
Closing wedge tibial osteotomy: is it an actual procedure nowadays?
Introduction
High tibial osteotomy (HTO) is a common and widely accepted procedure in orthopaedic surgery.
First introduced by Jackson et al. (1), HTO has become more popular by Conventry (2) since the mid-1960s as a treatment option for medial compartment osteoarthritis of the knee usually associated to varus deformity. The goals of HTO are:
- To reduce knee pain by transferring weight-bearing loads to the relatively unaffected compartment;
- To increase the life span of the knee joint, by slowing or stopping the destruction of the medial joint compartment. This could delay the need of a joint replacement.
Although the improvements of partial and total knee arthroplasty (TKA), HTO remains a good option in some patients. Everybody agree in saying that in this surgery, in order to obtain satisfactory results, it is mandatory to have an appropriate patient selection and precise surgical planning (3-6).
HTO could be used to manage not only the primary varus deformity, but also double and triple varus deformity. In a double varus knee there is a varus bone deformity associated with a central ligaments injury and/or a lateral ligaments injury. A triple varus consists of a varus deformity accompanied by anterior and posterior cruciate ligaments injuries, and a posterolateral corner lesion (7).
Many techniques have been described for performing HTO, whether alone or in combination with other procedures: lateral and medial closing wedge, opening wedge, barrel vault (dome) osteotomy, “en chevron” osteotomy are some examples, but opening (medial) and closing (lateral) wedge HTO are the most commonly used. The latter is achieved by the removal of a wedge-shaped piece of bone from the lateral side of the proximal tibia, created by two osteotomies (Figure 1).
The disadvantage of this procedure is the necessity to have an osteotomy of the fibula or the disruption of the proximal tibiofibular joint, with the aim to free the fibula from the tibia.
In our practice, in the last years, we have almost forsaken the closing wedge HTO, that have been replaced by opening wedge osteotomy and partial knee replacement.
Indications: patient selection, contraindications, clinical exam, radiographic evaluation
The key point to achieve successful results after a HTO procedure is the correct selection of the patients. There is not a general rule to select, but some broad criteria can be described. The criteria for a closing osteotomy are the same for an opening one. The ideal patient for a tibial osteotomy is an active, young thin patient, ranging from 50 to 60 years old, with a unicompartmental medial knee pain and a stable knee without symptoms related to patellofemoral joint.
As usually in orthopaedics, the surgeon should consider the physiological age rather than the chronological one. Despite the good results showed by Langlais and Thomazeau (8) about HTO in low-grade arthritis after 70 years, we reserve this procedure to patients younger than 60 years. The activity level is the best predictor for the postoperative outcome (9). As we know, unicompartmental knee replacement is a complete pain relief option, and the surgeon has to carefully consider the patient’s expectation and his needs, job and life style.
Sometimes focusing the attention to the relative and absolute contraindications is helpful to choose properly the possible treatment (Table 1). A literature review (10-13) shows which conditions are related with worse outcomes: arthrosis of others compartment, in addition to that of the medial side; age more than 65 years; a decreased range of motion (<120°).
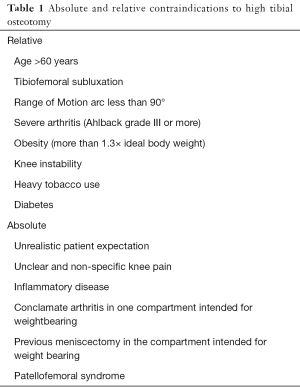
Full table
Preoperative planning
In our practice it is mandatory having a complete radiographic report that includes bilateral weight bearing AP views in full extension, Rosenberg views with 45° knee of flexion, lateral views and tangential patellar views or skyline views. An Insall-Salvati index for the patellar height must be carefully evaluated, because the choice between an opening or closing HTO may depend on it.
In the suspicion of associated lesions, a MRI could be performed. CT scan is helpful in identifying early signs of arthritis and lateral bone attrition, but it is not always necessary.
The surgical planning is similar to that for the opening wedge HTO. We usually refer to the osteotomy planning described by Dugdale et al. (14). The weight-bearing line (WBL) is defined as the one which starts from the center of the femoral head and ends to the middle of the ankle. The deviation of the WBL can be quantified as a percentage of the tibia plateau width. In a varus knee the WBL could be less than 0% if it passes outside the joint. The goal of the corrective osteotomy is to lead the WBL in the point corresponding to the 62.5% of the tibial plate’s width. In young patients with a minimal degeneration of the medial compartment, correction to a neutral mechanical axis is planned. The preoperative planning is described in the Figure 2.

Surgical technique
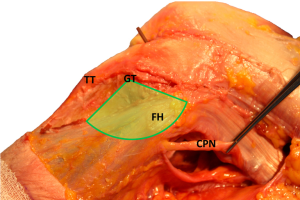
The patient is supine, on a radiolucent operating table. A sandbag is positioned beneath the gluteal region, to have a slight internal rotation. The tourniquet is applied around the proximal thigh. The surgeon with his team must check the position of the patient and all the instrumentation. The knee must be free to move up to 90° of flexion. We usually use an adhesive electrode on the center of the femoral head and one in the middle of the tibiotarsal joint line. The intermittent fluoroscopy must be in the surgery room. If there are associated injuries such as meniscal tear or cruciate ligament rupture, an arthroscopy surgery could be performed before the opening one. According to Rubel (15), we mark the Gerdy’s safe zone, to identify where there is not the risk of injuring the peroneal common nerve. From this study we know that the distance between Gerdy’s tubercle and fibular head determines the radius of a 100° arc, that represents an anatomical safe area (16,17) (Figures 3,4).

We use a short oblique incision on the lateral aspect of the tibia, from the fibular head to the tibial tubercle. The iliotibial tract is splitted just above the Gerdy’s tubercle, anteriorly to the fibular collateral ligament.
The proximal tibiofibular joint is opened. With a small osteotome, the medial half of the fibular head is excised with an oblique direction. This allows the sliding of the remaining fibula during the varus correction.
Tibialis anterior muscle is then elevated from the tibia and a retractor is gently inserted behind the posterior aspect of the tibia. Another retractor is placed anteriorly, to protect the patellar ligament. Now the surgical field is safe and there are no “danger zones”. Based on the preoperative measurements and with the use of fluoroscopy, two Kirchner wires are inserted. The first pin is placed parallel to the tibial plateau, 2–2.5 cm below the articular joint line. The second pin is inserted distally in an oblique fashion in order to meet the first pin at the medial tibial cortex. The distance between the two entry points depends on the pre-operative planning.
With an oscillating saw and then with an osteotome, paying attention not to interrupt the medial cortex, the two cuts are made. The osteotomy is performed parallel to the joint line in the sagittal plan, and the tibial slope in not changed. The wedge bone is then removed with a curette.
With the knee in full extension and with the help of an assistant, a valgus stress is applied in order to have a correct osteoclasis. With the intermittent fluoroscopy the medial hinge is checked and the mechanical axis is verified. If a long alignment rod is not available, a diathermy cable can be used to check the knee alignment fluoroscopically. Once achieved the correct alignment, the osteotomy is stabilized with two staples or with a plate. Some authors (18) suggest the use of two Kirschner wires to stabilize the cut, but we prefer to use a more stable fixation: in our practice, often in overweight patients, we insert two wires to have just a temporary fixation of the cut.
Once the tibia is fixated, the integrity of the medial hinge is re-checked fluoroscopically with dynamic images. A radio stereometric analysis indicates that a fracture in the opposite cortex increases the risk of lateral displacement of the distal segment, with a subsequent poorer outcome. Kohn and Pape (19) discovered that a correction of more than 8°, with a removal of a large wedge size, usually induces a non-displaced fracture caused by an exceed in the bone plastic deformation capacity. In the rare occasions where we need to correct more than 8°, we usually make drilled holes in the opposite cortex with a Kirchner wire, to induce a greenstick fracture and avoid the risk of a displaced or intra-articular fracture.
Finally, the removed bone is placed near the osteotomies, and the tourniquet is slowly released. A very accurate haemostasis and a deep drainage are essential to avoid postoperative complications such as compartment syndrome. After the wound closure, a slight compressive dressing is placed.
After 24 hours the drainage is removed, a hinged knee brace is positioned and active knee motion can be started as tolerated. This fast return to active mobility reduce the incidence of patella baja (20). Antero-posterior and lateral X-Ray is performed 24 hours after surgery and weight bearing AP views and lateral views are obtained after 8 weeks. For the first 8 weeks we allow touchdown weight bearing with two crutches, followed by progressive full weight bearing.
Complications
The best way to avoid complication starts from an appropriate patient selection, a good surgical technique and an accurate knowledge of the anatomy. The complications rate with this procedure ranges widely. Wu et al. (21) have reported an overall complications rate of 5.6%, whilst Naudie et al. (13) had reported a 34% rate in their series. HTO is proved to be a relatively simply technique with poor consequences. However, complications may occur and they should be well known by the surgeon and patients. They include:
- Varus deformity recurrence;
- Over- and under-correction;
- Altered patellofemoral kinematics;
- Patellofemoral malalignment;
- Increased q-angle and patellar subluxation;
- Fractures;
- Change in tibial inclination;
- Increased joint line obliquity;
- Delayed union and non-union;
- Peroneal nerve and popliteal artery injury;
- Leg shortening;
- Compartment syndrome;
- Infections;
- Thromboembolism.
Fracture
During any osteotomy a controlled fracture is produced with the aim to achieve the desired correction without destabilising the fragments. In lateral closing osteotomy it is recommend to end the osteotomy 5–10 mm from the opposite and conserve the medial cortex: the goal is to provide stability and maximise the contact area of the tibial segments (22,23). Nevertheless, during the procedure a fracture through the opposite cortex or into the intra-articular fragments can be produced: this is undesirable as it may lead to the instability of the proximal fragment with a mal-union or non-union result. The literature describes the intra-articular fracture occurring during HTO as a more severe complication than a medial cortex fracture, and it is reported in 10–20% of closing wedge against 11% in opening wedge osteotomy (24). As described before, and according to Engel et al. (25), sometimes we weaken the medial cortex with a drill hole to induce a greenstick fracture during correction and to prevent intra articular fractures. If we have any doubt we usually perform a CT scan in order to recognize the line fracture and decide the correct postoperative management.
Delayed union and non-union
Non-union after closing wedge osteotomy is uncommon. The incidence has been reported to be less than 1% (26). To prevent non-union it is fundamental to consider general factors as smoking, peripheral vascular status, nutritional status, strict adherence to postoperative protocols and comorbidities such as diabetes. These elements underline the importance of a proper patient selection.
Peroneal nerve palsy and vascular lesions
Nerve and vascular lesions can occur during any operating process. Peroneal nerve injury is reported to occur with percentages between 3.3% and 11.9% (24). To reduce a direct nervous damage a careful lateral dissection, atraumatic surgery manoeuvres (as much as possible) and a fibular osteotomy >15 cm distal to the fibular head are recommended. It is also important to avoid an indirect vascular lesion, usually resulting from a high compartment pressure: in literature it is described the importance of haemostasis and adequate drainage to limit the frequency of this consequence.
Direct vascular injury following HTO is rarer: less than 1% of all cases. If the osteotomy is performed with 90 degrees of knee flexion, it has been demonstrated a risk reduction of popliteal artery damage.
Compartment syndrome
The exact incidence of compartment syndrome after HTO is unknown but literature shows high possibility of elevated anterior compartment pressures after surgery. The risk may increase if the osteotomy is combined with an arthroscopically-assisted ligament reconstruction.
Infections
Infections are a common problem of all surgery techniques. The incidence of deep infection after lateral closing wedge HTO ranges from 0 to 4% (10,21,26); on the contrary, septic arthritis or chronic osteomyelitis have been seldom reported.
Thromboembolism
The incidence of deep vein thrombosis ranges from 2–5% after HTO (24). It is mostly associated to immobilization during and after surgery; for this reason it is recommended to consider preventive measures to minimize the risk.
Patellar height changes
Closing wedge HTO is associated with an incidence rate between 7.6% and 8.8%. of postoperative patella baja. This condition is caused by contracture of the patellar ligament associated with conventional cast immobilisation. It is important to prevent it because of its association with anterior knee pain and a more difficulty in performing a subsequent TKA. This explain the importance of an aggressive postoperative mobilisation.
Results
Quite a few survival analysis have been reported in literature, but a correct interpretation of these data is difficult because of the heterogeneity of fixation devices (Kirchner wires, angular stability plate, cast immobilization and no internal fixation, etc.), postoperative rehabilitation protocols and outcomes analysed.
Overall, the results are very good in the first years; considering a longer follow up, instead, they tend to decline gradually. Rudan et al. (12) reported 80% rates of good or excellent results after 79 closing wedge osteotomy, with a follow up period of 5.8 years. In patients with no satisfactory results the causes were under-correction and patellofemoral arthritis. Akizuki et al. (27), with a technique and a postoperative protocol similar to that described before, obtained survival rates of 97% and 90% after 10 and 15 years respectively. Naudie et al. (13) reported that 75% of patients did not require a TKA after 5 years, almost 50% at 10 years, and 39% at 15 years. The survival rates of Tang et al. (28) were 90% at 5 years, 75% at 10 years and 67% at 15 and 20 years of follow up. Ivarsson et al. (10), performed almost 100 closing HTO, using staples and cast immobilization for 6 weeks. In three out of four patients the results were good or acceptable at 5.7 years after surgery. Finally, Flecher et al. (29) reported a survival rate of 85% at 20 years of follow up, considering revision surgery as the endpoint. He believes that the most important predicting factors are an age older than 50 years, and a preoperative arthritis.
The scientific community agrees in saying that poor outcomes are correlated with under- or overcorrection (30,31), patellofemoral arthritis (12), a decreased range of motion (13), lateral tibial thrust and of course severe arthritis (10).
In a short term follow up study Keene et al. (32), showed that mild arthritis of the lateral compartment does not compromise the results of HTO. Nevertheless, we do not recommend this procedure in such condition.
The correction accuracy of the mechanical axis relative to the preoperative situation is one of the most important factors that predicts the final outcome. In a recent review performed by Van den Bempt et al. (33), it has been demonstrated that this accuracy is very low. Among the 23 studies analysed, a HTO closing technique was chosen only in 5. For example, Bae et al. (34) showed a successful rate only in 50% of patients with a standard technique; the percentage increased in the computer navigated group. Since the long term results mostly depend by the precision of the correction, the authors underlined the necessity of a careful preoperative planning and a progressive gentle correction. Furthermore, computer navigated tools seem to be helpful during surgery, but they are not widespread among orthopaedic community. It is well known that open wedge osteotomy is more accurate in axis correction: Hankemeier et al. (31) revealed a difference between the preoperative planning and the postoperative correction angle (3° of discrepancy in the closed osteotomy group, and a significant less difference in the open one). Gaasbeek et al. (35), reported an overcorrection tendency in closing osteotomy and, on the contrary, an under correction tendency in the open HTO, although there were not significant differences. Also Magyar et al. (36), showed their results after an osteotomy with external fixator: despite the discomfort for the patient, with this technique they were able to better control the mechanical axis correction with a gentle distraction. We believe that with an open HTO it is easier to achieve a precise correction, not least because after the two osteotomies were done it is very difficult to obtain slight modifications.
In the young and active population one of the most important outcomes is the return to work and sport. As already described by Ekhtiari et al. (37), there is only one study reporting the return to sport rate after closing HTO, in which all the 23 patients (100%) returned to sport after surgery, and 22 (96%) of them gained an equal or greater level. Concerning the return to work rate, evaluating by 3 studies, more than 90% of patients went back to work within 12 months. For those who did a physically demanding activity the mean time away from work was 10 months, but in the other workers it could be about 3 months.
Closing vs. opening wedge HTO
Good results have been reported for opening and closed wedge osteotomy (38,39) with a pain reduction and improved function at 1 year of follow up (3).
As previously discussed, the pre-operative selection and the accuracy in the surgical technique are essential factors to reduce complications and obtain long-lasting results.
If closed wedge osteotomy is associated with fibular osteotomy and tibiofibular joint release with a possible peroneal nerve injury, on the other hand medial opening wedge osteotomy is correlated with a higher risk of non-union, collapse and eventually need of bone graft (38-40).
It is well demonstrated that closing wedge osteotomy has the advantage of a more accurate correction with less morbidity, but leads to a more challenging conversion to TKA as a drawback (41). There are not significant differences in functional outcomes or in survival rates of TKA performed after closing or opening wedge osteotomy (42) as well as in the risk of TKA revision after the two operations. During a TKA following a CWHTO a lateral release may be needed, whereas in OWTHO a medial release occurred with higher probability (43). TKA after lateral closing wedge osteotomy could require a more prolonged rehabilitation and cause a greater reduction in the postoperative ROM.
CWHTO could result in a posterior tibial slope decrease or in a posterior cruciate ligament hyperextension that is associated with anterior instability. OWTHO, on the contrary, could elicit a posterior tibial slope increase with an overload on the anterior cruciate ligament (ACL).
Closing wedge HTO vs. unicondylar knee arthroplasty
Patients suffering from unicompartmental osteoarthritis could also be treated with a unicondylar joint replacement (UKA). The survivorship rate published in literature (44) ranges from 80% to 98% at 10 years of follow up, and a progressive increase use of the UKA has been observed (45). The age of patients is an important factor to be taken into account for the correct indication: patients with 55–60 years may be treated with both options. Only few studies compared UKA with closing wedge HTO (44,46-51).
Petersen and Metzlaff (44) evaluated 25 patients treated with UKA and 25 patients treated with closing wedge HTO with a minimum follow up of 5 years. They reported 1 case of revision surgery in both group, and no infection complications. In the HTO group, 92% of the patients underwent to an implant removal. Petersen described a significantly better KOOS subscore in UKA group, with benefit in pain, symptoms and quality of life. The subscore referred to sports recovery was better in UKA group, even if it did not reach a statistical difference.
In 2001 Stukenborg-Colsman et al. (49) published a prospective randomized study in which compared 28 patients treated with UKA (Aesculap) to 32 patients treated with a closing HTO fixed with a five-hole two-thirds tubular plate. In both groups the mean age was 67 years. Sxiteen patients underwent a revision to TKA: 10 were HTO after an average time of 3.5 years, and 6 were UKA after an average time of 4.5 years. The authors observed 9 complications after a HTO despite only 2 in the UKA group. They concluded that if a correct mechanical axis is achieved, HTO can have as good results as the UKA, especially in over 60 years patients.
Broughton et al. (47) asserted that the key factor for a satisfactory result depends on the mechanical axis correction: they stated that, at final follow up, a valgus deformity was observed more in HTO group than in UKA one.
In the last prospective randomized study published, the authors evaluated the range of motion, pain and time-distance variables of gait. They did not report any statistical difference between the two techniques at the final follow up of 5 years. Despite this, in the first months they documented a better gait analysis in the UKA group.
Mancuso et al. (51), in his systematic review, concluded that in patients with ACL lesion there is not an increase in complication rate due to UKA surgery, whereas in HTO and LCA reconstruction the complication rate is around 20%.
There is not a universal consensus in literature about which technique is superior, despite some studies showed better results in UKA patients.
TKA after closing wedge HTO
The results of HTO can change over the time despite of initial success and patient’s satisfaction (52,53).
Some cases may require conversion to TKA because of arthritis worsening (30,54), loss of correction angle, loss of pain relief (4).
In a 10-year follow-up study reported, TKA was necessary in 23% of patients treated with HTO (55).
Various factors have been supposed to be associated with the survival of HTO: age, body mass index, gender, pre-operative range of motion, osteoarthritis grade and post-operative correction angle.
The presence of a prior closing wedge HTO complicates the performance and the surgeon has to confront himself with several difficulties:
- Tibial metaphyseal deformity;
- Limited knee motion;
- Rotational deformity;
- Previous cutaneous incision;
- Hardware removal;
- Soft tissue mismatches;
- Patellar high.
A pre-operative plan becomes essential to anticipated possible problems: the strategy to approach must be determined before surgery.
It is generally accepted that TKA after closing wedge HTO is technically more demanded. However, the previous HTO has no deleterious effects on the outcome of a secondary TKA (44-51,56-64). Surgeons need to evaluate various factors and technical difficulties during conversion TKA, including surgical approach, anatomical deformities, ligament imbalance, and a correct selection of prosthesis types.
It is not unusual that the surgical approach to the proximal tibial metaphysis and the patellar eversion prove to be demanding, especially when there are a patella baja, adhesions around the osteotomy site and infrapatellar adhesions (57-59).
Sometimes it becomes necessary “special” approach techniques, such as the V-Y plasty of the quadriceps, the quadriceps snip, the tibial tubercle osteotomy, the early release of the lateral retinaculum, the lateral parapatellar approach and/or the release of the patellofemoral ligament (57,58,60).
Bastos Filho et al. (43) found that the incidence of additional procedures for the approach during TKA after HTO, such as TTO or rectus snip, was 25% because the difficulties in patellar eversion.
The removal of previous osteotomy hardware can be done during the same TKA surgery or few weeks before. In most cases the surgeon prefers one single approach to avoid two anaesthetics, two surgeries and two hospitalizations. On the other hand, the double approach permits to start bacteriological exams during the first surgery, as to discover a possible infection.
When there is a concern regarding infections, two different operations are mandatory; this option should also be preferable when the hardware is voluminous or when the extraction looks difficult.
After a closed wedge HTO, a coronal and rotational tibial plateau deformities occur with a change in the posterior slope angle. The surgeon needs to be familiar with this possible anatomical variation correlated to the use of a correct TKA technique, and has to be able to resolve problems.
Regarding rotational deformities, the tibial axial malunion correction by modifying the position of the tibial component could be dangerous as it affects tibiofemoral and patellofemoral kinematics; for severe malunion, a derotational osteotomy or a medial transfer of tibial tuberosity can be proposed to improve the patellofemoral kinematic (61).
In closing wedge osteotomy, it can frequently be observed a lateral imbalance caused by bone resection: a previous CWHTO can produced, in fact, an extra articular deformity and a different soft tissue tension. Since the cut-off value for correctable deformities is not always predictable during the preoperative evaluation, preoperative stress radiographs can be helpful (61). Different rates of medial and lateral release in conversion TKA after open versus closing wedge HTO have been reported: these were 91.5% and 46.0% respectively in TKA after open wedge HTO, and 55.5% and 57.2% respectively in TKA after closing wedge HTO (43).
For conversion TKA after HTO, many authors recommend the use of the PCL substituting prosthesis because of PCL contracture, insufficiency, and postoperative stiffness. Hernigou et al. (62) reported good results after conversion TKA with a posterior- stabilized prosthesis but, because of the tibial bone defect, it is arduous to maintain an appropriate tension of PLC and a good extension gap after a CWHTO. Furthermore, patella resurfacing has been recommended as a routine procedure for the high risk of anterior knee pain and the high revision rate for a secondary resurfacing after the conversion TKA after HTO (63). Amendola and Bonasia (39) reported the results of 29 consecutive TKAs after failed HTO: three patients had persistent anterior pain that required a further arthroplasty of the patella performed, respectively, at 18, 19, and 27 months after the index arthroplasty, with a remarkable clinical improvement.
Conclusions
We strongly believe that closing HTO is an option for weight bearing axis correction, and the key point for a good outcome consists of a correct indication. In our ward the use of this technique decreased in the last years in favour to open HTO and UKA, with very satisfactory results.
We prefer open HTO for the less intra-operatory risk, and the possibility to better control the tibial slope. Furthermore, the increase difficulty in knee replacement revision surgery usually leads us to choose other options.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Luigi Sabatini) for the series “Osteotomies and partial replacement in early osteoarthritis of the knee” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.06.04). The series “Osteotomies and partial replacement in early osteoarthritis of the knee” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br 1961;43-B:746-51. [PubMed]
- Coventry MB. Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. a preliminary report. J Bone Joint Surg Am 1965;47:984-90. [Crossref] [PubMed]
- Yasuda K, Majima T, Tsuchida T, et al. A ten- to 15-year follow-up observation of high tibial osteotomy in medial compartment osteoarthrosis. Clin Orthop Relat Res 1992;186-95. [PubMed]
- Insall JN, Joseph DM, Msika C. High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Joint Surg Am 1984;66:1040-8. [Crossref] [PubMed]
- Scott WN, Clarke HD. The role of osteotomy 2003: defining the niche. Orthopedics 2004;27:975-6. [PubMed]
- Amendola A. Unicompartmental osteoarthritis in the active patient: the role of high tibial osteotomy. Arthroscopy 2003;19:109-16. [Crossref] [PubMed]
- Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 2000;28:282-96. [PubMed]
- Langlais F, Thomezeau H. Ostetomies du genou. In: Bach JF, Dorfmann H. editors. Enciclopedie medico-chirurgicale Technique Chirurgicales: orthopedie-traumatologie. Paris: Ed. Techniques, 1989: 1-23.
- Nagel A, Insall JN, Scuderi GR. Proximal tibial osteotomy. A subjective outcome study. J Bone Joint Surg Am 1996;78:1353-8. [Crossref] [PubMed]
- Ivarsson I, Myrnerts R, Gillquist J. High tibial osteotomy for medial osteoarthritis of the knee. A 5 to 7 and 11 year follow-up. J Bone Joint Surg Br 1990;72:238-44. [PubMed]
- Aglietti P, Rinonapoli E, Stringa G, et al. Tibial osteotomy for the varus osteoarthritic knee. Clin Orthop Relat Res 1983;239-51. [PubMed]
- Rudan JF, Simurda MA. High tibial osteotomy. A prospective clinical and roentgenographic review. Clin Orthop Relat Res 1990;251-6. [PubMed]
- Naudie D, Bourne RB, Rorabeck CH, et al. The Install Award. Survivorship of the high tibial valgus osteotomy. A 10- to -22-year followup study. Clin Orthop Relat Res 1999;18-27. [PubMed]
- Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res 1992;248-64. [PubMed]
- Rubel IF, Schwarzbard I, Leonard A, et al. Anatomic location of the peroneal nerve at the level of the proximal aspect of the tibia: Gerdy's safe zone. J Bone Joint Surg Am 2004;86-A:1625-8. [Crossref] [PubMed]
- Adkison DP, Bosse MJ, Gaccione DR, et al. Anatomical variations in the course of the superficial peroneal nerve. J Bone Joint Surg Am 1991;73:112-4. [Crossref] [PubMed]
- Dellon AL, Ebmer J, Swier P. Anatomic variations related to decompression of the common peroneal nerve at the fibular head. Ann Plast Surg 2002;48:30-4. [Crossref] [PubMed]
- Tuli SM, Kapoor V. High tibial closing wedge osteotomy for medial compartment osteoarthrosis of knee. Indian J Orthop 2008;42:73-7. [Crossref] [PubMed]
- Bonnin M, Amendola NA, Bellemans J, et al. editors. The knee joint: surgical techniques and strategies. Paris: Springer-Verlag Paris, 2012.
- Closkey RF, Windsor RE. Alterations in the patella after a high tibial or distal femoral osteotomy. Clin Orthop Relat Res 2001;51-6. [Crossref] [PubMed]
- Wu LD, Hahne HJ, Hassenpflug T. A long-term follow-up study of high tibial osteotomy for medial compartment osteoarthrosis. Chin J Traumatol 2004;7:348-53. [PubMed]
- Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am 1993;75:196-201. [Crossref] [PubMed]
- Bauer T, Hardy P, Lemoine J, et al. Drop foot after high tibial osteotomy: a prospective study of aetiological factors. Knee Surg Sports Traumatol Arthrosc 2005;13:23-33. [Crossref] [PubMed]
- Tunggal JA, Higgins GA, Waddell JP. Complications of closing wedge high tibial osteotomy. Int Orthop 2010;34:255-61. [Crossref] [PubMed]
- Engel GM, Lippert FG 3rd. Valgus tibial osteotomy: avoiding the pitfalls. Clin Orthop Relat Res 1981;137-43. [PubMed]
- Bettin D, Karbowski A, Schwering L, et al. Time-dependent clinical and roentgenographical results of Coventry high tibial valgisation osteotomy. Arch Orthop Trauma Surg 1998;117:53-7. [Crossref] [PubMed]
- Akizuki S, Shibakawa A, Takizawa T, et al. The long-term outcome of high tibial osteotomy: a ten- to 20-year follow-up. J Bone Joint Surg Br 2008;90:592-6. [Crossref] [PubMed]
- Tang WC, Henderson IJ. High tibial osteotomy: long term survival analysis and patients' perspective. Knee 2005;12:410-3. [Crossref] [PubMed]
- Flecher X, Parratte S, Aubaniac JM, et al. A 12-28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res 2006;91-6. [Crossref] [PubMed]
- Matthews LS, Goldstein SA, Malvitz TA, et al. Proximal tibial osteotomy. Factors that influence the duration of satisfactory function. Clin Orthop Relat Res 1988;193-200. [PubMed]
- Hankemeier S, Mommsen P, Krettek C, et al. Accuracy of high tibial osteotomy: comparison between open- and closed-wedge technique. Knee Surg Sports Traumatol Arthrosc 2010;18:1328-33. [Crossref] [PubMed]
- Keene JS, Dyreby JR Jr. High tibial osteotomy in the treatment of osteoarthritis of the knee. The role of preoperative arthroscopy. J Bone Joint Surg Am 1983;65:36-42. [Crossref] [PubMed]
- Van den Bempt M, Van Genechten W, Claes T, et al. How accurately does high tibial osteotomy correct the mechanical axis of an arthritic varus knee? A systematic review. Knee. 2016;23:925-935. [Crossref] [PubMed]
- Bae DK, Song SJ, Yoon KH. Closed-wedge high tibial osteotomy using computer-assisted surgery compared to the conventional technique. J Bone Joint Surg Br 2009;91:1164-71. [Crossref] [PubMed]
- Gaasbeek RD, Welsing RT, Verdonschot N, et al. Accuracy and initial stability of open- and closed-wedge high tibial osteotomy: a cadaveric RSA study. Knee Surg Sports Traumatol Arthrosc 2005;13:689-94. [Crossref] [PubMed]
- Magyar G, Toksvig-Larsen S, Lindstrand A. Open wedge tibial osteotomy by callus distraction in gonarthrosis. Operative technique and early results in 36 patients. Acta Orthop Scand 1998;69:147-51. [Crossref] [PubMed]
- Ekhtiari S, Haldane CE, de Sa D, et al. Return to Work and Sport Following High Tibial Osteotomy: A Systematic Review. J Bone Joint Surg Am 2016;98:1568-77. [Crossref] [PubMed]
- Rossi R, Bonasia DE, Amendola A. The role of high tibial osteotomy in the varus knee. J Am Acad Orthop Surg 2011;19:590-9. [Crossref] [PubMed]
- Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop 2010;34:155-60. [Crossref] [PubMed]
- Magyar G, Ahl TL, Vibe P, et al. Open-wedge osteotomy by hemicallotasis or the closed-wedge technique for osteoarthritis of the knee. A randomised study of 50 operations. J Bone Joint Surg Br 1999;81:444-8. [Crossref] [PubMed]
- Song EK, Seon JK, Park SJ, et al. The complications of high tibial osteotomy: closing- versus opening-wedge methods. J Bone Joint Surg Br 2010;92:1245-52. [Crossref] [PubMed]
- Preston S, Howard J, Naudie D, et al. Total knee arthroplasty after high tibial osteotomy: no differences between medial and lateral osteotomy approaches. Clin Orthop Relat Res 2014;472:105-10. [Crossref] [PubMed]
- Bastos Filho R, Magnussen RA, Duthon V, et al. Total knee arthroplasty after high tibial osteotomy: a comparison of opening and closing wedge osteotomy. Int Orthop 2013;37:427-31. [Crossref] [PubMed]
- Petersen W, Metzlaff S. Open wedge high tibial osteotomy (HTO) versus mobile bearing unicondylar medial joint replacement: five years results. Arch Orthop Trauma Surg 2016;136:983-9. [Crossref] [PubMed]
- Nwachukwu BU, McCormick FM, Schairer WW, et al. Unicompartmental knee arthroplasty versus high tibial osteotomy: United States practice patterns for the surgical treatment of unicompartmental arthritis. J Arthroplasty 2014;29:1586-9. [Crossref] [PubMed]
- Börjesson M, Weidenhielm L, Mattsson E, et al. Gait and clinical measurements in patients with knee osteoarthritis after surgery: a prospective 5-year follow-up study. Knee 2005;12:121-7. [Crossref] [PubMed]
- Broughton NS, Newman JH, Baily RA. Unicompartmental replacement and high tibial osteotomy for osteoarthritis of the knee. A comparative study after 5-10 years' follow-up. J Bone Joint Surg Br 1986;68:447-52. [PubMed]
- Ivarsson I, Gillquist J. Rehabilitation after high tibial osteotomy and unicompartmental arthroplasty. A comparative study. Clin Orthop Relat Res 1991;139-44. [PubMed]
- Stukenborg-Colsman C, Wirth CJ, Lazovic D, et al. High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7-10-year follow-up prospective randomised study. Knee 2001;8:187-94. [Crossref] [PubMed]
- Weale AE, Newman JH. Unicompartmental arthroplasty and high tibial osteotomy for osteoarthrosis of the knee. A comparative study with a 12- to 17-year follow-up period. Clin Orthop Relat Res 1994;134-7. [PubMed]
- Mancuso F, Hamilton TW, Kumar V, et al. Clinical outcome after UKA and HTO in ACL deficiency: a systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:112-22. [Crossref] [PubMed]
- Fisher DE. Proximal tibial osteotomy 1970-1995. Iowa Orthop J 1998;18:54-63. [PubMed]
- Papachristou G, Plessas S, Sourlas J, et al. Deterioration of long-term results following high tibial osteotomy in patients under 60 years of age. Int Orthop 2006;30:403-8. [Crossref] [PubMed]
- Kettelkamp DB, Wenger DR, Chao EY, et al. Results of proximal tibial osteotomy. The effects of tibiofemoral angle, stance-phase flexion-extension, and medial-plateau force. J Bone Joint Surg Am 1976;58:952-60. [Crossref] [PubMed]
- Insall JN, Hood RW, Flawn LB, et al. The total condylar knee prosthesis in gonarthrosis. A five to nine-year follow-up of the first one hundred consecutive replacements. J Bone Joint Surg Am 1983;65:619-28. [Crossref] [PubMed]
- Meding JB, Keating EM, Ritter MA, et al. Total knee arthroplasty after high tibial osteotomy. A comparison study in patients who had bilateral total knee replacement. J Bone Joint Surg Am 2000;82:1252-9. [Crossref] [PubMed]
- Katz MM, Hungerford DS, Krackow KA, et al. Results of total knee arthroplasty after failed proximal tibial osteotomy for osteoarthritis. J Bone Joint Surg Am 1987;69:225-33. [Crossref] [PubMed]
- Mont MA, Antonaides S, Krackow KA, et al. Total knee arthroplasty after failed high tibial osteotomy. A comparison with a matched group. Clin Orthop Relat Res 1994;125-30. [PubMed]
- Scuderi GR, Windsor RE, Insall JN. Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am 1989;71:245-8. [Crossref] [PubMed]
- Windsor RE, Insall JN, Vince KG. Technical considerations of total knee arthroplasty after proximal tibial osteotomy. J Bone Joint Surg Am 1988;70:547-55. [Crossref] [PubMed]
- Cerciello S, Vasso M, Maffulli N, et al. Total knee arthroplasty after high tibial osteotomy. Orthopedics 2014;37:191-8. [Crossref] [PubMed]
- Hernigou P, Duffiet P, Julian D, et al. Outcome of total knee arthroplasty after high tibial osteotomy: does malalignment jeopardize the results when using a posterior-stabilized arthroplasty? HSS J 2013;9:134-7. [Crossref] [PubMed]
- Kleinbart FA, Bryk E, Evangelista J, et al. Histologic comparison of posterior cruciate ligaments from arthritic and age-matched knee specimens. J Arthroplasty 1996;11:726-31. [Crossref] [PubMed]
- Gill T, Schemitsch EH, Brick GW, et al. Revision total knee arthroplasty after failed unicompartmental knee arthroplasty or high tibial osteotomy. Clin Orthop Relat Res 1995;10-8. [PubMed]
Cite this article as: Mattei L, Lea S, Nicolaci G, Ferrero G, Marmotti A, Castoldi F. Closing wedge tibial osteotomy: is it an actual procedure nowadays? Ann Joint 2017;2:30.



