
Medial unicompartmental knee arthroplasty
Introduction
Unicompartmental knee arthroplasty (UKA) is a surgical procedure even now discussed, but interest on it increased rapidly over the last three decades. At the end of the eighties, several studies showed failures of the implant up to 30% at 5–7 years follow-up and this leads a progressive abandonment of this procedure (1-4). Main causes of failure and indications for revision were due to mechanical alignment mistakes, implant design (5), bad cementing technique and mobilization or wear of all-polyethylene tibial tray with a thickness inferior to 6 mm (6). In 1994 the Swedish Joint Replacement Registry recorded high failure rate. Nevertheless, this result is attributable to patient’s selection: surgery was primarily performed in patients affected by rheumatoid arthritis (7).
After publication of numerous studies at the end of the years 1990 showing survival of the implant at 10 years superior to 93%, the interest in UKA has increased rapidly again (8). The introduction of a flat tibial component on which a fully congruent polyethylene mobile bearing is seated has subsequently stimulated the interest towards this surgical procedure: the level of congruence of the articular surfaces is increased and polyethylene wear characteristics of the mobile bearing device are improved. Goodfellow and O’Connor reported good to excellent long-term follow-up (9).
Recently, the introduction of minimally invasive surgical (MIS) techniques with modified surgical instruments reduced morbidity, complications and the hospital recovery time. Bone preservation technique, reduced surgical time, fast recovery time and good clinical out-come scores made UKA as valid alternative to high tibial osteotomy (HTO) in relatively young patient. Prospective study showed a high survival rate of UKA with a low major complication rate when strict indication criteria are followed: good results are also due to accurate surgical technique and modern implant design (10,11). Currently UKA represents around the 8% of knee arthroplasty annually performed in the United States (12).
In order to achieving good results, careful selection of the patient is mandatory.
The degenerative process must be predominantly unicompartmental and X-ray skyline of patellofemoral joint has to be acceptable, without lateral facet osteoarthritis with bone loss, grooving or subluxation; at X-ray stress the opposite compartment needs full thickness cartilage without narrowing. It’s recommended to perform UKA only if there is exposed bone on both the femur and tibia in the involved compartment.
Anterior cruciate ligament (ACL) must result functionally intact, while the absence of the ACL with posterior erosion or subluxation at true lateral X-ray is a contraindication (13). Femoral condyle osteonecrosis is acknowledged as good indication for UKA. Pre-operative mal-alignment of mechanical axis should be corrigible; this is usually possible in case of varus inferior to 15° or valgus inferior to 20°. Knee flexion deformity must be inferior to 15°: in fact, correction of more severe flexion deformity is prevent by difficult osteophytes exeresis (14).
Principal contraindications for UKA are: bone-on-bone is not seen on antero-posterior weight bearing view X-ray or varus-valgus stress X-ray or Rosenberg standing posteroanterior 20° flexion X-ray; septic knee arthritis; metal or cement hypersensitivity; patella-femoral osteoarthritis with bone loss, grooving or patella subluxation; bone narrowing of opposite compartment; rheumatic diseases, correlated to progressive bone degeneration, and chondrocalcinosis; severe bone deformity; limited knee range-of-motion with flexion inferior to 90°; sportive young patient <60 years old; body mass index >40.
Between the acute complications, deep venous thrombosis is one of the most frequent complications. The infectious risk results globally inferior in comparison to total hip or total knee arthroplasty (15). It’s demonstrated paralysis of the peroneus common nerve common even if this event is more frequent after total knee arthroplasty for severe valgus knee. Tibial plateau or femoral condyle fractures can be caused by rising stresses during cementing; this eventuality, even though possible, is rare, as the risk of post-operative instability results uncommon (16). The most common reason for revision is aseptic loosening: so, malposition of the components results as one of the principal cause of late complication. Articular disequilibrium causes alteration on loads distribution with cartilage degeneration of healthy compartment or polyethylene wear with consequent implant failure. Dislocation of tibial polyethylene mobile bearing is rare and it’s due usually to a mismatch in the extension and flexion gap. Wrong positioning of the components can cause moreover partial dislocation of tibial tray on the femur, patella impingement and sometimes patella instability (17).
Methods
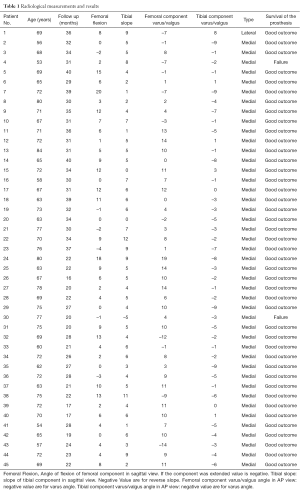
From January 2014 to December 2015 we treated 45 knees in 44 patients (Table 1). A lateral unicompartmental knee arthroplasty (UKA) was performed in 1 case, while the medial unicompartmental knee arthroplasty was performed in 44 cases.
Full table
The diagnosis was primary monocompartimental arthritis of the knee in all cases. We selected patients with osteoarthritis grade 3–4 Kellgren-Lawrence for the tibiofemoral joint. Each patient gave their informed consent before the surgical procedure and was subjected to a clinical exam and radiographic investigations before and after surgery. We used Oxford Partial Knee system as unicompartmental implants. In order to evaluate the stability and the cartilage degeneration we performed a preoperative knee MRI. Radiological analysis included standard anterior-posterior, lateral view of knee and axial view of the patella at 3 and 12 months postoperatively, and yearly thereafter.
On postoperative standard anterior-posterior and lateral views, we evaluated the positioning of the implants, as shown by Sarmah et al. (18). In the antero-posterior view, we measured the valgus/varus angle of the femoral and tibial components: we measured the angle between the diaphyseal axis with the femoral component axis and the perpendicular of the tibial basis. In the lateral view we measured the tibial component slope and the femoral component flexion. Regarding tibial component slope we measured the angle between tibial axis and the component basis, while in order to evaluate the femoral component flexion, we measured the angle between femoral axis and the axis of the femoral component peg. In the last cases the newer femoral component has two peg; in those cases we used the axis of the biggest peg. All those measurements were performed with the help of Trauma Cad software.
Results
No patients were lost during follow up. The mean follow up was 24 months (SD =6.75; range, 12–36, months). The mean femoral component flexion was 5 degrees (SD =5.72; range, –4–20 degrees) and the mean tibial slope was 5 degrees (SD =3.07; range, –5–12 degrees). The mean varus/valgus angle of femoral component was 5 degrees valgus (SD =7.55; range, 19–14 degrees varus), while the mean varus/valgus angle of tibial component was 3 degrees varus (SD =3.46; range, 8–9 degrees varus).
During follow up we observed two complicated cases: in the first cases, 6 months after surgery the patient was suffering diffused knee pain. At standard X-ray we observed the mobilization of polyethylene and the progression of the osteoarthritis in the external compartment. The patient was subjected to a total knee replacement. In the second case, we observed the mobilization of polyethylene at 3 months after surgery. The patient was subjected to the revision of the tibial component and polyethylene. After that, we obtained a good clinical and functional result.
Discussion
The mean femoral component flexion was 5 degrees and the mean tibial slope was 5 degrees. The mean varus/valgus angle of femoral component was 5 degrees valgus, while the mean varus/valgus angle of tibial component was 3 degrees varus.
Hernigou et al. (19) report in their work that “The mean posterior slope of the tibial implant was significantly less in the group of seventy-seven knees without loosening of the implant” and concludes that more than 7 degrees of posterior slope of the tibial implant should be avoided. According to this precept, our mean tibial slope was 5 degrees. In our second failure the slope was –5 degrees and this may have been one of the factors that brought the polyethylene loosening.
Assor et al. studied the rotatory malposition effects of condylar implant (20). They said that the main cause of failure was rotatory malposition of condylar implant and suggested the importance of finding one method to avoid prosthetic malrotations; they also stressed the importance of improving instrumentations and reproducible techniques to re-establish the 3D anatomic orientation of the femoral component, as a key element for longer life of unicompartmental prostheses.
We obtain good clinical and functional results although the follow up is only of 2 years, we did not use some clinical score to report objective data.
There are few works in literature analysing the femoral component flexion. A wrong position of the femoral component would result in a lower range of movement, but further study are needed. The simple method we used to evaluate this feature of prosthetic implant could be useful for better understanding of UKA and its failure.
The lasts cases were performed with a newer surgical technique. Its most important changes focus in improving the femoral position. The femoral shell presents two pegs in order to have better position accuracy and a better endurance. Another news consists in a little instrument called intramedullary link. It connects the intramedullary guide with the femoral drill guide in order to reduce the risk of wrong positioning in all planes. In fact, it allows the mobilisation of the femoral drill guide blocking it in parallel to the intramedullary guide and, therefore with femoral diaphysis.
Conclusions
After 2-year follow up, the results of our monocompartimental arthroplasty are promising. The mean position of the components appears correct if compared with the literature. The method we used to evaluate femoral component flexion of prosthetic implant could be useful for better understanding of UKA and its failure. The newer technique supports the surgeon in order to reduce the risk of wrong positioning. A longer follow up and further studies are needed in order to evaluate the relationship between the femoral component position and its effect on the clinical results.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Luigi Sabatini) for the series “Osteotomies and partial replacement in early osteoarthritis of the knee” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.06.02). The series “Osteotomies and partial replacement in early osteoarthritis of the knee” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was carried out without an ethics approval, because we only analyzed the X-rays controls of the patients without the involvement of the patients. Each patient gave their informed consent before the surgical procedure.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gunston FH. Polycentric knee arthroplasty. Prosthetic simulation of normal knee movement. J Bone Joint Surg Br 1971;53:272-7. [PubMed]
- Marmor L. Unicompartmental knee arthroplasty. Ten- to 13-year follow-up study. Clin Orthop Relat Res 1988;14-20. [PubMed]
- Laskin RS. Unicompartmental tibiofemoral resurfacing arthroplasty. J Bone Joint Surg Am 1978;60:182-5. [Crossref] [PubMed]
- Insall J, Aglietti P. A five to seven-year follow-up of unicondylar arthroplasty. J Bone Joint Surg Am 1980;62:1329-37. [Crossref] [PubMed]
- Skolnick MD, Bryan RS, Peterson LF. Unicompartmental polycentric knee arthroplasty: description and preliminary results. Clin Orthop Relat Res 1975;208-14. [PubMed]
- Ryd L, Boegård T, Egund N, et al. Migration of the tibial component in successful unicompartmental knee arthroplasty. A clinical, radiographic and roentgen stereophotogrammetric study. Acta Orthop Scand 1983;54:408-16. [Crossref] [PubMed]
- Knutson K, Lewold S, Robertsson O, et al. The Swedish knee arthroplasty register. A nation-wide study of 30,003 knees 1976-1992. Acta Orthop Scand 1994;65:375-86. [Crossref] [PubMed]
- Vorlat P, Verdonk R, Schauvlieghe H. The Oxford unicompartmental knee prosthesis: a 5-year follow-up. Knee Surg Sports Traumatol Arthrosc 2000;8:154-8. [Crossref] [PubMed]
- Goodfellow J, O'Connor J. The mechanics of the knee and prosthesis design. J Bone Joint Surg Br 1978;60-B:358-69. [PubMed]
- Borus T, Thornhill T. Unicompartmental knee arthroplasty. J Am Acad Orthop Surg 2008;16:9-18. [Crossref] [PubMed]
- Jamali AA, Scott RD, Rubash HE, et al. Unicompartmental knee arthroplasty: past, present, and future. Am J Orthop (Belle Mead NJ) 2009;38:17-23. [PubMed]
- Riddle DL, Jiranek WA, McGlynn FJ. Yearly incidence of unicompartmental knee arthroplasty in the United States. J Arthroplasty 2008;23:408-12. [Crossref] [PubMed]
- Pandit H. Combined anterior cruciate reconstruction and Oxford unicompartmental knee arthroplasty. J Bone Joint Surg Br 2006;88:887-92. [Crossref] [PubMed]
- Deschamps G, Chol C. Fixed-bearing unicompartmental knee arthroplasty. Patients’ selection and operative technique. Orthop Traumatol Surg Res 2011;97:648-61. [Crossref] [PubMed]
- Ritter MA, Olberding EM, Malinzak RA. Ultraviolet lighting during orthopaedic surgery and the rate of infection. J Bone Joint Surg Am 2007;89:1935-40. [PubMed]
- Vardi G, Strover AE. Early complications of unicompartmental knee replacement: the Droitwich experience. Knee 2004;11:389-94. [Crossref] [PubMed]
- McAuley JP, Engh GA, Ammeen DJ. Revision of failed unicompartmental knee arthroplasty. Clin Orthop Relat Res 2001;279-82. [Crossref] [PubMed]
- Sarmah SS, Patel S, Hossain FS, et al. The radiological assessment of total and unicompartmental knee replacements. J Bone Joint Surg Br 2012;94:1321-9. [Crossref] [PubMed]
- Hernigou P, Deschamps G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am 2004;86-A:506-11. [Crossref] [PubMed]
- Assor M, Aubaniac JM. Influence of rotatory malposition of femoral implant in failure of unicompartimental medial knee prosthesis. Rev Chir Orthop Reparatrice Appar Mot 2006;92:473-84. [Crossref] [PubMed]
Cite this article as: Atzori F, Schirò M, De Feo C, Borromeo N, Russo R. Medial unicompartmental knee arthroplasty. Ann Joint 2017;2:39.


