
When it all fails—use the iliac crest
Introduction
Traumatic anterior glenohumeral dislocation is a commonly encountered injury, particularly in young, active patients. The degree of injury to the glenoid resulting from the dislocation may range from soft tissue injury to the anterior labrum (Bankart lesions) to bone involvement along the glenoid rim. Depending on the severity of the injury, the resultant glenoid based lesion may be treated via soft tissue Bankart repair or a procedure to address bone loss.
Soft tissue repairs, such as arthroscopic Bankart repair have a high rate of success when performed for the appropriate indications (1-7). However, recurrent instability is a known complication. A meta-analysis of 26 studies by Harris et al. reported an 11% rate of instability recurrence following arthroscopic Bankart repair in patients without significant glenoid bone loss (8). Several risk factors for recurrent instability after Bankart repair have been identified. Younger age, pre and post-operative participation in competitive contact sports, hyperlaxity, large Hill Sachs lesions, and glenoid bone loss portend a higher rate of failure after arthroscopic Bankart repair (9,10). The instability severity index score (ISIS) uses these risk factors to help identify higher risk patients, who would be better served with an alternative procedure, such as a Latarjet (9).
The Latarjet procedure is commonly indicated as a revision procedure following a failed Bankart repair, or as a primary procedure in patients with high ISIS scores and those with a significant amount of glenoid bone loss. What constitutes “critical bone loss”, thereby necessitating a stabilizing procedure to address the bone defect, has been the subject of recent debate. In 2000, Itoi et al. provided biomechanical evidence that Bankart repair may not restore stability and may lead to stiffness in defects with a width greater than 21% of the glenoid length (11). Additionally, significant bone loss has been defined as defects involving greater than 25% of the inferior glenoid (3,12), or those with a superoinferior length greater than half of the maximum glenoid anteroposterior diameter (13). More recently, in a physically demanding military population, the cut-off for critical bone loss was suggested to be 13.5% (14). Patients with larger defects reported inferior functional outcome scores, though recurrent instability was not necessarily present.
While the calculation of the percentage of glenoid bone loss requires cross-sectional imaging, in some cases such imaging may not be necessary to identify a significant glenoid rim defect. Jankauskas et al. defined the loss of the sclerotic glenoid line on anteroposterior radiographs, a pathognomonic finding with very high specificity for anterior glenoid rim defects (15). Patients with this radiographic finding are often best served with a procedure to address the bone defect, or at a minimum require cross-sectional imaging to calculate the extent of the critical glenoid bone loss.
In many situations with engaging lesions or critical bone loss, the Latarjet procedure is an excellent surgical option. With long-term follow-up, recurrent instability following Latarjet is reported at a rate of 5–6% (16-18). Failures are most often the result of technical errors, which include excessively inferior or medial graft malposition, failure to obtain secure graft fixation with bicortical screws, and reliance on single screw fixation (16,19). Additionally, patients with large glenoid defects or narrow coracoid morphology may be prone to failure of a Latarjet procedure (18).
As discussed herein, the Eden-Hybinette procedure, which utilizes autogenous structural iliac crest bone graft (ICBG) is an excellent option to restore shoulder stability in the setting of a failed Latarjet procedure.
Indications
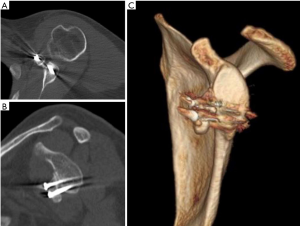
Patients who have failed a Latarjet procedure present unique challenges. With failed union and resorption of the coracoid graft, glenoid bone defects may range from small to quite large without the availability of local bone graph, such as the coracoid (Figure 1). Similarly, a sub-category of patients undergoing their index stabilization procedure may have a significant degree of glenoid bone loss that may be too large to reconstruct with a coracoid graft. The size of glenoid defect over which a Latarjet procedure may not restore stability has not been clearly defined in the literature. In such cases where the degree of glenoid bone loss is large or the coracoid morphology prevents its use for reconstruction, the Eden-Hybinette procedure may be a better option.
With careful technique, the iliac crest graft size available for reconstruction is large, enabling the surgeon to address sizeable defects. Graft availability comes at the cost of donor site morbidity, which may include prolonged pain or injury to the lateral femoral cutaneous nerve if the graft is harvested in close proximity to the anterior superior iliac spine (ASIS). After harvesting the tricortical ICBG, it can be contoured to match the site of the glenoid deficiency. The concavity of the inner table may also be a closer match to that of the glenoid, providing a more congruent reconstruction (20). Furthermore, use of autogenous structural ICBG is a cost effective alternative to use of allograft, with lower risk of disease transmission.
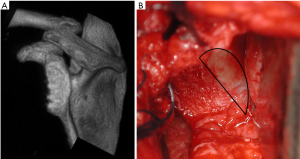
We prefer the Eden-Hybinette procedure in patients who have failed a Latarjet procedure, or as an index procedure in patients with glenoid bone loss exceeding 40% (Figure 2), abnormal coracoid morphology, or an unreconstructable glenoid fracture with instability. Patients with uncontrolled seizures, active infections, and those who are unable to follow post-operative precautions are not recommended for this procedure.
Operative planning, technique, and post-operative care
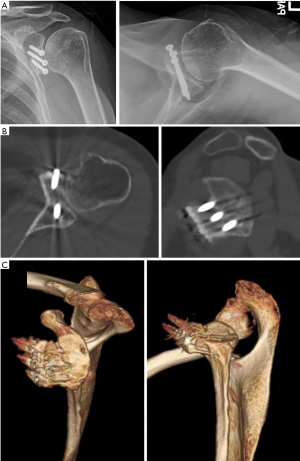
In patients with suspected bone loss, we routinely get computed tomography (CT) with three-dimensional (3D) reconstructions. We use this imaging modality to accurately determine the shape of the glenoid and the extent of bone loss. In cases of substantial bone loss, provisional measurements of the length and width of the defect can be taken to determine the size of bone graft needed. CT scans can also be useful in identifying abnormal coracoid morphology.
For the Eden-Hybinette procedure, we prefer an open approach, though arthroscopic techniques have been described as well. The patient is placed in the beach chair position, sitting upright with only 30 degrees of elevation. Lower degrees of elevation may aid in keeping a particularly unstable shoulder in a more reduced position and also provide access to harvest the ICBG. We also do not sit obese patients as far upright as it may make accessing the iliac crest more challenging. The lateral support on the operative side often needs to be adjusted so that it supports the patient, but does not impede access to the iliac crest. A pneumatic arm positioner is used for the operative arm to aid in aid in arm positioning throughout the procedure.
After prepping and draping both the operative shoulder and the iliac crest, a standard deltopectoral approach is made. As this procedure is often done in the setting of a failed Latarjet procedure, it is important to be cognizant of the altered surgical field. In addition to the scarring from previous procedures, the deltopectoral interval may not be readily identifiable, and the coracoid and conjoined tendon are not reliable landmarks. The axillary nerve is then carefully identified and protected.
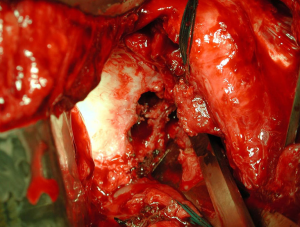
The subscapularis is managed with either a split in line with its fibers at its superoinferior midpoint or a tenotomy. A subscapularis split may be a better option, particularly if a tenotomy was used previously such as at the time of a Latarjet. If instead a tenotomy is used during the exposure, the subscapularis should be dissected from the underlying capsule from lateral to medial using needle-tip electrocautery. In the setting of a failed Latarjet procedure, the conjoint tendon will likely be scarred into the subscapularis and does not need to be disturbed. The capsule is then released along the neck of the humerus. A Fukuda retractor is used to posteriorly displace the humeral head and a cobra retractor is placed over the anterior glenoid. The glenoid is then prepared by removing any screws and un-united coracoid graft (Figure 3). A burr or curved Lambotte osteotome is used to remove any prominent bone and abrade the surface to create a flat surface of bleeding bone for placement of the graft. After preparing the glenoid surface, measurements of the defect are taken to verify the size of graft needed. Once the glenoid has been prepared, we proceed with harvesting the iliac crest graft.
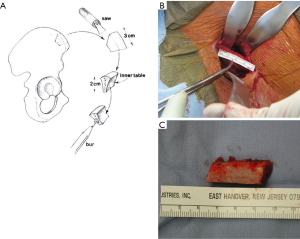
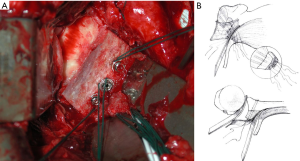
In order to facilitate the ICBG harvest the patient can be placed in a more supine position. The incision should be well posterior to the ASIS so as to avoid injury to the lateral femoral cutaneous nerve. An oblique incision is made two centimeters lateral to the ASIS extending approximately 5 centimeters laterally. The inner and outer tables are exposed with the aid of blunt retractors (Figure 4). An oscillating saw and osteotome are used to remove a tricortical wedge of bone that is appropriate in size for the patient’s glenoid defect. The graft is then prepared, with the concavity of the inner table aligning with the glenoid articular surface. This requires some planning and fitting of the graft so as to restore proper glenoid concavity. All soft tissue must be meticulously removed and the graft is carefully contoured to match the defect on the bony interface.
The graft is then positioned along the anterior glenoid, congruent with or slightly medial to the articular surface. If the graft is positioned too laterally, the patient will be at risk of developing rapidly progressive arthritis. The graft is then secured with at least two 3.5 mm cortical screws with washers oriented parallel to the articular surface. Before fully seating each screw, a #2 fiberwire suture is placed around the screw and washer for repair of the capsular sleeve down to the graft (Figure 5). Due to the bulk of the graft, lateral repair of the capsule may not be possible. If this is the case, the capsule is secured to the undersurface of the subscapularis. The subscapularis is then repaired with either a side-to-side closure for a split, or transosseous suture repair over a suture button for a tenotomy.
Postoperative protocol is dictated based on how the subscapularis was managed during the exposure. In the case of a subscapularis split, the patient is kept in a sling for 4 weeks, though pendulums are allowed immediately. After 2 weeks, formal physical therapy begins with passive range of motion followed by active range of motion with assisted stretching at week 4. Strengthening is initiated after 2 months. Physical therapy is delayed for 4–6 weeks if a subscapularis tenotomy was performed. Pendulum exercises are allowed after the first week. After the 4 to 6 weeks period of immobilization, the patient may begin supervised physical therapy for active and passive range of motion and they may begin using the arm of activities of daily living. Strengthening is delayed until 3 months. A CT scan may be ordered after 6 months to confirm graft union (Figure 6). Contact sports are typically delayed until at least 8 months from surgery.
Outcomes
The Eden-Hybinette procedure has proven to be effective at restoring stability following failed Latarjet procedures. Warner et al. reported improvement in all recorded functional outcome scores (ASES, UCLA, and Rowe scores) in a series of 11 patients. All patients in this series returned to pre-injury levels of sport without recurrence of instability (7). Lunn et al. reported good to excellent results in 79% of 46 patients who underwent a modified Eden-Hybinette after a failed Latarjet (21). Successful long-term results have also been reported in a series of 48 patients, 28 of which were revision cases. At a mean of 9 years follow-up, 7% of patients reported subjective instability and only 1 patient had sustained a redislocation. Twenty percent of patients had radiographic progression of arthritis by one stage in the Samilson and Prieto classification. One patient developed subscapularis insufficiency and two developed either Goutallier stage 3 or 4 subscapularis atrophy (22). Early results of an arthroscopic technique have also shown some success in a series of 18 patients (23). Sixty-seven percent of the patients had good or excellent results, though 42% had a positive apprehension test postoperatively. Regardless of technique, restoration of stability and a successful outcome of the Eden-Hybinette are dependent on bony union of the iliac crest graft to the glenoid.
Conclusions
Arthroscopic Bankart repairs and Latarjet procedures have a high rate of success when performed in the appropriate patient. Consideration of patient-specific factors and goals, along with imaging to determine the presence of significant bony defects is critical for indicating the proper procedure. In the subset of patients in which the Latarjet procedure fails with recurrent instability, the Eden-Hybinette procedure using autologous structural ICBG is an excellent option. With proper technique, the available iliac crest graft size can be quite substantial, enabling treatment of very large glenoid defects. The surgeon should be prepared to approach this complicated procedure with caution as the surgical field can be disorienting from the altered anatomy. “When it all fails”, the Eden-Hybinette procedure has proven to be very successful in restoring stability.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Albert Lin and Jason J. Shin) for the series “Trends in Anterior Shoulder Instability” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.10.02). The series “Trends in Anterior Shoulder Instability” was commissioned by the editorial office without any funding or sponsorship. WD reports grants from Arthrex, grants from Smith & Nephew, during the conduct of the study. JJPW reports personal fees from DePuy, Johnson & Johnson, personal fees from Stryker, grants from Arthrex, grants from Smith & Nephew, during the conduct of the study, personal fees from Wright Medical, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Warner JJ, Johnson D, Miller M, et al. Technique for selecting capsular tightness in repair of anterior-inferior shoulder instability. J Shoulder Elbow Surg 1995;4:352-64. [Crossref] [PubMed]
- Gill TJ, Micheli LJ, Gebhard F, et al. Bankart repair for anterior instability of the shoulder: long-term outcome. J Bone Joint Surg Am 1997;79:850-7. [Crossref] [PubMed]
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94. [Crossref] [PubMed]
- Gartsman GM, Roddey TS, Hammerman SM. Arthroscopic treatment of anterior-inferior glenohumeral instability. Two to five-year follow-up. J Bone Joint Surg Am 2000;82-A:991-1003. [Crossref] [PubMed]
- Kim SH, Ha KI, Cho YB, et al. Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg Am 2003;85-A:1511-8. [Crossref] [PubMed]
- Millett PJ, Clavert P, Warner JJ. Arthroscopic management of anterior, posterior, and multidirectional shoulder instability: pearls and pitfalls. Arthroscopy 2003;19:86-93. [Crossref] [PubMed]
- Warner JJ, Gill TJ, O'hollerhan JD, et al. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med 2006;34:205-12. [Crossref] [PubMed]
- Harris JD, Gupta AK, Mall NA, et al. Long-term outcomes after Bankart shoulder stabilization. Arthroscopy 2013;29:920-33. [Crossref] [PubMed]
- Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 2007;89:1470-7. [Crossref] [PubMed]
- Tauber M, Resch H, Forstner R, et al. Reasons for failure after surgical repair of anterior shoulder instability. J Shoulder Elbow Surg 2004;13:279-85. [Crossref] [PubMed]
- Itoi E, Lee SB, Berglund LJ, et al. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 2000;82:35-46. [Crossref] [PubMed]
- Burkhart SS, Debeer JF, Tehrany AM, et al. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy 2002;18:488-91. [Crossref] [PubMed]
- Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res 2002;65-76. [Crossref] [PubMed]
- Shaha JS, Cook JB, Song DJ, et al. Redefining "Critical" Bone Loss in Shoulder Instability: Functional Outcomes Worsen With "Subcritical" Bone Loss. Am J Sports Med 2015;43:1719-25. [Crossref] [PubMed]
- Jankauskas L, Rüdiger HA, Pfirrmann CW, et al. Loss of the sclerotic line of the glenoid on anteroposterior radiographs of the shoulder: a diagnostic sign for an osseous defect of the anterior glenoid rim. J Shoulder Elbow Surg 2010;19:151-6. [Crossref] [PubMed]
- Hovelius L, Sandström B, Olofsson A, et al. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg 2012;21:647-60. [Crossref] [PubMed]
- Mizuno N, Denard PJ, Raiss P, et al. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg 2014;23:1691-9. [Crossref] [PubMed]
- Mook WR, Petri M, Greenspoon JA, et al. Clinical and Anatomic Predictors of Outcomes After the Latarjet Procedure for the Treatment of Anterior Glenohumeral Instability With Combined Glenoid and Humeral Bone Defects. Am J Sports Med 2016;44:1407-16. [Crossref] [PubMed]
- Gasbarro G, Giugale JM, Walch G, et al. Predictive Surgical Reasons for Failure After Coracoid Process Transfers. Orthop J Sports Med 2016;4:2325967116676795 [Crossref] [PubMed]
- Ghodadra N, Gupta A, Romeo AA, et al. Normalization of glenohumeral articular contact pressures after Latarjet or iliac crest bone-grafting. J Bone Joint Surg Am 2010;92:1478-89. [Crossref] [PubMed]
- Lunn JV, Castellano-Rosa J, Walch G. Recurrent anterior dislocation after the Latarjet procedure: outcome after revision using a modified Eden-Hybinette operation. J Shoulder Elbow Surg 2008;17:744-50. [Crossref] [PubMed]
- Steffen V, Hertel R. Rim reconstruction with autogenous iliac crest for anterior glenoid deficiency: forty-three instability cases followed for 5-19 years. J Shoulder Elbow Surg 2013;22:550-9. [Crossref] [PubMed]
- Giannakos A, Vezeridis PS, Schwartz DG, et al. All-Arthroscopic Revision Eden-Hybinette Procedure for Failed Instability Surgery: Technique and Preliminary Results. Arthroscopy 2017;33:39-48. [Crossref] [PubMed]
Cite this article as: Daner WE 3rd, Chang MJ, Fox HM, Higgins LD, Warner JJP. When it all fails—use the iliac crest. Ann Joint 2017;2:60.


