
Popliteal artery thrombosis a TKA complication due to retractor: a report of two cases treated with endovascular reconstruction
Introduction
Popliteal artery injury resulting in thrombosis is an uncommon complication after total knee arthroplasty (TKA) (1), with reported incidences ranging from 0.03% to 0.5% (2-5). Early identification and revascularization minimizes the risk of limb loss, although a delayed diagnosis is not uncommon, even in high-volume centers, and is associated with severe consequences. Therefore, we report two cases of popliteal artery thrombosis, which were caused by a retractor during TKA. These cases were successfully treated using emergency endovascular thrombectomy and stent reconstruction. Both patients consented to their data being used for publication.
Case presentation
Case 1
A 76-year-old woman was admitted to undergo unilateral TKA. She did not have a history of peripheral vascular disease, and pulses were palpable in both lower limbs. Right TKA was successfully performed using a posterior stabilized Genesis II implant (Smith & Nephew, Memphis, TN, USA). The tourniquet time was 84 min, the pressure was 260 mmHg, and the surgery was considered uneventful. However, in the recovery room, the affected calf was cool and there was no detectable foot pulse. Doppler examination confirmed that a pulse was present above the knee but not below the knee. Angiography revealed popliteal artery thrombosis at the level of the knee (Figure 1A).
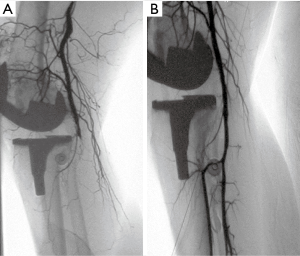
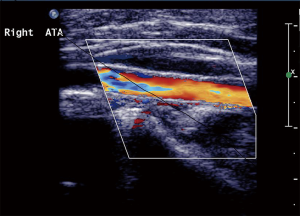
An expandable Astron peripheral stent (Biotronik SE & Co. KG, Woermannkehre, Berlin, Germany) was deployed through a 6-F arterial sheath (Figure 1B), which rapidly restored the distal pulse and leg temperature. The limb had been without perfusion for 380 min. The patient experienced an uneventful in-hospital recovery, and follow-up at 40 months confirmed that her vascular function was intact and the popliteal artery was free from stenosis (Figure 2). The patient reported being satisfied with the result of her surgery.
Although we could not identify the precise cause of the complications in Case 1, we attributed them to the posterior procedures, which were subsequently performed with greater care to avoid arterial injury. During subsequent surgeries, we routinely checked the postoperative status of the dorsalis pedis and posterior tibial arteries. After treating >12 cases without similar complications, we assumed that the issue had been effectively addressed.
Case 2
At 4 months after Case 1, a 71-year-old man was admitted for unilateral TKA. He did not have a history of peripheral vascular disease, and pulses were palpable in both lower limbs. TKA was successfully performed using a posterior stabilized Genesis II implant (Smith & Nephew). The tourniquet time was 80 min, the pressure was 260 mmHg, and the surgery was considered uneventful. However, while still in the operating room, the patient’s distal pulse was not detectable. Doppler examination and angiography (Figure 3A) revealed complete occlusion of the popliteal artery at the level of the knee.
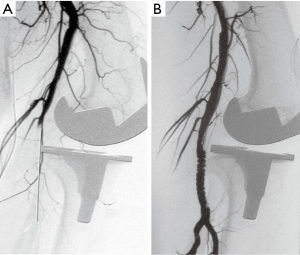
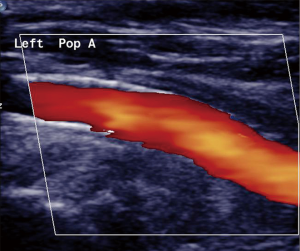
An expandable Astron peripheral stent (Biotronik SE & Co. KG) was deployed through a 7-F arterial sheath (Figure 3B), which rapidly restored the distal pulse. The limb had been without perfusion for 290 min. The patient experienced an uneventful recovery, and follow-ups at 3 and 7 years confirmed that his distal pulse was normal and that there was no stenosis in the popliteal artery (Figure 4). The patient reported being satisfied with the results of the surgery.
Discussion
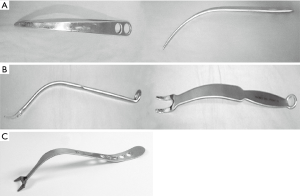
After Case 2, we launched a detailed investigation to determine the cause of these complications. This investigation revealed that we had recently started using retractors that could expose the proximal tibia, with the single-pronged retractor (Figure 5A) replacing the Mikhail double-pronged retractor (Figure 5B). The single toothed retractor was not curved, and had a longer and narrower distal part, which increased the possibility of distal slipping along the posterior tibia. As the single prong applies great pressure to the midline artery, and the proximal tibia is translated anteriorly, deviation from a retractor angle of 90º could apply pressure to the vascular structures by creating an edge that the vessel must stretch to accommodate. Furthermore, careless insertion of this retractor behind the plateau could increase the risk of vascular injury, especially if the insertion site is slightly lateral to the midline. Based on these findings, we resumed using the Mikhail retractor and have successfully performed 270 TKA surgeries without vascular events during the last 3 years. We are aware that another retractor has been specifically designed to avoid this complication, although we have no experience with it (Figure 5C).
Popliteal artery complications are uncommon and classified as direct or indirect. The popliteal artery thrombosis in these cases is an indirect injury, and is the most common popliteal artery complication (6). In this context, thrombosis caused by arterial intimal disruption as the result of extensive surgical manipulation, and some authors have indicated that patients with preexisting vascular disease have an increased risk of vascular injury during TKA (3,7). However, other authors have not confirmed that relationship (2,8). Our cases suggest that surgical instruments can cause indirect popliteal artery injuries, and Ninomiya et al. (9) have also reported that a posterior retractor could cause popliteal artery injury if it was inserted >1 cm into the soft tissues. We believe that this mechanism explains the complications in our cases.
The prognosis for arterial thrombosis injury is mainly determined by the time spent without perfusion, and early identification can facilitate revascularization and minimize the risk of limb loss. However, delayed diagnosis is not uncommon, even in some high-volume joint replacement centers (5). Therefore, we strongly suggest performing vascular evaluation while the patient is in the operating theater. If a pulse is absent and cannot be confirmed during a Doppler examination, an emergent vascular consultation should be called and angiography should be performed.
Popliteal arterial thrombosis secondary to arterial injury can be treated using autologous venous bypass grafting (5,10). However, this technique is complicated in cases with recent TKA. Moreover, endovascular treatment is safe, durable, and effective, with patency rates that are comparable to those of bypass grafting (11). Thus, endovascular treatment may be especially effective after TKA, as it is minimally invasive and can be effectively performed near the operative site (12). Semi-rigid stents placed across the joint may be prone to breakage, although Piffaretti et al. (13) failed to identify early mechanical adverse events when stents were used in this manner. Moreover, late failure after endovascular treatment could be re-treated or addressed using elective bypass grafting after the acute phase of the earlier knee surgery. This would limit the additional trauma and risk that is associated with open surgery soon after TKA.
Fortunately, acute arterial thrombosis not commonly associated with TKA. Nevertheless, a thorough understanding of the normal and anatomical variants is essential, as well as careful intraoperative instrumentation and knee manipulation. Thus, careful attention to the specific surgical techniques can decrease the incidence of direct and indirect intraoperative arterial injuries.
Conclusions
Our two cases demonstrate that immediate endovascular repair of popliteal artery thrombosis is possible and durable. Furthermore, these iatrogenic injuries appear to have been induced by the use of a specific type of retractor. Prompt recognition and treatment are critical to resolving arterial thrombosis, preserving the affected limb, and limiting patient morbidity. Therefore, our experience indicates that endovascular treatment can be considered in cases of popliteal arterial thrombosis after TKA.
Acknowledgments
The authors appreciate the patients’ consent to present this case.
Funding: This work was supported by Beijing outstanding talent project (No. 2015000020124G116).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.10.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor(s)-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lazaro LE, Cross MB, Lorich DG. Vascular anatomy of the patella: implications for total knee arthroplasty surgical approaches. Knee 2014;21:655-60. [Crossref] [PubMed]
- Rand JA. Vascular complications of total knee arthroplasty. Report of three cases. J Arthroplasty 1987;2:89-93. [Crossref] [PubMed]
- Calligaro KD, DeLaurentis DA, Booth RE, et al. Acute arterial thrombosis associated with total knee arthroplasty. J Vasc Surg 1994;20:927-30; discussion 930-2. [Crossref] [PubMed]
- Holmberg A, Milbrink J, Bergqvist D. Arterial complications after knee arthroplasty: 4 cases and a review of the literature. Acta Orthop Scand 1996;67:75-8. [Crossref] [PubMed]
- Calligaro KD, Dougherty MJ, Ryan S, et al. Acute arterial complications associated with total hip and knee arthroplasty. J Vasc Surg 2003;38:1170-7. [Crossref] [PubMed]
- Padegimas EM, Levicoff EA, McGinley AD, et al. Vascular Complications After Total Knee Arthroplasty-A Single Institutional Experience. J Arthroplasty 2016;31:1583-8. [Crossref] [PubMed]
- Smith DE, McGraw RW, Taylor DC, et al. Arterial complications and total knee arthroplasty. J Am Acad Orthop Surg 2001;9:253-7. [Crossref] [PubMed]
- Bayne CO, Bayne O, Peterson M, et al. Acute arterial thrombosis after bilateral total knee arthroplasty. J Arthroplasty 2008;23:1239.e1-6. [Crossref] [PubMed]
- Ninomiya JT, Dean JC, Goldberg VM. Injury to the popliteal artery and its anatomic location in total knee arthroplasty. J Arthroplasty 1999;14:803-9. [Crossref] [PubMed]
- Abularrage CJ, Weiswasser JM, Dezee KJ, et al. Predictors of lower extremity arterial injury after total knee or total hip arthroplasty. J Vasc Surg 2008;47:803-7; discussion 807-8. [Crossref] [PubMed]
- Jung E, Jim J, Rubin BG, et al. Long-term outcome of endovascular popliteal artery aneurysm repair. Ann Vasc Surg 2010;24:871-5. [Crossref] [PubMed]
- Saunders JH, Subramonia S, Tennant WG. Endovascular repair of iatrogenic popliteal artery trauma. Eur J Trauma Emerg Surg 2012;38:617-22. [Crossref] [PubMed]
- Piffaretti G, Tozzi M, Lomazzi C, et al. Endovascular treatment for traumatic injuries of the peripheral arteries following blunt trauma. Injury 2007;38:1091-7. [Crossref] [PubMed]
Cite this article as: Zhou M, Shen H, Cao G, An S. Popliteal artery thrombosis a TKA complication due to retractor: a report of two cases treated with endovascular reconstruction. Ann Joint 2017;2:59.


