compartments. Several studies reported that at 10 years follow-up, TKA was necessary in 23% of patients previously treated with osteotomies (3). However conversion of osteotomy to TKA is more surgically demanding compared with a primary prosthesis for a number of reasons, including skin incision, hardware removal, residual tibial and femoral deformities and balancing of soft tissue.
Surgical incision
The knee joint is vulnerable to multiple parallel incision and skin necrosis is an important issue in this surgery. The blood supply come from the lateral branches of genicular arteries and the lateral flap is more vulnerable also because lymph fluid drainage is mainly located on medial side, therefore previous scars must be considered with attention. Certainly multiple parallel incisions and incision convergence must be avoided and when this is not possible and a new incision is required it should be at least 6 cm away from older incision (4). If the osteotomy is performed in severe valgus deformed knee a lateral incision and a lateral arthrotomy can be used.
After incisions, the first procedure is hardware removal, in fact staples or plates may be at risk of impingement of tibial and femur stems. Some authors prefer to use implant without stems preserving bone stock that may be valuable for these patients if they require revision arthroplasty and avoiding potential complications such as stress shielding or pain at stem tip, however without stems implants have not the ability to bypass areas of least resistance due to the screw holes and plates with a greater risk of fractures during surgery and early postoperative peri-prosthetic fractures (2).
There is not a uniform consensus about the timing to remove them, 2 stages versus 1 stage procedure. Advantages to use a two stage procedure are the possibility to perform samples to bacteriological studies in case of doubt of local infection, on the other hand this choice increase costs of hospitalization and patient discomfort. In both cases the surgeons have to pay attention to not damage proximal insertion of the anterior tibialis muscle in case of precedent closing-wedge high tibial osteotomy (HTO) or tibial insertion of medial collateral ligament (MCL) and pes anserinus tendons in case of opening-wedge HTO.
Joint exposure
An accurate joint exposure can be difficult for presence of scar tissue, tibial or femur deformities, especially in case of malunion that is more frequent like complication in closing-wedge HTO, and patella baja (5). In fact, the most common challenge during conversion TKA after failed HTO is to evert the patella and the risk of patellar tendon damage or avulsion it should not be underestimated.
When a TKA after osteotomy becomes necessary, the surgeons have to do many different observations regarding mechanical alteration of the patellofemoral joint during planning of surgery. The evidence of patella baja after HTO is not uncommon and these changes seem related to the surgical technique and postoperative care (6).
Theoretically, closing-wedge HTO distalized the joint line and increases the height of patella but Scuderi et al. (7) reported that 76% to 89% of 66 patients how had an HTO with knee immobilization post-operatively had a measurable patella baja. To support the relations between patella baja and post-operative treatment with cast immobilization Westrich et al. (8) in their paper study the patella height in 98 patients that had underwent an HTO with secure and rigid internal fixation and early knee mobilization. In this paper, there was a significant reduction in the incidence of this issue compared with knee immobilization after surgery, exactly 9% versus 53% respectively.
This condition does not appear to be related with distal femur osteotomies. The theoretical changes in the patella mechanics after these interventions are a decrease in quadriceps tendon length and a decrease of Q angle. Effectively the typical femur varus osteotomy involves only the medial side of quadriceps tendon and only a little part of the over-length and in literature mechanical changes of patellofemoral joint following the femoral osteotomy largely are ignored (6). Kosashvili et al. in their study analyzed 22 consecutive distal femoral varus osteotomies converted to TKA at a mean follow-up of 5 years and they had seen four cases of patella baja with an Insall-Salvati (IS) index lesser than 0.8 and six additional knees with an IS index of between 0.8 and 1.0, but there were no association between patella baja and failure of the index arthroplasty (2).
However, if the patellar eversion is too much difficult, it should be necessary an additional procedure to approach the joint like a lateral retinaculum release, plasty of quadriceps tendon, tibial tubercle osteotomy or rectus snip. Bastos Filho et al. had shown that 25% of conversion TKA after HTO needed an additional procedure during surgical approach (9). Similar results are shown by Gill et al. that commonly adopted quadriceps snip and V-Y plasty in 23% of patients treated (10).
Tibial and femoral resections
HTO could be responsible for translation of tibial metaphysis on the diaphysis with alterations of mechanical axis and this is more frequent in case of tibial nonunion or malunion. Conversion TKA requires good understanding of these deformities and a good consideration of any residual correction defect that could be the consequence of hypercorrection and subsequent valgus knee o hypocorrection with persistence of varus.
Considering the coronal plane the surgeon that perform the tibial resection has to evaluate the local anatomy, because performing a tibial cut perpendicular to the mechanical axis can lead to impingement between tibial cortex and, when used, tibial stem (4). This issue is very frequent and it can be solved using undersized implants or using stems with medial or lateral offset (11). In the first example, it is easier to make mistakes like uncovering the lateral compartment or of overhang on the medial side.
On the sagittal plane an increase or decrease of the tibial slope must be corrected. This is mandatory to achieve long-term implants survival with a good range of motion and stability. In case of increased tibial slope our implant could be instable with a recurrence of tibial anterior translation and instability in flexion, on the other hand a decreased slope reduces ROM of the knee in flexion and induces posterior subluxation of tibia. Generally, some authors recommend to minimize the depth of the bone resection, Meding et al. reported that the average of tibial bone resection was 3.3 mm in a conversion group after HTO compared to 7.5 mm in a group without previous HTO (12). Thus, if a good flexion is achieved and the extension gap need to be increased, that may be achieved by release of posterior capsule rather than an additional resection (2).
Rotating deformity influences the relationship of the patella in the condylar groove and the stability of the patella to track properly. In conversion TKA an eventual alteration on axial plane must be evaluated correctly and is helpful in determining the centralization of patella. Thus in case of clinical examination shows an important difference between affected and unaffected knee in internal and external rotation a computed tomography and an accurate pre-operative planning must be done. For severe malunion, a derotating osteotomy or medial transfer of the tibial tuberosity may be necessary (4).
Soft tissue balance
A previous HTO produces an extra-articular deformity that influences soft tissue tension, in fact after bone resection an important medial and lateral imbalance is frequently observed. In many cases, a posterior cruciate-substituting or a posterior cruciate-retaining component after proper alignment with soft tissue balancing can provide satisfactory stability and knee function.
In case of persistence of varus-deformities after HTO with instability, the knee presents in most cases a contracture on MCL associated with a flexion contracture of the pes anserine tendon and consequently an attitude of flexed knee not reducible, while Knees with valgus instability present medial collateral laxity and achieve satisfying soft tissue balance is technical demanding and in many cases an insufficiency of medial compartment is persistent.
Furthermore, tibial and femoral osteophytes are incorporated in soft tissue and their removal requires an extensive release, which can lead to residual instability. Thus, the surgeons have to select the adapt prosthesis type.
Different recent works yet recommend to take in account the use of a condylar constrained devices when it is particularly complex to gain adequate soft tissue balance.
Survival rate and outcomes
The reports on TKA after distal femur osteotomy in the literature have not showed objective outcomes and often presented very small numbers of patients.
Nelson et al. published a report with outcomes of eleven patients that need a TKA after distal femur varus osteotomy gathered from three different centers. With a mean follow-up of 5 years the authors found improvements in mean arc of motion from 82° to 106° post-operatively, also good results are showed when the authors evaluated the knee society score that increased from 35 point pre-operatively to 84 and when they evaluated the functional score that improved in mean from 49 point to 68 (13).
Kosashvili et al. published a larger series than previous authors, with 21 patients and 22 knees that performed an intervention of TKA after a mean time of 13 years from the osteotomy of distal femur. Their results showed an increased arc of motion from 94° to a mean of 114° at final follow-up. Knee society score increased from a mean of 52 points to a mean of 91 points and knee society function score increased from a mean of 52 points to a mean of 64 points.
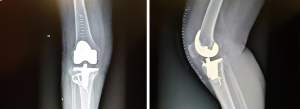
In literature, more data have been reported focusing on conversion TKA after HTO, but the results are more various with many authors that confirm less satisfaction and others that don’t notice any differences between TKA after HTO than TKA as primary implants (Figures 1,2).
Haslam et al. affirmed that there were no significant differences found when comparing the overage hospital for special surgery score between two groups of patients, HTO group and control group, but they revealed a significantly less flexion in the TKA after HTO group (91°) as compared with the control group (106°). Moreover, the authors performed more reoperation like revision or arthrodesis after arthroplasty in HTO group (14).
Parvizi et al. had evaluated 166 total knee replacements that were performed in 118 patients who had a prior proximal tibial osteotomy. In this study the mean knee society pain score improved from 34.5 to 82.9 point at the time of the latest follow-up, the mean knee society function score improved from 44.6 to 88.1 points and the mean arc of motion improved significantly from 68.9° (range, 20°to 120°) to 100.5° (range, 80° to 130°). However, they reported a higher incidence of aseptic loosening in a 15 years follow-up study, revision of TKA was performed in thirteen knees and eight knees that had failed to achieve an adequate range of motion required manipulation following the knee arthroplasty (15).
But these results are very heterogeneous, in fact Haddad and Bentley showed comparable results at 6 years’ follow-up although patella baja was present in 60% of patients in conversion TKA. The authors detected no statistically significant differences between two groups of patients (patients who had undergone previous HTO compared with patients that had undergone primary TKA) in term of function score, pain scores, total KS score or HSS scores and the overall outcomes remains good to excellent in most cases (16).
Conclusions
Total knee replacement is the appropriate treatment in the failure of tibial or femoral osteotomy. Certainly, this procedure can’t be compared to a first implant because the surgeons perform an already complex intervention with a multi-operated joint. The literature in many cases showed that clinical results are generally inferior to those of primary TKA. Thus, patients should be informed that this procedure is more complex, that results could be less satisfactory and complications more frequent.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “Osteotomies and partial replacement in early osteoarthritis of the knee”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.05.11). The series “Osteotomies and partial replacement in early osteoarthritis of the knee” was commissioned by the editorial office without any funding or sponsorship. LS served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Joint from Jun 2016 to May 2018. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hutchison CR, Cho B, Wong N, et al. Proximal valgus tibial osteotomy for osteoarthritis of the knee. Instr Course Lect 1999;48:131-4. [PubMed]
- Kosashvili Y, Safir O, Gross A, et al. Distal femoral varus osteotomy for lateral osteoarthritis of the knee: a minimum ten-year follow-up. Int Orthop 2010;34:249-54. [Crossref] [PubMed]
- Insall JN, Hood RW, Flawn LB, et al. The total condylar knee prosthesis in gonarthrosis. A five to nine-year follow-up of the first one hundred consecutive replacements. J Bone Joint Surg Am 1983;65:619-28. [Crossref] [PubMed]
- Cerciello S, Vasso M, Maffulli N, et al. Total knee arthroplasty after high tibial osteotomy. Orthopedics 2014;37:191-8. [Crossref] [PubMed]
- Bae DK, Song SJ, Yoon KH. Total knee arthroplasty following closed wedge high tibial osteotomy. Int Orthop 2010;34:283-7. [Crossref] [PubMed]
- Closkey RF, Windsor RE. Alterations in the patella after a high tibial or distal femoral osteotomy. Clin Orthop Relat Res 2001;51-6. [Crossref] [PubMed]
- Scuderi GR, Windsor RE, Insall JN. Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am 1989;71:245-8. [Crossref] [PubMed]
- Westrich GH, Peters LE, Haas SB, et al. Patella height after high tibial osteotomy with internal fixation and early motion. Clin Orthop Relat Res 1998;169-74. [Crossref] [PubMed]
- Bastos Filho R, Magnussen RA, Duthon V, et al. Total knee arthroplasty after high tibial osteotomy: a comparison of opening and closing wedge osteotomy. Int Orthop 2013;37:427-31. [Crossref] [PubMed]
- Gill T, Schemitsch EH, Brick GW, et al. Revision total knee arthroplasty after failed unicompartmental knee arthroplasty or high tibial osteotomy. Clin Orthop Relat Res 1995;10-8. [PubMed]
- Nagamine R, Inoue S, Miura H, et al. Femoral shaft bowing influences the correction angle for high tibial osteotomy. J Orthop Sci 2007;12:214-8. [Crossref] [PubMed]
- Meding JB, Keating EM, Ritter MA, et al. Total knee arthroplasty after high tibial osteotomy. A comparison study in patients who had bilateral total knee replacement. J Bone Joint Surg Am 2000;82:1252-9. [Crossref] [PubMed]
- Nelson CL, Saleh KJ, Kassim RA, et al. Total knee arthroplasty after varus osteotomy of the distal part of the femur. J Bone Joint Surg Am 2003;85-A:1062-5. [Crossref] [PubMed]
- Haslam P, Armstrong M, Geutjens G, et al. Total knee arthroplasty after failed high tibial osteotomy long-term follow-up of matched groups. J Arthroplasty 2007;22:245-50. [Crossref] [PubMed]
- Parvizi J, Hanssen AD, Spangehl MJ. Total knee arthroplasty following proximal tibial osteotomy: risk factors for failure. J Bone Joint Surg Am 2004;86-A:474-9. [Crossref] [PubMed]
- Haddad FS, Bentley G. Total knee arthroplasty after high tibial osteotomy: a medium-term review. J Arthroplasty 2000;15:597-603. [Crossref] [PubMed]
Cite this article as: Risitano S, Bistolfi A, Sabatini L, Galetto F, Massè A. Total knee arthroplasty after osteotomies around the knee. Ann Joint 2017;2:26.