
Is high hip center technique an acceptable choice for total hip arthroplasty of the developmental dysplasia of the hip?
Developmental dysplasia of the hip (DDH) is a common cause of hip pain, deformity and limb-length discrepancy (LLD) (1), which is characterized by shallow and short acetabulum and normal or flattened femoral head, with anatomic deformities ranging from a shallow acetabulum, subluxation hip to the femoral head fully dislocation from the acetabulum (2). In low subluxation hip, the acetabulum is small and shallow. The deficiency of bone is usually in the anterior, superior and lateral of the acetabulum, with posterior bone stock much better. The normal or nearly normal femoral head makes contact with only a part of the acetabulum, with a normal displacement position. In high dislocation hip, the pelvis is small with thin and soft acetabular walls, and the femoral head is out of the acetabulum (3). Crowe classification is most popular used methods to evaluate the hip dysplasia, which compared the proximal migration extent of femoral head to the height of the normal femoral head or pelvis as follows. Crowe I: proximal displacement less than 50% of the normal femoral head or 10% of pelvis; Crowe II: proximal displacement from 50% to 75% of the normal femoral head; Crowe III: proximal displacement from 75% to 100% of the normal femoral head; Crowe IV: proximal displacement more than 100% of femoral head or 20% of pelvis (4).
Total hip arthroplasty (THA) is one of most popular used methods to treat these patients with symptomatic osteoarthritis secondary to DDH (5). The main goal of replacement of hip is to reconstruct a durable functional hip joint similar to normal. It is predicted to reconstruct the acetabular prosthesis at the ideal anatomic acetabular location with normal offset and rotation center, to acquire well balance of the muscles around the hip joint, to restore the abductor mechanism, respectively. However, the complexity of THA is increased as the anatomic abnormalities in DDH. Hereby, several techniques are introduced, such as bone grafting or bulk femoral autografting allowing sufficient bony coverage of the acetabular component, or placing the socket medial or proximal of the shallow acetabulum (6).
The high hip center (HHC), which allows implanting the socket proximally to the normal rotation center of the hip, is one of the frequently used methods. However, it is still controversial whether this method is acceptable for most DDH cases and how to define the proper height of hip center.
Several reconstructive techniques to restore sufficient coverage of acetabulum implant in anatomic hip rotation center
Many techniques were used to reconstruct hip rotation center in the anatomic location, such as medial protrusio-technique, bone grafting and special sockets. These methods were popular but with controversial results among different reports, especially some results showed that poor long-term survival rates of the prosthesis.
The medial protrusio-technique was asked to ream the medial wall of the pelvis, which allowed acetabular component max containment but may reduce joint reaction forces. This technique is acceptable even few data confirming its safety (7). Another option is using bone cement alone without additional support to reconstruction of the bone defect, which is easy to fail because of the high loosening rates of acetabular prosthesis (8).
Bone grafting and bulk femoral autografting to acetabular reconstruction have been described widespread and at the time represents probably the gold standard (9-12). But the rehabilitation process of patients can be prolonged because of the partial weight-bearing required. This method has been nearly abandoned because of the increased operative time, high rate of graft resorption and expanded soft tissue exposure (13).
To overcome these disadvantages, special designed sockets were also used in this situation. The cranial socket, with the antero-posterior dimension lesser than the craniocaudal dimension, is designed to reconstruction of acetabular deficiency, which can be used in the osteoarthritis of the hip secondary to DDH. The femoral head can be placed eccentrically and allows more distally locate of the center of rotation. Accordingly, in the small external diameter of most DDH cases, greater superior polyethylene thickness can be used, which may be benefit to extend the wear time. Holzapfel BM et al. reported good mid-term results using these cranial sockets (14). Another socket was designed with 15° face-changing to maximizing the cover of the component by host bone while position the optimal angle of inclination, which similarly had good short follow-up time results (15).
How to determinate the center of rotation of the hip?
The center of rotation of the hip is one key landmarks of THA, which position determines both vertical limb-length and the horizontal lever arms of abductor muscles. Determine the position of hip rotation is one of the key steps for pre-operation planning, which is also important during operation and post-operation evaluation. As the contralateral hip can be used as a reference, it is easy to determine the rotation center with a healthy control hip joint but which becomes difficult while the contralateral hip is destroyed, too (16).
Many anatomic locations and reference lines showed on the anteroposterior (AP) radiological view of pelvis were introduced, each with not only advantages but also disadvantages, which should be selected properly when used in different conditions depending on the anatomic deformities and surgeries (Figure 1).
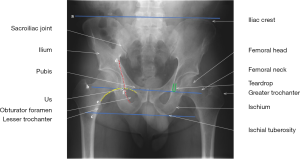
Lewalle J et al. introduced one method refer to the highest point of the obturator foramen, 25 mm above this point was considered the theoretic center of the hip. This method defines the vertical position only but not the mediolateral position of the rotation center of the hip (17). Boudriot U et al. introduced another method to determine the rotation center of the hip, both the vertical and mediolateral distances in relation to the point of intersection between two reference lines were used, a horizontal line between the superior rims of the two obturator foramen and Kohler’s line, which is defined as a line showed on AP view of pelvis, connecting most lateral aspect of pelvic brim and most lateral aspect of obturator foramen (18). Ranawat CS et al. described a method on the frontal radiograph of the pelvis two horizontal lines were traced, with one horizontal line between the summit of the iliac crests, and the other line between the lowest point of the two ischial tuberosities. It is practicable to a normal ilium but not applicable with the subluxation hip, because of the abnormal of the Shenton’s line, which is defined as a curved line formed by the top of the obturator foramen and the inner side of the femoral neck (19).
The horizontal line between the most distal points of the two sides radiological teardrop was defined as line TD. Fessy MH et al. defined the intersection between Kohler’s line and the TD line as radiological Us, which determine the horizontal and vertical rotation center of the femoral head. This procedure is useful even the acetabulum is destroyed bilaterally for preoperative planning of prosthetic reconstruction (16). Crowe JF et al. induced Us line as the location level of the head-neck junction of a normal hip. This method is only used before operation. When a prosthesis is in place or a resection of the femoral neck is done it becomes useless (4).
It is difficult to confirm the center of rotation during operation. Lu YF et al. reported the teardrop as a reference (20). It is assumed that the placement of the lower aspect of the acetabular component is at the same horizontal plane of the lower aspect of the teardrop. The lower edge of the teardrop can be used as a guide for judgement of the correct placement of the acetabular prosthesis in operation. If the lower aspect of the acetabular component is above lower edge of the teardrop, it is referred to superior placement and vice versa.
HHC leads to the lever arms and gait changes after THA
HHC can lead changes of length of the gluteus minimus muscle, the gluteus maximus muscle and also other abductor muscles. Jerosch J et al. reports that increased length of the gluteus maximus muscle and the posterior part of the gluteus minimus muscle and decreased length of these evaluated abductor muscles were seen in the HHC cases. As these muscles were important for the pelvic stabilization, the necessary muscle strength need is increased largely because of the lever arms changes and may resulting in insufficiency of the abductor muscles (21). Kiyama T et al. also found that compared with the abductor muscle strength of the inferior group, that of the HHC group was decreased significantly (22). If placing the cup in the true acetabulum of a Crowe III or IV dysplastic hip, the rotation center of the hip will move medially, inferiorly and also anteriorly from the normal hip center, which will lead to joint reaction force, abductor muscle force and contraction force decrease and the abductor muscle preload increase slightly (23). On the basis of these findings, it is not recommended to implant the acetabular component at a HHC location. When superior placement of the hip center in THA, it is suggested to avoid lateralize of the rotation center of the hip, which could decrease postoperative abductor muscle strength.
HHC influences hip load after THA
Goran Bicanic et al. concerned about whether acetabular cup position can influence the hip load during THA in DDH. They found that displacement of the acetabular cup every millimeter of laterally or proximally relative to the ideal center of rotation, it was expected an increase of 0.7% or 0.1% respectively in hip load. The hip load was expected 1% decrease for every millimeter of neck length increase, and was expected 0.8% decrease for every millimeter of lateral offset. According to their model, if the acetabular cup is placed within five millimeters of the ideal anatomic center of rotation, the hip load changes is within 10% relative to that in the ideal center of rotation (24). Altogether, the hip load will increase if the cup is placed laterally or in HHC while the hip load will decrease if a longer femoral neck or lateral offset is used.
Range of hip joint motion in HHC patients after THA
The required range of motion (ROM) for hip joint is defined as flexion ≥110°, extension ≥30°, and external rotation ≥30°, internal rotation (IR) at 90° flexion ≥30°. Whether a HHC influences the postoperative ROM in THA or not? Komiyama K et al. reported that the higher hip center decreased the range of hip flexion and IR, but increased the range of extension and external rotation. In terms of ROM, acceptable vertical center of rotation in DDH was around 35 mm (25). It is also predicted that the impingement may occurs because of the increased external rotation of hip joint.
The loosening rate and polyethylene wear of the HHC after THA
Loosening rates and polyethylene wear varied in different studies. It was shown that the early results of loosening rates of acetabular prosthesis ranging from 16% to 42%, while the cup was placed higher than the anatomy hip center with cemented fixation. Callaghan JJ et al. reported that HHC placement account for 41% loosening of the acetabular component, and they assumed that inadequate anatomic reconstruction leading to mechanical failure and progressive radiolucencies (26). Pagnano W et al. reported similar results. They found that the sockets placed more than fifteen millimeters higher to the theoretic center of femoral head related with an increased rate of acetabular components loosening, therefore revision of these components needed (27). Previous experimental studies suggest that it was an unacceptable with the socket placement higher (28). These findings suggest that HHC leads to increased rates of loosening of the acetabular components and polyethylene wear. According to these results, HHC should be avoid and the placement of acetabular component should be in or near the true acetabular region (27).
However, Murayama T et al. reported there is no significantly difference of the average rates of polyethylene wear and survivorship of prosthesis, a 15 years of clinical and radiographic outcomes for Crowe I–III with anatomic cup placement (29). There was no difference between the HHC group and the anatomic hip center group of the Kaplan-Meier survivorship, whatever the revision reasons. Wear rates and acetabular loosening did not differ significantly between these two groups. At 10-year follow-up, the acetabular polyethylene wear was more in lateralized acetabular reconstructions groups than that of medialized groups with a HHC position. Medialization of hip center was important to decrease wear during THA in DDH (30). Schutzer SF and Harris WH showed that HHC group also had an satisfactory survivorship and there was no cup failures account for acetabular loosening (31). Christodoulou NA et al. showed that the wear of PE or mechanical loosening were similar between these two groups, superolateral placement of the cup and placement on the true acetabulum, with a mean 8.6±3.5 years follow-up (32).
These controversial results focus on the loosening rate and polyethylene wear gave issue problem about whether HHC technology reliable or not during THA. Interestingly, earlier reports showed higher loosening rate and polyethylene wear, such as Callaghan JJ et al. published their results in 1985 (26) and Pagnano W et al. published their results in 1996 (27), while recently reports showed similar results between HHC group and anatomic hip center, such as Kaneuji A et al. published their data in 2009 (33), Christodoulou NA et al. published their results in 2010 (32), Nawabi DH et al. published their results in 2014 (30), etc. The possible reasons for these differences were improvements of prosthesis designs, surgery concept and techniques. The friction interface defects which were common in the earlier years’ practice definitely led a higher failure rate. As showed by Nawabi DH et al., medialization of hip center was another key factor, which was not concerned in these early reports.
How to define the HHC after THA?
Two studies concerning about HHC follow-up gave good survivorship, low polyethylene wear, low incidence of dislocation and no obviously acetabular loosening, the involved mainly Crowe I and Crowe II dysplasia of the hip patients. In these studies, the mean vertical distance of the hip center were 24.5 and 26.8 mm respectively (29,33). In another study, the mean vertical distance was 25.6 mm in Crowe II cases and was 30.3 mm in Crowe III cases, respectively, referred to the inter teardrop line. Russotti GM (34) and Schutzer SF (31) reported higher failures for acetabular loosening. Reconstruction of the hip 35 mm higher than the inter teardrop line or 15 mm higher than the femoral head center was considered as HHC technique, which was usually helpful to treat the deficient acetabulum.
LLD in the HHC patients after THA
In the HHC patients, it is difficult to equalize limb-length to the opposite cite, which easily result LLD, which can be conceptually divided into structural and functional, a main cause of patient dissatisfaction after THA. Structural LLD may be due to DDH. The deformity of hip can influence the knee joint, with the ipsilateral knee valgus tendency and the contralateral knee tends to be varus. It is thought that after the LLD improved after THA, the lower limb alignment discrepancy was decreased, the clinical outcome was also influenced by LLD which determined by the mechanical axis. Fujimaki H et al. showed that the alignment of the knee tended to be valgus in the same side of the affected hip, while the lower limb alignment discrepancy still existing after THA, which influenced the mechanical axis determined LLD (35). This demonstrated that it is also important to align coronal plane lower limb correctly to get a satisfactory outcome after THA. So it is important to correct the whole-leg LLD rather than the pelvic LLD, no matter reconstructing cup at a higher hip center or in the anatomic center, especially in patients with severe knee deformities, varus or valgus alignment, preoperative (35).
In conclusion, HHC technique is another choice for acetabular reconstruction, which is acceptable while center of rotation located at a distance less than 35 mm from the inter teardrop line and medialization of these HHC reconstructions is suggested. This method can increase host bone coverage of socket without structural bone grafts, simplify surgical procedures, reduce anesthetic and surgical time, conserve of adequate healthy bone stock for revision, elsewise, it leads to insufficiency of the abductor muscles, increased hip load, lower range of hip flexion and IR.
Acknowledgments
Funding: The work was supported by grants from the National Natural Science Foundation of China (grant no. 81201373, 81772410, 81271948) and Postdoctoral Foundation of Shaanxi Province (grant no. 2016BSHEDZZ93).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.09.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Swarup I, Marshall AC, Lee YY, et al. Implant survival and patient-reported outcomes after total hip arthroplasty in young patients with developmental dysplasia of the hip. Hip Int 2016;26:367-73. [Crossref] [PubMed]
- Mavcic B, Iglic A, Kralj-Iglic V, et al. Cumulative hip contact stress predicts osteoarthritis in DDH. Clin Orthop Relat Res 2008;466:884-91. [Crossref] [PubMed]
- Storer SK, Skaggs DL. Developmental dysplasia of the hip. Am Fam Physician 2006;74:1310-6. [PubMed]
- Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am 1979;61:15-23. [Crossref] [PubMed]
- Öner A, Koksal A, Tunç OD, et al. Midterm Results Of Total Hip Arthroplasty (THA) In Developmental Dysplasia Of The Hip (DDH). Internet Journal of Orthopedic Surgery 2015;23.
- Sanchez-Sotelo J, Berry DJ, Trousdale RT, et al. Surgical treatment of developmental dysplasia of the hip in adults: II. Arthroplasty options. J Am Acad Orthop Surg 2002;10:334-44. [Crossref] [PubMed]
- Dorr LD, Tawakkol S, Moorthy M, et al. Medial protrusio technique for placement of a porous-coated, hemispherical acetabular component without cement in a total hip arthroplasty in patients who have acetabular dysplasia. J Bone Joint Surg Am 1999;81:83-92. [Crossref] [PubMed]
- MacKenzie JR, Kelley SS, Johnston RC. Total hip replacement for coxarthrosis secondary to congenital dysplasia and dislocation of the hip. Long-term results. J Bone Joint Surg Am 1996;78:55-61. [Crossref] [PubMed]
- Akiyama H, Kawanabe K, Iida H, et al. Long-term results of cemented total hip arthroplasty in developmental dysplasia with acetabular bulk bone grafts after improving operative techniques. J Arthroplasty 2010;25:716-20. [Crossref] [PubMed]
- Shetty AA, Sharma P, Singh S, et al. Bulk femoral-head autografting in uncemented total hip arthroplasty for acetabular dysplasia: results at 8 to 11 years follow-up. J Arthroplasty 2004;19:706-13. [Crossref] [PubMed]
- Dai X, Omori H, Okumura Y, et al. Bone grafting in cementless total hip replacement for congenital dysplasia of the hip. Int Orthop 2000;24:260-3. [Crossref] [PubMed]
- Papachristou G, Hatzigrigoris P, Panousis K, et al. Total hip arthroplasty for developmental hip dysplasia. Int Orthop 2006;30:21-5. [Crossref] [PubMed]
- Sporer SM, O’Rourke M, Chong P, et al. The use of structural distal femoral allografts for acetabular reconstruction. Average ten-year follow-up. J Bone Joint Surg Am 2005;87:760-5. [PubMed]
- Holzapfel BM, Greimel F, Prodinger PM, et al. Total hip replacement in developmental dysplasia using an oval-shaped cementless press-fit cup. Int Orthop 2012;36:1355-61. [Crossref] [PubMed]
- Zahos K, Mehendale S, Ward AJ, et al. The 15° face-changing acetabular component for treatment of osteoarthritis secondary to developmental dysplasia of the hip. J Bone Joint Surg Br 2012;94:163-6. [Crossref] [PubMed]
- Fessy MH, N'Diaye A, Carret JP, et al. Locating the center of rotation of the hip. Surg Radiol Anat 1999;21:247-50. [Crossref] [PubMed]
- Lewalle J, Hebrant A. Acta Orthop Belg 1990;56:395-405. [Multicenter Belgian study of the results of total arthroplasty for persistent congenital hip dislocation]. [PubMed]
- Boudriot U, Hilgert J, Hinrichs F. Determination of the rotational center of the hip. Arch Orthop Trauma Surg 2006;126:417-20. [Crossref] [PubMed]
- Ranawat CS, Dorr LD, Inglis AE. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg Am 1980;62:1059-65. [Crossref] [PubMed]
- Lu Y, Cheng L, Guo W, et al. Ability of lower teardrop edge to restore anatomical hip center height in total hip arthroplasty. Chin Med J (Engl) 2014;127:3915-20. [PubMed]
- Jerosch J, Steinbeck J, Stechmann J, et al. Influence of a high hip center on abductor muscle function. Arch Orthop Trauma Surg 1997;116:385-9. [Crossref] [PubMed]
- Kiyama T, Naito M, Shitama H, et al. Effect of superior placement of the hip center on abductor muscle strength in total hip arthroplasty. J Arthroplasty 2009;24:240-5. [Crossref] [PubMed]
- Abolghasemian M, Samiezadeh S, Jafari D, et al. Displacement of the hip center of rotation after arthroplasty of Crowe III and IV dysplasia: a radiological and biomechanical study. J Arthroplasty 2013;28:1031-5. [Crossref] [PubMed]
- Bicanic G, Delimar D, Delimar M, et al. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop 2009;33:397-402. [Crossref] [PubMed]
- Komiyama K, Nakashima Y, Hirata M, et al. Does High Hip Center Decrease Range of Motion in Total Hip Arthroplasty? A Computer Simulation Study. J Arthroplasty 2016;31:2342-7. [Crossref] [PubMed]
- Callaghan JJ, Salvati EA, Pellicci PM, et al. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. J Bone Joint Surg Am 1985;67:1074-85. [Crossref] [PubMed]
- Pagnano W, Hanssen AD, Lewallen DG, et al. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am 1996;78:1004-14. [Crossref] [PubMed]
- Doehring TC, Rubash HE, Dore DE. Micromotion measurements with hip center and modular neck length alterations. Clin Orthop Relat Res 1999;230-9. [PubMed]
- Murayama T, Ohnishi H, Okabe S, et al. 15-year comparison of cementless total hip arthroplasty with anatomical or high cup placement for Crowe I to III hip dysplasia. Orthopedics 2012;35:e313-8. [PubMed]
- Nawabi DH, Meftah M, Nam D, et al. Durable fixation achieved with medialized, high hip center cementless THAs for Crowe II and III dysplasia. Clin Orthop Relat Res 2014;472:630-6. [Crossref] [PubMed]
- Schutzer SF, Harris WH. High placement of porous-coated acetabular components in complex total hip arthroplasty. J Arthroplasty 1994;9:359-67. [Crossref] [PubMed]
- Christodoulou NA, Dialetis KP, Christodoulou AN. High hip center technique using a biconical threaded Zweymüller cup in osteoarthritis secondary to congenital hip disease. Clin Orthop Relat Res 2010;468:1912-9. [Crossref] [PubMed]
- Kaneuji A, Sugimori T, Ichiseki T, et al. Minimum ten-year results of a porous acetabular component for Crowe I to III hip dysplasia using an elevated hip center. J Arthroplasty 2009;24:187-94. [Crossref] [PubMed]
- Russotti GM, Harris WH. Proximal placement of the acetabular component in total hip arthroplasty. A long-term follow-up study. J Bone Joint Surg Am 1991;73:587-92. [Crossref] [PubMed]
- Fujimaki H, Inaba Y, Kobayashi N, et al. Leg length discrepancy and lower limb alignment after total hip arthroplasty in unilateral hip osteoarthritis patients. J Orthop Sci 2013;18:969-76. [Crossref] [PubMed]
Cite this article as: Hou W, Lu Y, Xu P. Is high hip center technique an acceptable choice for total hip arthroplasty of the developmental dysplasia of the hip? Ann Joint 2017;2:55.


