
Is stem design important in uncemented total hip replacement to decrease subsidence in obese patients?
There has been a world-wide trend towards cementless total hip replacement (THR) over the last 20 years (1). One of the primary reasons for the introduction of the cementless stem was to improve the outcome in younger, more active patients, particularly males. The New Zealand Joint Registry (NZJR) has shown a revision rate of 0.89/100 component years (cy) for cementless THR’s in patients under 55 years compared to 1.73/100 cy for cemented THR and 0.90/100 cy compared to 0.98/100 cy for those between 55–65 years (P<0.001). Over 65 years this is reversed with the cemented THR surviving significantly longer than the cementless variety (2).
Early revision within 90 days is far more common in the cementless THR (0.899%) compared to cemented THR (0.353%) continuing across all age groups but only reaching statistical significance in those over 65 years (P<0.001). When the reason for revision is evaluated the major cause for early revision in cementless implants is either due to fracture (30%) or dislocation (40%). Both of these reasons for revision can be secondary to stem subsidence. Therefore achieving the initial primary stability of a cementless stem is of paramount importance.
Outcomes following primary THR are influenced by surgical, patient and implant-related factors. Body mass index (BMI) is an important patient-related factor that can influence outcomes following cementless THR (3,4). In this article we will discuss the article “Cementless tapered wedge femoral stems decrease subsidence in obese patients compared to traditional fit-and-fill stems” by Grant et al. in the Journal of Arthroplasty (5) and also consider the findings from the NZJR 17 year results of the Corail (Depuy Synthes, Johnson and Johnson) stem which is the commonest cementless stem implanted in our country.
Synopsis of study findings
The study by Grant et al. is a single-surgeon retrospective cohort of 126 consecutive cementless primary THRs. The article compares the short-term radiographic outcomes of two cementless, proximally-tapered porous coated stems produced by Stryker: the Sur-Fit (a traditional “fit-and-fill”, “ream-and-broach” stem) and the Accolade II (a more modern “metaphysical tapered wedge design”). The rationale for this study was that cementless femoral stems that are designed to maximize the fill of the medullary canal and increased cortical contact will reduce stem motion.
All THRs were performed by the posterior approach and patients followed a standardized perioperative care pathway. The null hypothesis was that there would be no difference between the two stems in terms of radiographic femoral canal fill and subsidence with reference to the femoral neck cut. BMI was examined as a covariate.
This study showed that when comparing two similar patient groups those who had the “fit-and-fill” cementless stems had significantly less femoral canal fill compared to the “metaphyseal tapered wedge” cementless stems. The “fit-and-fill” design aims to fill the metaphysis in both coronal and sagittal planes whereas the “metaphyseal tapered wedge” design aims for a more congruent cortical fit in the coronal plane. Interestingly the rate of stem subsidence of >2 mm was more than 10 times more prevalent in the “fit-and-fill” group. The subsidence did not increase from 4 weeks to 1 year and the rate of subsidence in the “fit-and-fill” correlated directly with the patient’s BMI, which was not the case in the “metaphyseal tapered wedge” group. In this series there were no revisions for instability or aseptic loosening. However, a number of cases had periprosthetic fractures and these were excluded from the analysis. The infection rate of four cases in 126 THR is notably high.
Critical appraisal
Whilst the authors should be commended on demonstrating the correlation between BMI and subsidence in conjunction with these stem designs, further studies are required to substantiate these findings. In a previous study early stem subsidence was associated with aseptic loosening in the long term (6). The short-term follow-up and retrospective nature of this cohort study are therefore limitations.
The method of radiological assessment also warrants examination. Firstly the estimation of femoral canal fill and component extension is difficult without accounting for limb rotation. There was no description in the article about considering this or how it was achieved. Secondly the method for evaluating stem migration is not validated and could be potentially improved by using RSA (7,8) or alternatively EBRA (9).
This study can also be criticized on the basis of lack of patient reported outcome measures, in particular the physical activity of the patient, and short length of follow-up. A registry-based study to examine the differences in revision rates and reasons for revision would add an interesting perspective when considering this paper.
Another important consideration is that not all cementless stems achieve canal fill to gain stability. The Corail stem (Depuy Synthes, Johnson and Johnson) is a common cementless prosthesis which achieves rotational stability without canal or metaphyseal fill. It is a fully hydroxyapatite coated prosthesis which is designed to preserve the metaphyseal bone by compaction broaching as part of the design rationale. Canal fill is avoided to limit “hold-up” of the stem by premature distal on-growth. If the results of this study are extrapolated then one would expect Corail to behave more like the Sur-Fit and subside with greater BMI potentially undergoing more revisions especially for instability, fracture and aseptic femoral loosening. To put this study into context we have therefore examined the NZJR results of the Corail stem in primary THR accounting for BMI, gender and age.
NZJR perspective
The NZJR was established in 1998 and has a >96% data capture rate of all joint replacement surgeries. Prospective entry of data into the NZJR is a mandatory requirement of all members of the New Zealand Orthopaedic Association with all data secured in Christchurch, New Zealand. One of the authors (Chris Frampton) accessed the database to acquire the data specifically for this study. We performed a retrospective cohort analysis of the 17-year results of the NZJR identifying all primary THR’s performed between 1st January 1999 and 31st December 2016 using the Corail cementless stem. Bilateral cases were considered separately. Data-linkage to the national New Zealand register for marriages, births and deaths is performed automatically to the NZJR every 6 months.
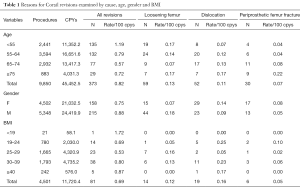
There were 9,850 Corail stems identified in the NZJR and the overall all-cause revision rate was 0.82/100 cy (373 revisions for any cause). The highest rate of all-cause revision for this stem was greatest in those <55 years or age and lowest in those >75 years or age (1.19/100 and 0.57/100 cy, respectively). Interestingly the highest rates of revision for aseptic femoral loosening was seen in these same age groups [0.17/100 cy (14.1%) for <55 years of age; 0.17/100 cy (24.1%) for >75 years of age] (Table 1).
Full table
When examining gender as a covariate the all cause revision rates were less in females (0.75/100 cy) vs. males (0.88/100 cy). Revision for aseptic femoral loosening was also more common in males (0.18/100 cy; 20.5%) compared to females (0.07/100 cy; 9.5%). Revisions for instability were greater in females than males [0.14/100 cy (18.4%) females; 0.09/100 cy (10.7%) males]. There was an even gender distribution for all other causes of revision including periprosthetic femoral fractures.
Extremes of BMI ≥40 and <19 kg/m2 were associated with the highest rates of all-cause revision (0.87/100 cy and 1.72/100 cy, respectively). Interestingly a BMI of 25–29 had the highest associated revision rate for femoral loosening (0.16/100 cy; 30.4%). BMI did not correlate with the rate of revision for periprosthetic femoral fracture or dislocation.
Conclusions
The study by Grant et al. has highlighted the different ways in which cementless femoral stems achieve primary stability and raises the issue of fit-and-fill stems having a greater rate of early subsidence with increasing BMI. However given the results of the NZJR for the Corail cementless stem which neither fills the metaphysis nor the diaphysis we question these findings; the Corail did not have a higher rate of revision for aseptic femoral loosening with increasing BMI. Other factors such as surgical training and technique may be of crucial importance.
BMI has been used in this current study, and many others, as a surrogate for increased force or weight transferred across the joint, however we know that several other factors are involved in increased load transmission across a hip replacement. Perhaps a better way of determining the force across the joint would be by using weight alone, and stratify subsidence into various “weight bands”. Male gender has been associated with increased risk of loosening, presumably secondary to the increased weight of males and their perceived higher physical activity, which is likely to load the joint more than females. Our review of the Corail stem would support this accusation with increased aseptic loosening of both the femur and acetabulum in young males. In future we believe that any discussion on loosening and subsidence of the cementless femoral stem should be accompanied with data on the patient’s weight and overall physical activity. Certainly risk stratification of patients will become increasingly relevant with more drive towards value-based healthcare and minimizing complications.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Executive Editor-in-Chief, Dongquan Shi, MD, PhD (Department of Sports Medicine and Adult Reconstruction, Drum Tower Hospital, Medical School, Nanjing University, Nanjing, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.07.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hooper GJ, Rothwell AG, Stringer M, et al. Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br 2009;91:451-8. [Crossref] [PubMed]
- Wyatt M, Hooper G, Frampton C, et al. Survival outcomes of cemented compared to uncemented stems in primary total hip replacement. World J Orthop 2014;5:591-6. [Crossref] [PubMed]
- Stihsen C, Radl R, Keshmiri A, et al. Subsidence of a cementless femoral component influenced by body weight and body mass index. Int Orthop 2012;36:941-7. [Crossref] [PubMed]
- Jacobs CA, Christensen CP. Progressive subsidence of a tapered, proximally coated femoral stem in total hip arthroplasty. Int Orthop 2009;33:917-22. [Crossref] [PubMed]
- Grant TW, Lovro LR, Licini DJ, et al. Cementless Tapered Wedge Femoral Stems Decrease Subsidence in Obese Patients Compared to Traditional Fit-and-Fill Stems. J Arthroplasty 2017;32:891-7. [Crossref] [PubMed]
- Streit MR, Haeussler D, Bruckner T, et al. Early Migration Predicts Aseptic Loosening of Cementless Femoral Stems: A Long-term Study. Clin Orthop Relat Res 2016;474:1697-706. [Crossref] [PubMed]
- Collopy D. A prospective single-centre case series using Roentgen Stereophotogrammetruc analysis (RSA) to evaluate stem micromotion of the Stryker Accolade II cementless hip system two years post-surgery. Bone Joint J 2017;99-B:77.
- Selvik G. Roentgen stereophotogrammetry. Acta Orthop Scand 2009;60:1-51. [Crossref] [PubMed]
- Wilkinson JM, Hamer AJ, Elson RA, et al. Precision of EBRA-Digital software for monitoring implant migration after total hip arthroplasty. J Arthroplasty 2002;17:910-6. [Crossref] [PubMed]
Cite this article as: Wyatt M, Frampton C, Hooper G. Is stem design important in uncemented total hip replacement to decrease subsidence in obese patients? Ann Joint 2017;2:50.


