Remplissage—when and how to fill in the defect
Introduction/background
The complex interaction of dynamic and static stabilizers of the glenohumeral joint promote superior range of motion yet given the anatomic bony structures, the shoulder is susceptible to instability. Traumatic unidirectional instability events most commonly lead to anteroinferior labral and glenoid injury, with capsulolabral avulsions known as soft-tissue Bankart lesions. However, with unidirectional instability, bony lesions, including bony Bankart defects and Hill-Sachs lesions on the humerus can arise, contributing to more complex shoulder pathology (1-3).
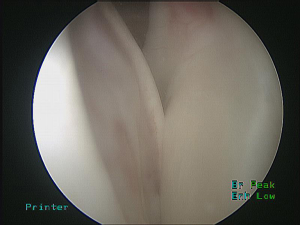
The first descriptions of humeral head defects in the literature appeared in the 19th century by Flower, Broca, and Hartmann; a humeral head defect sustained after glenohumeral dislocation (4,5). In 1941 Hills and Sachs further characterized the posterior-superior fractures of the humerus ensuing from impaction of the posterior-superior aspect of the humeral head against the dense anteroinferior glenoid cortical rim (6) (Figure 1). Subsequently, these lesions were further explored, with demonstration of engaging Hills-Sachs lesions that occur when the long axis of the humeral head defect is parallel to the anterior glenoid rim, now better characterized as Off-track lesions, allowing the humeral head defect to fall off of the glenoid fossa (7-9) in essence becoming levered anteroinferiorly to the glenoid fossa (Figures 1,2). This research provides an understanding for the mechanism through which recurrent anterior dislocations can occur.
Hill-Sachs lesions can be seen in 65–80% of initial glenohumeral dislocations, and up to 100% of recurrent instability episodes (10,11). Given the complex three-dimensional nature of such lesions, failure rates as high as 67% have been reported with arthroscopic Bankart repair alone (8). Therefore, several procedures have been proposed to address these humeral head defects including humeral head osteotomy, osteochondral allograft, humeroplasty, anterior capsular plication, and limited resurfacing arthroplasty (12,13). While many of these procedures do result in acceptable clinical outcomes (14), they are performed in an open surgical approach and are associated with complications such as implant, malfunction, nonunion, and glenohumeral osteoarthritis (15). More recently, an arthroscopic technique which involves soft tissue interposition into the humeral defect, known as remplissage (French: to fill in) procedure, has been developed to prevent Hill-Sachs lesion engaging on the glenoid rim (16). This review will discuss the current literature surrounding the arthroscopic remplissage procedure and address the gaps in knowledge concerning this relatively new procedure.
Outline of technique
While the term remplissage was coined by Purchase et al. when describing their arthroscopic technique in 2008, the open procedure was originally described by Connolly in 1972 (17). Connolly proposed open tenodesis of the posterior joint capsule and infraspinatus tendon into the humeral defect, which converts the lesion from an intra-articular to an extra-articular defect, thus preventing engagement of the Hill-Sachs lesion on the glenoid rim. Moreover, limited anterior translation is accomplished, overall conferring enhanced glenohumeral joint stability despite the incurred bony defect(s).
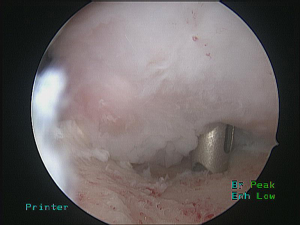
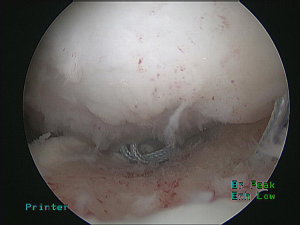
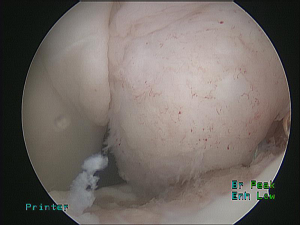
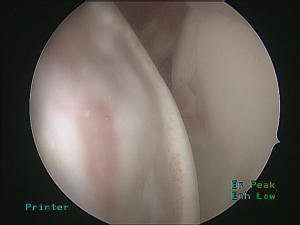
This technique was first modified for arthroscopic surgery by Purchase et al., to treat “traumatic shoulder instability in patients with glenoid bone loss and a large Hill-Sachs lesion.” (16,18). Briefly, their technique consisted of positioning the patient in the lateral decubitus position before establishing a posterior portal at the lateral convexity of the humeral head. This portal serves as an arthroscopic viewing portal as well as a working portal, allowing adequate access to the lesion. Following creation of anteroinferior and anterosuperior portals, the camera is placed in the anterosuperior portal. Utilizing the posterior portal, the lesion is eburnated with a bur, removing only a minimal amount of bone. In preparation for a Bankart repair, the anterior labrum and glenoid neck were prepared before proceeding with remplissage. Subsequently, a cannula is placed in the posterior portal through the deltoid with care to avoid penetration of the infraspinatus and capsule. Through this portal, an anchor can be placed in the inferior aspect of the humeral defect (Figure 3). Next, a penetrating grasper is passed through the tendon and posterior capsule, about 1 cm inferior to the initial portal entry site, to retrieve one suture limb (Figure 4). Then, a second anchor is placed in the superior aspect of the defect and a suture limb passed in an identical fashion. The inferior sutures are tied first, followed by the superior sutures, ensuring that all knots remained extra-articular (Figure 5). In this manner, the infraspinatus and capsule are sunk drawn into the lesion via mattress sutures. After completion of the remplissage, Bankart lesions are then repaired (Figure 6).
In 2009, Koo et al. described the first large modification to the arthroscopic technique with the goal of creating a larger footprint of fixation (19). Their technique, known as the double-pulley remplissage technique, begins in comparable fashion to that described by Purchase and Wolf. The patient is placed in the lateral decubitus position and similar portals are created. Afterwards a subacromial bursectomy is performed in order to prevent interference of bursal tissue during knot-tying. In contrast to the original procedure, a Bankart labral lesion is approached with placement suture anchors. These sutures are retrieved through the anteroinferior portal and left untied. The Hill-Sachs lesion is freshened with a bur placed in the posterior portal and afterwards, a posterior cannula is placed through the deltoid without penetration of the infraspinatus tendon or capsule. Following placement of two transtendon suture anchors in the Hill-Sachs lesion, the Bankart repair sutures are tied. Only thereafter are the remplissage sutures tied above the infraspinatus tendon from within the subacromial space, through use of the transtendon double-pulley technique. This technique ties one strand from each suture anchor over a switching stick. The two remaining free ends are pulled, effectively using the anchor eyelets as pulleys to slide the knot onto the infraspinatus in double-mattress fashion.
While the two procedures detailed above are the main iterations of the remplissage technique, there have since been many variations published. Camp et al. described a variation of the original remplissage technique, incorporating only the capsule into the repair as a method of minimizing undue stress on the rotator cuff (20). Another version utilizes a partial articular supraspinatus tendon avulsion (PASTA) repair kit to avoid the need to retrieve sutures in the subacromial space, eluding formation of larger rotator cuff defects, all the while providing direct visualization of the fixation of the capsule and cuff onto the Hill-Sachs lesion—all advantages worth considering (21). One last modified version of the original procedure was described by Bhatia, who not only placed the patient in a beach-chair position, but also utilized a double suture knot, called the double barrel knot, to produce a more predictable amount of repair tensioning (22).
There have also been several variations of the remplissage procedure Koo et al. described. Alexander et al. modified Koo’s technique through the use of a single percutaneous skin and deltoid incision, which is exploited for placement of both anchors (23). Other modifications, with beach-chair positioning of the patient have been described (24). Lastly, a combined arthroscopic Hill-Sachs remplissage with open Latarjet procedure performed in patients with combined bony defects that are “off-track” (9,25) has been described. In this setting, suture anchors are arthroscopically placed in the humeral defect, the open coracoid transfer is completed, and then the tendinocapsular fixation into the Hill-Sachs defect is performed. While these techniques have different technical advantages, none have been shown to be superior in terms of outcomes, and choice of technique is mostly dictated by surgeon preference for positioning and efficiency.
Indications
Studies that have looked at the efficacy of this procedure have varying indications. The first study to outline this procedure by Purchase and Wolf was in a series of patients with traumatic anterior shoulder instability who had bony lesions of the posterior humeral head (Hill-Sachs) and <25% anterior glenoid deficiency (Bigliani grade IIIA), in which the Hill-Sachs lesion engaged the glenoid at the time of surgery (16,18). Purchase suggested that remplissage is an effective arthroscopic augment to Latarjet or similar bone grafting procedures done for substantial glenoid bone loss. Subsequently, several studies have been described, which investigate the outcomes of the remplissage procedure, using the same indications (26-32).
A systematic review of this procedure was described by Buza et al. (33). All of the studies included in the review agreed that the authors preferred to see evidence of the Hill-Sachs lesion on preoperative imaging to consider remplissage but the final decision to perform the procedure was based on the engagement of the humeral head defect on the anterior glenoid rim during dynamic arthroscopic assessment. Furthermore, all the included studies in this review agreed that patients needed to be without substantial glenoid bone loss: most cited less than 25% osseous deficiency of the glenoid for the remplissage procedure to be considered.
More recently, the concept of the glenoid track has been described by Itoi et al. and may serve as an indication for remplissage (9). Through use of 3-D CT, Itoi et al. demonstrated that as the arm was raised the glenoid contact area shifted to the superolateral portion of the articular surface of the humeral head and defined this contact area as the glenoid track. They further demonstrated those Hill-Sachs lesions that are within the medial margin of the glenoid track allow for bony stability and non-engagement defined an “on-track” lesion, while those Hill-Sachs lesions that are medial to the medial margin of the glenoid track cause loss of bony support and engage the glenoid defined as an “off-track” lesion. Utilizing the glenoid track concept, Hartzler et al. conducted a study on frozen cadaveric shoulders to determine if remplissage could be utilized for “off-track” Hill-Sachs lesions (34). They found that with a 15% glenoid defect, adding remplissage to Bankart repair prevented engagement throughout rotation for all eight shoulders with engaging lesions, especially at end-rotation where Bankart repair alone prevented engagement in none of the shoulders. This study demonstrates that assessment of the glenoid track may also serve as an indication for remplissage repair.
A recent survey distributed to members of the American Shoulder and Elbow Society further demonstrates the increasing consensus that in the setting of engaging Hill-Sachs lesions, remplissage procedure should be considered (35). In this survey, 60% of surgeons recommended a remplissage procedure when provided with a case scenario detailing a “weekend warrior” with a large engaging Hill-Sachs lesion.
While most studies suggest decision of whether or not to perform the remplissage procedure should be based on the aforementioned criteria, there are some studies that include the Instability Severity Index Score (ISIS), a preoperative evaluation tool (36) that determines the risk of failure following isolated arthroscopic Bankart repair. Included in the ISIS system is an assessment of Hill-Sachs lesion, where 2 points (of total 10 points) are allotted for its presence on AP radiograph, which may be used to determine indication for remplissage (36). Nourissat et al. conducted a prospective study that investigated Latarjet alone vs Latarjet and remplissage for patients with anterior shoulder instability and utilized ISIS to determine which patients should receive remplissage procedure in addition to the coracoid transfer (37).
Lastly, the preoperative physical exam under anesthesia can be helpful in this decision-making process. If the lesion locks during the anterior load-and-shift test performed with the arm abducted in the scapular plane, an engaging Hill-Sach has been demonstrated (20). This can also be confirmed intraoperatively with the arthroscope in the glenohumeral joint, while taking that patient through range of motion testing.
Outcomes
The advantages of the remplissage technique over other techniques to repair posterior humeral defects are the minimally invasive nature of using an arthroscopic approach, shorter recovery time, and avoidance of the complications associated with bone grafting, as well as excellent clinical outcomes. Many studies have investigated these outcomes in depth utilizing validated shoulder scores and range of motion measurements. The findings of Wolf et al. (18) on the remplissage technique demonstrated a mean postoperative Rowe score of 92, Constant score of 92, and a Western Ontario Shoulder Stability Index Score of 224. Only 4.4% of the cohort had recurrence of shoulder instability resulting from traumatic events while participating in sports, and no limitation to external rotation was observed in the cohort.
Since this initial study, multiple other studies have confirmed that the remplissage procedure provides significant anterior shoulder stability and improved functionality, with minimal limitation in range of motion. Zhu et al. found an average loss of 1.9 degrees of external rotation, and significant improvement in the ASES (84.7 vs. 96.0), Constant (93.3 vs. 97.8) and Rowe (36.8 vs. 89.8) scores (26). Brilakis et al. had similar findings, demonstrating ASES scores that increased by a mean of 20 points and Rowe scores that increased by more than 50 points (29).
Many systematic reviews have also compiled the outcomes of remplissage procedures. One by Buza et al. demonstrated a substantial increase in mean Rowe scores postoperatively (mean of 36.1 preoperatively to 87.6 postoperatively), 89% of patients had a good to excellent postoperative Walch-Duplay score, and 80% of patients had a successful return to sport (33). More importantly, while forward elevation increased from 165.7° preoperatively to 170.3° postoperatively, the mean external rotation, initially thought to yield significant impairment due to tethering of the infraspinatus tendon, only decreased from 57.6° to 54.6°. The reported recurrence rate of these six studies was minimal (5.4%). Leroux et al. conducted another systematic review that not only demonstrated a low rate of recurrent instability (3.4%), but also high patient satisfaction after remplissage (98.4%) (38). Lastly, Rashid et al. showed a mean recurrence rate of 4.2% with a mean decrease in external rotation of 11° and a mean decrease in internal rotation of 0.9° (39).
Remplissage has also been compared to other procedures that treat anterior shoulder instability. Nourissat et al. investigated the effect of remplissage on shoulder range of motion as compared to arthroscopic Bankart alone (37). They found that the average difference between the patients range of motion in the operative arm was greater in the remplissage group, and this was not statistically significant. They also found no difference in recurrence rates of shoulder dislocation. Franceschi et al. compared arthroscopic remplissage with Bankart verses Bankart alone. In their cohort, no instability recurrence was seen in the remplissage group while the Bankart alone group had five recurrent episodes of instability, a rate of 20% (28). Garcia et al. found an even higher rate of failure in patients undergoing Bankart alone for large engaging Hill-Sachs lesions, with 57% of patients failing after the Bankart procedure verses 20% in patients who underwent remplissage with Bankart repair (31).
Remplissage has also been compared to osteochondral substitute grafting. Garcia et al. demonstrated the remplissage group reported significantly better WOSI scores (74.7) when compared to patients who underwent grafting (50.4), when controlling for sex, age, lesion size, and follow-up differences (40). Remplissage has also been compared to Latarjet procedures. However this has only been reported in cadaveric studies, which have not shown a difference in instability (41,42).
Excellent outcomes in patients who participate in sports have also contributed to the widespread adoption of the remplissage procedure. Boileau et al. demonstrated an average loss in external rotation of 8° with the arm in adduction and 9° with the arm in abduction, and found a return to sports rate of 90%, with 70% of these patients returning at the same preoperative level (43). They reported only 1 patient out of 47 who experienced recurrence of shoulder instability. Garcia et al. also investigated return to sports post remplissage procedure in throwing athletes. Ninety-five percent of patients were able to return to sports, with 81% returning to prior level. Overall, 65% reported an impact on their ability to throw, with 34.5% reporting decreased velocity, 17.2% reporting pain with throwing, and 58.6% reporting stiffness (44). Therefore, caution is advised when considering remplissage for the throwing athlete.
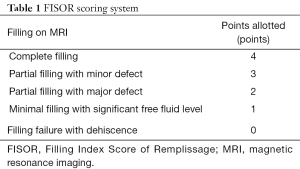
In terms of the intended anatomical aim of the technique—to fill the humeral head defect with tendon—multiple studies have demonstrated this technique’s success. Park et al. took postoperative 3-T protocol MRI’s with the shoulder in the abduction-external rotation (ABER) and neutral positions at the time of the latest clinical examination. The humeral head defect was measured as an ellipsoid mathematical formula using the largest measurements at coronal, sagittal, and axial images as vertical, major, and minor axis values. The percentage fill by the tendon was measured based on previously outlined ellipsoid volume calculations and categorized as a percentage of the defect size: 0–25%, 25–50%, 50–75%, and 75–100%. They found that the technique filled anywhere from 75–100% of the defects repaired with remplissage (45). A similar study utilized MRI images to create a filling index score, Filling Index Score of Remplissage (FISOR), that was used to assess the structural outcomes of the remplissage procedure. The study enrolled 23 patients who underwent arthroscopic Bankart repair with a remplissage procedure for a large or engaging Hill-Sachs lesion confirmed by arthroscopic findings. The postoperative filling index was classified into five categories by axial and sagittal views of T2-weighted images on magnetic resonance arthrography (Table 1). FISOR was calculated from the sum of points in the axial and sagittal planes. The FISOR was 8 points in 13 patients, 7 points in 2 patients, 6 points in 3 patients, 5 points in 1 patient, 4 points in 1 patient, 3 points in 1 patient, 2 points in 1 patient, and 0 point in 1 patient. Further studies may correlate this new filling index score, FISOR, with clinical outcomes (46).
Full table
Complications
Overall, complications following remplissage are not very common with multiple studies citing almost no complications (18,33,47). The most commonly reported complication of the remplissage procedure has been loss of range of motion, specifically external rotation with arm at side of trunk. Most studies quote a minimal decrease in external rotation ranging anywhere from a loss of 1.9° to 11° (26,33,39,43). In at least one case study, a patient had a severe loss of external rotation that was still present 2 years following this procedure which necessitated arthroscopic release of the tenodesed infraspinatus (48). Yet, patients with severe loss of external rotation are not widely described. Other studies have shown no significant difference in external rotation postoperatively (18). Decreased external rotation is thought to be caused by inclusion of muscle fibers of the infraspinatus tendon or the musculotendinous junction, making it more of a myodesis. Cadaveric studies by Elkinson et al. and Garcia et al. have shown there is variability in accurately placing sutures in the infraspinatus tendon, and found decreased glenohumeral stiffness could be avoided just by placing sutures 1 cm lateral to the authors’ initial fixation site (49,50). Currently, there are new techniques that use the posterolateral acromion as an anatomic landmark to increase the accuracy of suture passage through the infraspinatus tendon (51). Furthermore, recent cadaveric studies have demonstrated this restriction of motion is more pronounced for larger Hill-Sachs lesions, as expected, which should prompt the surgeon to warn such patients preoperatively about the likelihood of this restriction of motion postoperatively (52).
In addition to range of motion deficits, posterior shoulder pain has been reported as another complication of this procedure. In a study by Nourissat et al., they found persistent posterior shoulder pain in one third of patients at 2 years of follow-up (37). The pain is thought to be related to impingement or to partial healing of the tendon. No other studies have reported such a significant incidence of posterior shoulder pain. Since this study, others have suggested that inaccurate suture placement may also play a role in pain generation (50).
Infraspinatus weakness after this procedure has also been reported. Merolla et al. looked at the infraspinatus strength test and infraspinatus scapular retraction test, and found the remplissage group had an average maximum infraspinatus strength test measurement of 0.4 kg less than their control group, and an average maximum infraspinatus scapular retraction test of 0.2 kg less than their control group. Both differences were not found to be statistically significant (30).
To our knowledge, the literature on remplissage procedure complications has shown only one instance of postoperative biceps tenosynovitis, and one incident of ulnar nerve palsy (29,33). A reoperation was required in the former case, namely biceps tenodesis, which brought about resolution, while the latter was self-limiting in nature.
Discussion and conclusions
The remplissage procedure is an arthroscopic technique used to treat anterior shoulder instability in patients with large Hills-Sachs lesions. Current indications for the procedure focus on patients with recurrent instability with an engaging Hill-Sachs lesion and minimal anterior glenoid deficiency, with intraoperative findings consistent with this diagnosis. The technique involves the use of arthroscopic tools to incorporate the tendon of infraspinatus and capsule within the humeral lesion to prevent continued engagement on the anterior glenoid and subsequent shoulder instability; in essence taking an intra-articular defect and turning it into an extra-articular defect. While the technical aspects of the technique can be modified, the procedure always involves the use of two anchors to fixate the tendon within defect. Different techniques can be utilized for efficiency or for patients with coexisting bony defects in addition to the humeral defect. Outcomes for this procedure have been favorable. For patients with large engaging Hill-Sachs lesions, remplissage has been proven to be superior to Bankart repair alone. Most patients have excellent outcome scores with minimal recurrent anterior shoulder instability reported. Furthermore, range of motion does not seem to be significantly decreased in most patients. The complications include minimal deficits in range of motion, namely a decrease in external rotation.
Gaps in knowledge concerning this technique remain, with some controversy regarding cut-off size of Hill-Sachs lesion for which the remplissage technique is most effective. Furthermore, while there is concern for postoperative deficits in range of motion, this has not been shown to be statistically significant, and only clearly demonstrated in cadaveric studies. Prospective randomized cohort studies could further elucidate the impact on patient range of motion, pain, and shoulder outcome scores. Lastly, while this procedure seems to have gained widespread acceptance among the shoulder surgeon community, there have been no studies looking at the trends of the remplissage procedure within the United States in treating anterior shoulder instability. Nonetheless, remplissage is a successful arthroscopic procedure for anterior shoulder instability. Future research should be directed to better refine the indications, further describe potential complications, and supplement an understanding of its utilization in the population of patients with anterior shoulder instability.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Albert Lin and Jason J. Shin) for the series “Trends in Anterior Shoulder Instability” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.10.04). The series “Trends in Anterior Shoulder Instability” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bankart AS. Recurrent or habitual dislocation of the shoulder-joint. Br Med J 1923;2:1132-3. [Crossref] [PubMed]
- Lynch JR, Clinton JM, Dewing CB, et al. Treatment of osseous defects associated with anterior shoulder instability. J Shoulder Elbow Surg 2009;18:317-28. [Crossref] [PubMed]
- Bushnell BD, Creighton RA, Herring MM. Bony instability of the shoulder. Arthroscopy 2008;24:1061-73. [Crossref] [PubMed]
- Broca A, Hartmann H. Contribution a’ l’e’tude des luxations de l’e’paule. Bull Soc Anat Paris 1890;4:416-23.
- Flower WH. On the pathological changes produced in the shoulder-joint by traumatic dislocation: as derived from an examination of all the specimens illustrating this injury in the museums of London. London: s.n., 1861:179.
- Hill HA, Sachs MD. The Grooved Defect of the Humeral Head. Radiology 1940;35:690-700. [Crossref]
- Palmer I, Widen A. The bone block method for recurrent dislocation of the shoulder joint. J Bone Joint Surg Br 1948;30B:53-8. [PubMed]
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94. [Crossref] [PubMed]
- Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy 2014;30:90-8. [Crossref] [PubMed]
- Antonio GE, Griffith JF, Yu AB, et al. First-time shoulder dislocation: High prevalence of labral injury and age-related differences revealed by MR arthrography. J Magn Reson Imaging 2007;26:983-91. [Crossref] [PubMed]
- Taylor DC, Arciero RA. Pathologic changes associated with shoulder dislocations. Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. Am J Sports Med 1997;25:306-11. [Crossref] [PubMed]
- Armitage MS, Faber KJ, Drosdowech DS, et al. Humeral head bone defects: remplissage, allograft, and arthroplasty. Orthop Clin North Am 2010;41:417-25. [Crossref] [PubMed]
- Weber BG, Simpson LA, Hardegger F. Rotational humeral osteotomy for recurrent anterior dislocation of the shoulder associated with a large Hill-Sachs lesion. J Bone Joint Surg Am 1984;66:1443-50. [Crossref] [PubMed]
- Hawkins RJ, Angelo RL. Glenohumeral osteoarthrosis. A late complication of the Putti-Platt repair. J Bone Joint Surg Am 1990;72:1193-7. [Crossref] [PubMed]
- Flatow EL, Miniaci A, Evans PJ, et al. Instability of the shoulder: complex problems and failed repairs: Part II. Failed repairs. Instr Course Lect 1998;47:113-25. [PubMed]
- Purchase RJ, Wolf EM, Hobgood ER, et al. Hill-sachs "remplissage": an arthroscopic solution for the engaging hill-sachs lesion. Arthroscopy 2008;24:723-6. [Crossref] [PubMed]
- Connolly JF. Humeral head defects associated with shoulder dislocations: their diagnostic and surgical significance. Instr Course Lect 1972;21:42-54.
- Wolf EM, Arianjam A. Hill-Sachs remplissage, an arthroscopic solution for the engaging Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elbow Surg 2014;23:814-20. [Crossref] [PubMed]
- Koo SS, Burkhart SS, Ochoa E. Arthroscopic double-pulley remplissage technique for engaging Hill-Sachs lesions in anterior shoulder instability repairs. Arthroscopy 2009;25:1343-8. [Crossref] [PubMed]
- Camp CL, Dahm DL, Krych AJ. Arthroscopic Remplissage for Engaging Hill-Sachs Lesions in Patients With Anterior Shoulder Instability. Arthrosc Tech 2015;4:e499-502. [Crossref] [PubMed]
- Tan BH, Kumar VP. The Arthroscopic Hill-Sachs Remplissage: A Technique Using a PASTA Repair Kit. Arthrosc Tech 2016;5:e573-8. [Crossref] [PubMed]
- Bhatia DN. Double-Barrel Remplissage: An Arthroscopic All-Intra-articular Technique Using the Double-Barrel Knot for Anterior Shoulder Instability. Arthrosc Tech 2015;4:e65-70. [Crossref] [PubMed]
- Alexander TC, Beicker C, Tokish JM. Arthroscopic Remplissage for Moderate-Size Hill-Sachs Lesion. Arthrosc Tech 2016;5:e975-9. [Crossref] [PubMed]
- Parnes N, Carey PA, Schumacher C, et al. Arthroscopic Transtendinous Double-Pulley Remplissage Technique in the Beach-Chair Position for Large Hill-Sachs Lesions. Arthrosc Tech 2015;4:e305-9. [Crossref] [PubMed]
- Katthagen JC, Anavian J, Tahal DS, et al. Arthroscopic Remplissage and Open Latarjet Procedure for the Treatment of Anterior Glenohumeral Instability With Severe Bipolar Bone Loss. Arthrosc Tech 2016;5:e1135-41. [Crossref] [PubMed]
- Zhu YM, Lu Y, Zhang J, et al. Arthroscopic Bankart repair combined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: a report of 49 cases with a minimum 2-year follow-up. Am J Sports Med 2011;39:1640-7. [Crossref] [PubMed]
- Haviv B, Mayo L, Biggs D. Outcomes of arthroscopic “remplissage”: capsulotenodesis of the engaging large Hill-Sachs lesion. J Orthop Surg Res 2011;6:29. [Crossref] [PubMed]
- Franceschi F, Papalia R, Rizzello G, et al. Remplissage repair--new frontiers in the prevention of recurrent shoulder instability: a 2-year follow-up comparative study. Am J Sports Med 2012;40:2462-9. [Crossref] [PubMed]
- Brilakis E, Mataragas E, Deligeorgis A, et al. Midterm outcomes of arthroscopic remplissage for the management of recurrent anterior shoulder instability. Knee Surg Sports Traumatol Arthrosc 2016;24:593-600. [Crossref] [PubMed]
- Merolla G, Paladini P, Di Napoli G, et al. Outcomes of arthroscopic Hill-Sachs remplissage and anterior Bankart repair: a retrospective controlled study including ultrasound evaluation of posterior capsulotenodesis and infraspinatus strength assessment. Am J Sports Med 2015;43:407-14. [Crossref] [PubMed]
- Garcia GH, Park MJ, Zhang C, et al. Large Hill-Sachs Lesion: a Comparative Study of Patients Treated with Arthroscopic Bankart Repair with or without Remplissage. HSS J 2015;11:98-103. [Crossref] [PubMed]
- Liu JN, Garcia G, Wu HH, et al. Outcomes of The Remplissage Procedure and Its Effects on Return to Sports: Average Five-Year Follow Up. Orthop J Sports Med 2016;4: [Crossref]
- Buza JA 3rd, Iyengar JJ, Anakwenze OA, et al. Arthroscopic Hill-Sachs remplissage: a systematic review. J Bone Joint Surg Am 2014;96:549-55. [Crossref] [PubMed]
- Hartzler RU, Bui CN, Jeong WK, et al. Remplissage of an Off-track Hill-Sachs Lesion Is Necessary to Restore Biomechanical Glenohumeral Joint Stability in a Bipolar Bone Loss Model. Arthroscopy 2016;32:2466-76. [Crossref] [PubMed]
- Garcia GH, Taylor SA, Fabricant PD, et al. Shoulder Instability Management: A Survey of the American Shoulder and Elbow Surgeons. Am J Orthop (Belle Mead NJ) 2016;45:E91-7. [PubMed]
- Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 2007;89:1470-7. [Crossref] [PubMed]
- Nourissat G, Kilinc AS, Werther JR, et al. A prospective, comparative, radiological, and clinical study of the influence of the "remplissage" procedure on shoulder range of motion after stabilization by arthroscopic Bankart repair. Am J Sports Med 2011;39:2147-52. [Crossref] [PubMed]
- Leroux T, Bhatti A, Khoshbin A, et al. Combined arthroscopic Bankart repair and remplissage for recurrent shoulder instability. Arthroscopy 2013;29:1693-701. [Crossref] [PubMed]
- Rashid MS, Crichton J, Butt U, et al. Arthroscopic “Remplissage” for shoulder instability: a systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:578-84. [Crossref] [PubMed]
- Garcia GH, Park MJ, Baldwin K, et al. Comparison of arthroscopic osteochondral substitute grafting and remplissage for engaging Hill-Sachs lesions. Orthopedics 2013;36:e38-43. [Crossref] [PubMed]
- Cho NS, Yoo JH, Rhee YG. Management of an engaging Hill-Sachs lesion: arthroscopic remplissage with Bankart repair versus Latarjet procedure. Knee Surg Sports Traumatol Arthrosc 2016;24:3793-800. [Crossref] [PubMed]
- Degen RM, Giles JW, Johnson JA, et al. Remplissage versus latarjet for engaging Hill-Sachs defects without substantial glenoid bone loss: a biomechanical comparison. Clin Orthop Relat Res 2014;472:2363-71. [Crossref] [PubMed]
- Boileau P, O'Shea K, Vargas P, et al. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am 2012;94:618-26. [Crossref] [PubMed]
- Garcia GH, Wu HH, Liu JN, et al. Outcomes of the Remplissage Procedure and Its Effects on Return to Sports: Average 5-Year Follow-up. Am J Sports Med 2016;44:1124-30. [Crossref] [PubMed]
- Park MJ, Garcia G, Malhotra A, et al. The evaluation of arthroscopic remplissage by high-resolution magnetic resonance imaging. Am J Sports Med 2012;40:2331-6. [Crossref] [PubMed]
- Rhee YG, Cho NS, Yoo JH, et al. Filling Index Score of Remplissage (FISOR): a useful measurement tool to evaluate structural outcome after remplissage. J Shoulder Elbow Surg 2015;24:613-20. [Crossref] [PubMed]
- Gracitelli ME, Helito CP, Malavolta EA, et al. Results from filling “remplissage” arthroscopic technique for recurrent anterior shoulder dislocation. Rev Bras Ortop 2015;46:684-90. [Crossref] [PubMed]
- Deutsch AA, Kroll DG. Decreased range of motion following arthroscopic remplissage. Orthopedics 2008;31:492. [Crossref] [PubMed]
- Elkinson I, Giles JW, Boons HW, et al. The shoulder remplissage procedure for Hill-Sachs defects: does technique matter? J Shoulder Elbow Surg 2013;22:835-41. [Crossref] [PubMed]
- Garcia GH, Degen RM, Liu JN, et al. Accuracy of Suture Passage During Arthroscopic Remplissage-What Anatomic Landmarks Can Improve It?: A Cadaveric Study. Orthop J Sports Med 2016;4:2325967116663497 [Crossref] [PubMed]
- Garcia GH, Degen RM, Liu JN, et al. The “Safe Zone” Technique Improves Suture Placement and Accuracy During Arthroscopic Remplissage. Orthopedics 2017;40:e598-e603. [Crossref] [PubMed]
- Omi R, Hooke AW, Zhao KD, et al. The effect of the remplissage procedure on shoulder range of motion: a cadaveric study. Arthroscopy 2014;30:178-87. [Crossref] [PubMed]
Cite this article as: Idowu O, Chiu M, Miller J, Koh J, Shi L. Remplissage—when and how to fill in the defect. Ann Joint 2017;2:61.