Modern clinical decision-making in total joint arthroplasty
Introduction
Over the past decade, the process of clinical decision-making and the patient-physician relationship have continued to evolve. Much of this evolution has been brought about by legislation encouraging greater use of decision-making models. Historically, patients have not had an active role in medical decision-making, but as patients are increasingly expected to take on a more active role in medical decision-making and care, healthcare providers have implemented patient-centric methodologies promoting SDM models (1). This shift has been facilitated by the increasing amount of information available to patients through the internet, patient education applications, and public quality reporting instruments (2). Moreover, with the changing climate in medicine, there is particular interest in patient satisfaction and compliance with prescribed interventions (3-5). Patients are now increasingly expected to take actions to improve their health and reduce risks associated with surgical procedures (6). This engagement is sometimes referred to as patient activation. In this review, we will describe the three decision-making models, describe factors influencing modern clinical decision making in orthopaedic surgery, and describe the role of patient activation.
Decision making models
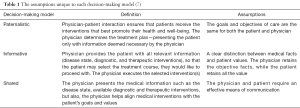
There are three commonly described types of decision-making models: paternalistic, informative, and SDM (Table 1) (7). The paternalistic decision-making model is one in which physicians make treatment decisions for patients (7). The paternalistic model assumes that the patient and physician have aligned interests. In this model, physicians make healthcare decisions for patients independent of their unique preferences (1,7). In contrast, the informed decision-making model equips patients with the necessary objective facts regarding disease state, available diagnostic and therapeutic interventions so that an informed decision can be made by the patient (7). The physician’s role is only to disseminate the information and implement the selected treatment pathway (7,8). The SDM is similar to the informative decision-making model in that the physician presents all clinically relevant information. However, the patient and the physician also aligns treatment modalities with the patients’ health goals and personal values, and treatment decisions are made together, as a team (4,5,7).
SDM
The concept of SDM is not a new one. It was envisioned more than 30 years ago by a Reagan-era Presidential Commission promoting the integration of ‘shared decision-making’ as a way of improving communication and informed consent in healthcare (9). However, it was not until the passage of the Patient Protection and Affordable Care Act (ACA) of 2010, which authorized the Center for Medicare and Medicaid Innovation (CMMI) to test SDM models designed to better inform patients’ of medical decision-making, that efforts to institute it became mandated. Numerous randomized trials have consistently demonstrated the effectiveness of SDM models within healthcare. A recent Cochrane review of 115 studies indicated that patients who used decision making aids had less decisional conflict regarding their disorder, more active role in decision making, and a greater likelihood of receiving care aligned with their values (10). Thus, if SDM models are properly implemented, as suggested by the Institute of Medicine (11), healthcare providers and patients may expect improved outcomes and higher patient compliance.
Patient activation
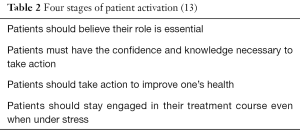
It has become increasingly apparent that patients must take steps to optimize their health and outcomes associated with surgical and medical procedures. A major barrier to the implementation of SDM has been patient activation, or an individual’s propensity to engage in adaptive health behaviors (12). If the SDM healthcare strategy is to be, successfully implemented patient activation is necessary. This is particularly true in orthopaedic care, which requires a high degree of patient-directed interventions, such as occupational and physical therapy participation. A study by Andrawis and colleagues (12) reported that total joint arthroplasty (TJA) candidates with higher preoperative patient activation were associated with better pain relief, reduced symptoms, and higher satisfaction following surgery. In another report, a national expert consensus panel and patient focus group feedback indicated that if the four stages (Table 2) of patient activation are implemented, healthcare costs may be reduced (13,14). In addition, patients can modify behavior or treat comorbid conditions reducing risks associated with elective orthopaedic procedures. If these recommendations are followed, patients may expect superior outcomes, higher satisfaction rates, lower healthcare costs, while also achieving a better understanding of their healthcare needs. Thus, the patient and orthopaedic surgeon should promote patient activation as part of the SDM model with the aim of improving the quality and reliability of orthopaedic care delivered.
Implementation of SDM in TJA
SDM requires effective delivery of information pertaining to the disease state, as well as the risks and benefits associated with diagnostic and therapeutic interventions. Physicians must strategize on how to deliver treatment information so that patients are able to make informed decisions using the validated patient-centered instruments designed to optimize patient outcomes in both the pre- and post-operative setting. It is important that patients and physicians understand the purpose behind each instrument so that they can be used to enhance the evaluation and decision making process.
Risk-stratification instruments are being increasingly used with SDM models. However, many of these tools are difficult for patients to interpret [e.g., Charlston Comorbidity Index (CCI) and American Society of Anesthesiologists (ASA) score]. It is crucial that preoperative screening instruments be interpretable to patients and realistic to implement within the clinical setting. Several risk calculators, including the American Joint Replacement Registry’s (AJRR) Total Joint Risk Calculator (15), are available and allow orthopaedic surgeons and patients to more precisely calculate an individual patient’s risk profile for certain complications (e.g., infection and mortality) when undergoing specific procedures. These instruments provide clinicians with a ‘teachable moment’ further enhancing the patient-physician relationship, while strengthening the SDM process. These risk stratification calculators may also provide the patient with the opportunity they need to institute risk reduction behaviors optimizing their health status. Most importantly, health benefits achieved during the preoperative medical optimization process may provide the patient with the necessary knowledge and tools for long-term healthy living. One such example may be patient participation in a tobacco cessation programs prior to elective TJA resulting in decreased short-term risks associated with surgery, and perioperative and long-term benefits if the behavior is continued. The SDM model enables physicians to solicit patient buy-in enabling patients to vest in their own care through the modification of risk factors and improvement in their overall health.
Advantages and disadvantages of SDM
Several studies have evaluated the effects of SDM in orthopaedic patients. In a study by Bozic and colleagues (16), two cohorts of patients were randomized to either a SDM intervention or the standard of care. The SDM cohort received decision-making aids consisting of digital video discs and booklets, whereas the control cohort received information regarding the surgeons’ practice. The study demonstrated that the use of SDM with decision-making aids benefited both patients and surgeons, enhancing informed decision-making, patient confidence and satisfaction. A recent study by Sepucha and colleagues (17) demonstrated that orthopaedic patients who met SDM criteria had significantly higher improvements in disease-specific and overall quality of life. In addition, these patients were more likely to be satisfied with the treatment, reported less regret with the selected treatment course, and were satisfied with the level of pain relief. Another study by Stacey and colleagues (18) demonstrated that in patients with osteoarthritis considering TJA, the implementation of SDM and collection of PROs in the clinical setting is feasible, improves decision quality, and patient knowledge. These studies demonstrate that SDM can be practically implemented within the clinical setting and have a positive impact on patients and the decision making process.
Despite these positive outcomes, there are some potential disadvantages, which warrant further investigation. The costs associated with designing and implementing decision-making aids (e.g., pamphlets, digital video discs, and electronic applications) can be considerable, especially within the confounds of a small group practice. Additionally, many of the decision-making instruments require the collection of unique patient reported outcomes (PROs) over the duration of treatment. These PROs may consist of questions pertaining to the patient’s perception on: quality of life, functional ability, and perception of pain. The data obtained through these PRO instruments must then be stored in a retrievable manner. Thus, requiring institution-wide implementation of advanced electronic medical record (EMR) systems further straining resources (19). Perhaps the most significant drawback associated with SDM is that quality metrics are difficult to compile and objectively evaluate. Yet, as medicine continues to shift from a pay-for-service to a performance-based system, payers will request that providers document SDM practices and the PROs corroborating these decisions (20). In spite of the challenges, patients who participate in SDM consistently select more conservative interventions and are more invested in improving health behaviors and modifying risks prior to surgery; potentially reducing episode of care costs, improving PROs, and satisfaction (20-22).
Innovative approaches at implementing SDM
Many innovative patient-centered programs have been developed to educate and optimize TJA candidates. Several technology platforms take advantage of smart phones and wearable devices to connect patients and their care teams via streamlined electronic applications. Through these applications, patients communicate and provide clinical information in real-time. Moreover, built in tactile sensors and scheduled administration of PROs can track progress, notifying clinicians if patients are not progressing as expected. Through these innovative decision-making aids, orthopaedic surgeons are now able to remotely monitor patients, and ensure clinical goals are achieved while maintaining patient autonomy and strengthening the physician-patient relationship through the integration of real-time data. However, prior to the widespread implementation, further studies are needed to determine how these resources can be best allocated as well as the optimal platforms for implementing these emerging technologies.
Conclusions
As the healthcare system continues to evolve, it is crucial that clinicians, patients, and payers work together enhance patient activation and decision-making. SDM instruments and technological advances provide an important opportunity for achieving these aims and should continue to be explored in order to optimize patient and physician decision-making.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.05.09). JS reports other from smith and Nephew, other from Zimmer/Biomet, personal fees from Pacira, personal fees from Horizon Pharmaceuticals, other from AAHKS, from AAOS, other from Hip and Knee Society, other from PCORI, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Charles C, Whelan T, Gafni A. What do we mean by partnership in making decisions about treatment? Bmj 1999;319:780-2. [Crossref] [PubMed]
- Slover J, Shue J, Koenig K. Shared decision-making in orthopaedic surgery. Clin Orthop Relat Res 2012;470:1046-53. [Crossref] [PubMed]
- Porter ME. A strategy for health care reform--toward a value-based system. N Engl J Med 2009;361:109-12. [Crossref] [PubMed]
- Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions. Am J Prev Med 1999;17:285-94. [Crossref] [PubMed]
- Kaplan SH, Greenfield S, Gandek B, et al. Characteristics of physicians with participatory decision-making styles. Ann Intern Med 1996;124:497-504. [Crossref] [PubMed]
- Bronson WH, Fewer M, Godlewski K, et al. The Ethics of Patient Risk Modification Prior to Elective Joint Replacement Surgery. J Bone Joint Surg Am 2014;96:e113 [Crossref] [PubMed]
- Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. JAMA 1992;267:2221-6. [Crossref] [PubMed]
- Vranceanu AM, Cooper C, Ring D. Integrating patient values into evidence-based practice: effective communication for shared decision-making. Hand Clin 2009;25:83-96. vii. [Crossref] [PubMed]
- Wynia M, Moulton B, Elwyn G. Shared Decision Making And The Use Of Patient Decision Aids. Health Affairs Blog, December 17, 2014.
- Stacey D, Légaré F, Col NF, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2014;CD001431 [PubMed]
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US); 2001.
- Andrawis J, Akhavan S, Chan V, et al. Higher Preoperative Patient Activation Associated With Better Patient-reported Outcomes After Total Joint Arthroplasty. Clin Orthop Relat Res 2015;473:2688-97. [Crossref] [PubMed]
- Hibbard JH, Stockard J, Mahoney ER, et al. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39:1005-26. [Crossref] [PubMed]
- Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood) 2013;32:207-14. [Crossref] [PubMed]
- Second American Joint Replacement Registry Annual Report on Hip and Knee Arthroplasty Data. 2014. Available online: http://www.ajrr.net/images/annual_reports/AJRR_2014_Annual_Report_final_11-11-15.pdf
- Bozic KJ, Belkora J, Chan V, et al. Shared decision making in patients with osteoarthritis of the hip and knee: results of a randomized controlled trial. J Bone Joint Surg Am 2013;95:1633-9. [Crossref] [PubMed]
- Sepucha K, Freiberg AA, Mangla M, et al. Shared Decision Making in Orthopaedic Care Leads to Better Health Outcomes: A Prospective Cohort Study. Paper presented at: Annual Meeting of the American Academy of Orthopaedic Surgeons; March 2017; San Diego, CA.
- Stacey D, Hawker G, Dervin G, et al. Decision aid for patients considering total knee arthroplasty with preference report for surgeons: a pilot randomized controlled trial. BMC Musculoskelet Disord 2014;15:54. [Crossref] [PubMed]
- Ayers DC, Zheng H, Franklin PD. Integrating patient-reported outcomes into orthopaedic clinical practice: proof of concept from FORCE-TJR. Clin Orthop Relat Res 2013;471:3419-25. [Crossref] [PubMed]
- Oshima Lee E, Emanuel EJ. Shared decision making to improve care and reduce costs. N Engl J Med 2013;368:6-8. [Crossref] [PubMed]
- Arterburn D, Wellman R, Westbrook E, et al. Introducing decision aids at Group Health was linked to sharply lower hip and knee surgery rates and costs. Health Aff (Millwood) 2012;31:2094-104. [Crossref] [PubMed]
- Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2011;CD001431 [PubMed]
Cite this article as: Edusei E, Anoushiravani AA, Slover J. Modern clinical decision-making in total joint arthroplasty. Ann Joint 2017;2:29.