
Rehabilitation and return to sports after anterior shoulder stabilization
Introduction
Anterior glenohumeral dislocations are a common occurrence in competitive sports and are frequently encountered in treating an athletic population. Anterior shoulder stabilization surgery has been shown to reduce subsequent instability compared to conservative intervention alone (1), and appears to be the preferred method to treat athletes who actively participate in sports (2). Rehabilitation of the athlete after anterior stabilization surgery plays an important role in the ultimate outcome of successfully returning to sports participation. Initially, rehabilitation after shoulder stabilization surgery aims to restore motion, strength, and basic function, while protecting the surgical procedure. However, as the athlete progresses, rehabilitation must prepare the shoulder for the large amount of mobility and forces required for overhead sports and/or the extreme loading that occurs with contact and collision sports, all while maintaining stability. Due to the physical and psychological demands associated with the performance of more advanced tasks, the complexity of clinical decision-making increases as the athlete progresses towards return to sports. Contributing to the difficulty of late stage rehabilitation, after anterior stabilization surgery, is a paucity of evidence and standardization to assist the clinician in determining the readiness for return to sports (3). The purpose of this article is to identify and review issues surrounding rehabilitation and return to play for athletes after an anterior shoulder stabilization. An examination of return to sports rates, recurrence of instabilities, general rehabilitation guidelines, with emphasis on late stage rehabilitation, assessment methods, and determination of readiness to return to sports will be presented. The article will look to identify methods to address the complex needs of the athlete and to provide the clinician with approaches to more objectively determine when an athlete should return to sports.
Return to sports rate
Anterior shoulder stabilization surgery typically results in good to excellent functional outcome scores (4), and return to sport rates that range from 56% (5) to 100% (6-8) (Table 1). The generally high return to sport rates suggest that surgical stabilization typically yields good results in an active population (17). However, a large amount of the information regarding return to sport rates is retrospective in nature, increasing the potential for bias, and does not quantify the level at which the athletes returns to sport. When successful return to sports is defined as achievement of preinjury levels of participation, the rate is markedly lower, ranging from 50% (12) to 80% (11) and most frequently being around 65% (5,6,9,13,18). Up to 11–22% of patients return to a lower level or change sports after the surgical stabilization (6,9,13,17). The level of post-surgery sports participation has been shown to vary depending on the sport (11) with overhead athletes requiring a longer time for rehabilitation and an overall lower return to preinjury sport status than collision athletes. These outcomes suggest that factors beyond physical limitations, such as the demands of the sport, fear of re-injury, and competing interests likely also affect the rate of return to sports (4). Given this information, recognition of and strategies to address sport specific demands and psychological factors should be considered in addition to the restoration of physical impairments following anterior stabilization (4).

Full table
Recurrence rate
Fear of re-injury and kinesiophobia have been reported to be barriers for athletes in returning to preinjury levels of sports participation (4). Review of the literature reveals that roughly 5–10% overall, and as high as 17%, of athletes experience further instability episodes following arthroscopic anterior stabilization surgery (5,8-15,17,18) (Table 1). As with return to sports rates, recurrence appears to have an association with the sport participated in, with collision sports generally resulting in higher rates (8). Given the lack of osseus congruency and inherent instability of the glenohumeral joint, some recurrence is not unexpected and emphasizes the need for proper rehabilitation to maximize the dynamic stabilizing features of the joint and utilization of useful decision-making tools to determine readiness to return to sport.
Consensus statement: global overview
The American Society of Shoulder and Elbow Therapists developed a consensus rehabilitation guideline for after arthroscopic anterior capsulolabral repair (19). Important conclusions of the review included the principle of gradual application of controlled stress to the healing repair through understanding the surgical procedure, the anatomical structures that must be protected and for how long, appropriate techniques to impart varying levels of stress, and management of the initial immobilization period and progression of range of motion (ROM) (19). The consensus guidelines provide a comprehensive review of the various phases of rehabilitation and stresses the need for sport-specific programs when working with athletes (19,20). However, the available evidence, and thus the guidelines, are less clear for the later stages of rehabilitation and determination of return to sports. The guidelines recommend that all return to sports/sport activity decisions should be made between the surgeon and patient and should not occur until specified milestones are met (19). The absence of any symptoms, appropriate ROM, strength, neuromuscular control, endurance, and power needed for the specific sport are the milestones for return to sport consideration (19). What is less apparent and where there is a lack of evidence is in the specifics of such milestones. Specifics, such as what constitutes sufficient strength, how to measure dynamic neuromuscular control and endurance, or how to assess willingness/confidence in the post-operative shoulder, remain less obvious and do not allow the clinician to make evidence based decisions regarding return to sport.
Post-operative phases of rehabilitation after anterior stabilization surgery
Phase I
Traditionally, rehabilitation and progression after anterior stabilization surgery has been heavily dependent on time frames. However, it is recommended that the clinician utilize objective criteria, in addition to time from surgery, to make decisions on entry into each phase (19). The initial rehabilitation phase is dependent on tissue healing, begins immediately after surgery, and extends through the first 6 weeks (19). Protection of the surgical repair and achievement of protected ROM is the primary goal of this phase (19). Patient education to not disrupt the surgical repair and delivery of controlled forces are integral during the first 6 post-operative weeks (19). The inflammation and repair phases for healing vascularized tissue can take up to 60 days, with full maturation of collagen taking as long as 360 days (21). The inflammatory (days 1–3) and proliferation (days 3–20) phases should incorporate minimal stress to allow the fibroblasts to synthesize a collagenous scar (21). Moderate stresses can then be applied, from days 21 onward, to promote tissue remodeling and maturation. Clinicians should apply stress via defined, protected ROM, controlled submaximal tissue loading, and dynamic stabilization (19). The proper magnitude and timing of application of the force is imperative to promote safe restoration of ROM and mobility without overstressing the capsule and repair. External rotation (ER) to 30° with the arm at the side has been shown to be safe to complete (22). If ROM exceeds the post-operative goals, then further ROM exercises should be held until the next phase. At no point, should ROM be forceful or proceed beyond the available limits of motion, ceasing at the ranges contraindicated after surgery, limiting the stretch that occurs (19). Supplemental activities include scapular exercises, active ROM of uninvolved joints of the upper extremity, and submaximal isometrics with the arm adducted to the side in neutral rotation (19). With all activities, the clinician needs to stay mindful and fully educate the patient that the first priority of this phase is protection of the surgical site and healing of the involved tissues.
Phase II
When a patient has reached weeks 6 through 12, they are considered to be in the second phase of rehabilitation following surgical stabilization of the shoulder. This phase emphasizes a gradual increase in ROM, submaximal tissue loading, and dynamic stabilization. The goal by the end of the 12th week is to have full ROM, with the exception of end-range ER at 90° abduction (19), which patients are educated to avoid as well as heavy lifting, and strengthening in provocative positions. Rehabilitation will continue with a staged approach to gaining ROM and rotator cuff and scapular strengthening/control exercises to promote dynamic stability will be initiated (19). Steady increases in the muscular demand required to perform strengthening and neuromuscular control activities is required and can be judged by quality of the movement and the presence or absence of symptoms. Performance of such activities should occur throughout the available ROM and include exercises to address strength and endurance limitations. Gentle manual therapy techniques may be utilized to address capsular and extracapsular restrictions at the glenohumeral and scapulothoracic joints as well as therapeutic exercises for strengthening of the periscapular musculature and rotator cuff. Any flexibility deficits, such as pectoralis minor, or posterior capsular restrictions should be addressed. Strengthening exercises may be gradually progressed to overhead positions, should include isolated and complex movement patterns, and be progressed via resistance and/or speed. Emphasis is placed on neuromuscular control and maintaining centralization of the humeral head on the glenoid. Progression should occur only if the patient is maintaining adequate form without compensation and in the absence of symptoms.
Phase III
The third phase of rehabilitation after anterior shoulder stabilization generally occurs between weeks 12 and 24 post-operatively. During this phase, the primary focus of rehabilitation is on normalizing strength and neuromuscular control, developing power required for higher level activities, and achieving dynamic stability of the glenohumeral joint (19). As with the previous two phases, the application of stress to the capsulolabral structures must be gradual and consistent surveillance of the patient’s tolerance is required. However, a clear, evidence based time-frame for the initiation of higher level activities after surgical stabilization has yet to be established (16). Allowing at least 12 weeks to pass from surgery appears to be the minimum requirement (21), but more specific guidance does not currently exist. An individualized approach needs to be taken to achieve the goal of this phase of rehabilitation, which is the full and complete return to the patient’s desired activities (19). Due to the specificity of demands placed on the shoulder during different sports, a sport specific approach is required to ready the athlete to return to competition (20). For example, overhead athletes will need to achieve functional amounts of ER in 90° abduction, a recommended strength ratio of external to internal rotation (IR) of at least 65% (23), and muscular endurance for the repetitive nature of throwing. Collision athletes will need to achieve strength, power, and stability to sustain impact loading of the glenohumeral joint. Highly specific rehabilitation plans will address these needs through exercise selection, rate and intensity of application, and ultimately place them in the context of the sport. Typically, athletes can expect to return to competition approximately 4–6 months after surgery (5,6,11,14,15,17), though contact and overhead sports may require more time (9,12).
Return to play criteria
As stated in the consensus guidelines presented by the American Society of Shoulder and Elbow Therapists (19), return to sporting activity should not occur until specific milestones are achieved. Gaunt et al. (19) recommended that the athlete should be free of symptoms, have appropriate ROM, strength, neuromuscular control, endurance, and power, and be cleared by the surgeon for return to sports. Pavlik et al. (9) permitted athletes to return to full sports participation after they achieved nearly full ROM, side-equivalent muscle power, and a negative apprehension sign. Alentorn-Geli et al. (18) cleared professional soccer players to return to sports when they achieved complete, painfree ROM and at least 80% strength of the contralateral side. Additional studies have utilized symmetry with abduction and ER strength (12), rotator cuff strength with 90% limb symmetry and equal proprioception bilaterally (7), and normal, pain-free ROM with symmetrical strength and function (17). However, far more studies do not state explicit criteria for determining readiness to return sport, instead reporting that the decision was time-based (5,6,10,11,13-15). Criteria utilized to return to sports in various studies is presented in Table 1.
As mentioned earlier, utilizing such criteria to determine readiness to return to sports has worked fairly well as evidenced by the rates of returning to pre-injury levels of participation (5,6,9,13,18) and the generally low recurrence rate (5,8-15,17,18). However, we believe that further refinement of return to play criteria is needed. Establishing valid, reliable, and evidence-based tests and measures that are sport/task specific to utilize as screening mechanisms may potentially enhance the return to preinjury level rates and further decrease the recurrence rates. Specific assessment methods will be summarized below. Return to play criteria should be specific for the type of sports played as well as the demands that will be placed upon the shoulder. Future research also should focus on determining the percentage of those returning to preinjury levels, without recurrence, when more detailed return to play criteria are applied.
Assessment methods
Much of the difficulty that surrounds rehabilitation and return to play after anterior stabilization is in determining readiness to advance through the phases of recovery and in determining when to allow return to sports participation. Various assessment methods have been developed and tested. A review of methods to assess ROM, strength, and function is provided and may be incorporated into determining readiness to return to sports participation.
ROM
ROM following an anterior instability stabilization procedure is an emphasis of treatment from the first postoperative session until it is restored to meet the needs of the patient. In communication with the surgeon, the physical therapist will ensure gradual, weekly increase in ROM taking care to ensure not to exceed any postoperative restrictions while also avoiding adhesive capsulitis. At the completion of the rehabilitation process, the expectation is for the patient to have symmetric ROM as well as what is required for their daily and physical activities. In the case of the overhead athlete, their sport may require increased ER at 90° elevation. The excessive ER can lead to decreased IR and an assessment of total arc of motion, ER and IR at 90° elevation, is required to determine if the athlete has a pathologic glenohumeral IR deficit (GIRD) (24). A decrease in IR up to 20° can be normal in overhead athletes if their total arc of motion is symmetric bilaterally. If the athlete presents with up to a 20° IR deficit and with greater than a 5° loss of total ROM, they are considered to have pathologic GIRD and are at risk for shoulder injury and disability (24). Education to the patient emphasizes the need to not exceed ROM limits early post-operatively, to achieve the amount of motion required for their sport during the later stages of rehabilitation, and to maintain ROM after the completion of the rehabilitation process.
Strength
Restoring dynamic stability is one of the main rehabilitation goals for this patient population. The rehabilitation specialist will need to assess the rotational strength of the involved to uninvolved extremities as well as assess the involved ER to IR (ER/IR) strength ratio. A ratio of 66% ER to IR strength was found to be normal in subjects (25) and therefore should be the goal of rehabilitation. A 10% increase in the ER/IR ratio has been recommended in individuals with anterior glenohumeral instability to produce a posterior-dominant shoulder for dynamic stabilization (26) and therefore an ER/IR ratio goal of 65–75% may be more appropriate.
Methods to assess upper extremity strength can include manual resistance applied in an against-gravity position, measurement of isometric force/torque with a hand-held dynamometer or isokinetic dynamometry (Table 2). While it is easy to complete in a clinical setting, the disadvantage to relying on manual muscle testing in the upper extremity is a lack of objective data and the possibility of overestimating limb symmetry. Ellenbecker (27) compared individuals with symmetric manual muscle testing to isokinetic testing and found up to 15% and 28% differences in ER and IR, respectively.
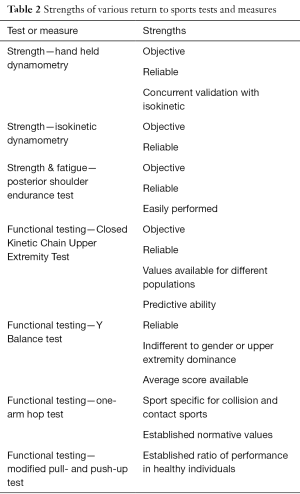
Full table
Hand held dynamometry (HHD) provides an objective, reliable measure for isometric strength testing. Use of HHD has been shown to have excellent reliability for assessing rotational shoulder strength in multiple positions (28). The use of HHD for strength assessments has revealed no significant differences between dominant and non-dominant limbs for ER at varying angles of abduction (29). However, side to side differences in IR do exist, with the dominant limb exhibiting greater strength than the nondominant limb (29). Using HHD to measure strength of the shoulder rotators has been shown to correlate well with the results of isokinetic testing (30). Additionally, HHD does exhibit reliability and concurrent validity with high correlations to isokinetic testing (31). Given these results, when assessing readiness to return an athlete to sports, the clinician can expect the results obtained from HHD can be similar to formal isokinetic testing.
Isokinetic dynamometry allows an assessment of ER/IR strength while controlling for position, ROM, speed, rotational forces and translational stresses (27). It provides an objective value for the agonist-antagonist ratio and has good reliability in assessing the ER/IR peak torque (32). It is important to assess as individuals with glenohumeral joint instability have demonstrated alterations in their ER/IR ratio (33), decreased rotational strength in those with anterior instability (34), and deficits in rotational strength that can remain up to 16 months after arthroscopic labral repair (35). As stated above, the goal is to achieve an ER/IR ratio of 65–75% however, there are also sport specific values in the literature. Their results provide insight into specific athletic populations, that include but are not limited to, tennis (36), baseball (37), swimmers (38), volleyball (39), and climbers (40).
An athlete’s rate of fatigue is an important return to sports consideration. Therefore, a method of fatigue testing is valuable to the clinician in later stages of rehabilitation. A variety of tests have been described to determine relative fatigue of the shoulder girdle. The Posterior Shoulder Endurance Test (PSET) (41) utilizes 2% of the performer’s body weight as resistance while prone horizontal abduction is performed at a cadence of 30 beats per minute. The test is reported to have excellent test-retest reliability [intraclass correlation coefficient (ICC) =0.85], though this test has been described in a healthy cohort only (41). Similarly, another study (42) described fatigue testing with scaption, prone horizontal abduction at 100° and standing cable press with 5%, 3%, and 30% body weight, respectively. Prone horizontal abduction at 100° was then found to be correlated to sustaining a shoulder injury in a cohort of football players (42).
Functional testing
Patient readiness to return to sport determined by objective measures of strength and ROM may not capture the patient’s ability to move effectively, efficiently and confidently. Literature has suggested several functional tests, specific to the shoulder that can be utilized to determine readiness to return to sport or discern when more rehabilitation is required (Table 2). Functional tests should be representative of the sport the athlete is returning to, with consideration for movement replication and energy system used (anaerobic vs aerobic).
The Closed Kinetic Chain Upper Extremity Stability (CKCUES) (43,44) test can assess an athlete’s confidence in the shoulder as well as relate to participation in contact sports. The athlete is in a push-up, or modified push-up position for females, and instructed to move one hand from the floor to the contralateral hand, that is 36 inches apart, and then back to its starting position. This motion is repeated for 15 seconds, testing the ability of the athlete to rapidly move their hand back and forth and their confidence in a three-point stance. Performance of the test is repeated 3 times with 45-second breaks and the scores are averaged. Test-retest reliability demonstrates excellent reliability (ICC =0.92) (44). The CKCUES test appears in the literature more frequently than other tests and has been described specifically in baseball (45), football (42), and in those with subacromial impingement (43). Reference values have been established for males (18.5) and females (20.5) (43) and in baseball players (45), and scores have found to be higher in active individuals over sedentary individuals and those with impingement syndrome (43).
Additionally, the CKCUES test has been shown to provide insight on injury prediction in collegiate football players, where those who scored less than 21 touches were 18 times more likely to sustain a shoulder injury (42).
The unilateral seated shot put test has also been suggested as a test to determine readiness for return to sport (46). The athlete is instructed to push a 6-pound medicine ball as far forward as they can while either long sitting in a chair or with their knees bent to 90° while seated on the floor (46). The patient should have their back against a chair or doorway, to allow for unrestricted glenohumeral extension as part of the test. Generally, three trials are performed with a rest period between trials ranging from 30 seconds to 2 minutes (46,47). Bilateral comparison in a healthy population of men and women demonstrated a 9% deficit in the nondominant shoulder vs. the dominant shoulder (47). A minimal detectable change of 17 (nondominant) and 18 (dominant) inches exists (47). This provides an objective goal when testing for return to sport.
The Y balance test incorporates both core strength and endurance and has been found to be reliable and indifferent to gender or upper extremity dominance (48). To perform, the athlete assumes a push-up position, keeping the involved extremity in contact with the floor as the athlete maximally reaches medially, inferolaterally and superolaterally with the contralateral extremity. The subject is given three trials for each direction. The distance achieved during the three trials for each direction is then averaged. This average is then divided by the subject’s upper limb length. The average composite reach score has been shown to be 84.5% of upper limb length (48).
The one-arm hop test was developed in efforts to make functional testing more sport specific to wrestling and football (49). The athlete is required to assume a one-arm push-up position on the floor, hop onto a 10.2-cm step and then back to the floor for five repetitions for time. After 1 minute, the contralateral side is tested. The dominant upper extremity has been shown to complete the test 4.4% faster than the nondominant upper extremity, and the test has established normative values for wrestlers and football players (49).
The modified pull up test has been described as a method of functional strength assessment (47). The athlete performs an inverted row with use of a Smith machine with a Smith Press bar positioned just beyond arm’s reach when supine. Support of the legs is either provided at the heel for men, or lower leg just below the knees for women. Patients are instructed to pull up so that the proximal arm would be parallel to the ground and then lower until elbows were fully extended. Patients are instructed to complete as many repetitions as possible within 15 seconds. Three trials are performed with a 45-second rest break. In conjunction with the modified pull up test, patient’s may be assessed with a modified push up test as well (47,50). Here, patients perform a push up in standard (males) or modified (female) position and are instructed to complete as many repetitions as possible within 15 seconds. Three trials are performed with a 45-second rest between tests (47). In healthy, recreationally active individuals, the muscles responsible for the modified push up test are 1.5–2.5 times stronger than those responsible for the modified pull up test (47).
A review of the literature (50) in regards to 6 upper extremity performance tests revealed the CKCUES test and the seated shot put had moderate evidence for reliability and construct validity for their use in functional performance testing. The review (50) highlighted the lack of quality research on the topic as gauged by sample size, reliability, and construct validity.
Our recommended return to sports criteria
Given the multitude of strength assessments and functional performance tests that exist regarding shoulder function and the paucity of evidence on their validity and overall value, a battery of tests is recommended to cover all aspects of sport specificity, confidence, strength, ROM, and endurance in efforts to appropriately assess the athlete’s ability to return to sport.
Conclusions
Rehabilitation after surgical anterior stabilization of the glenohumeral joint is a multi-phase process. The clinician must adhere to tissue specific contraindications in the early weeks after stabilization. Restoration of shoulder ROM, rotator cuff and scapular strength and joint proprioception and stability is paramount before turning the focus to optimization of function in preparation for returning to sports. An understanding of the demands of the sport is essential to appropriately match the rehabilitation protocol and assessment methods to ensure readiness for retuning to sports and increase the likelihood of the athlete retuning to preinjury levels of participation. A battery of tests is recommended to fully assess the athlete’s readiness to return to sport in effort to reduce the recurrence rate and increase the likelihood of a successful return to sports.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Albert Lin and Jason J. Shin) for the series “Trends in Anterior Shoulder Instability” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interests: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.10.06). The series “Trends in Anterior Shoulder Instability” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Handoll HH, Almaiyah MA, Rangan A. Surgical versus non-surgical treatment for acute anterior shoulder dislocation. Cochrane Database Syst Rev 2004;CD004325 [PubMed]
- Balke M, Shafizadeh S, Bouillon B, et al. Management of shoulder instability: the current state of treatment among German orthopaedic surgeons. Arch Orthop Trauma Surg 2016;136:1717-21. [Crossref] [PubMed]
- Creighton DW, Shrier I, Shultz R, et al. Return-to-play in sport: a decision-based model. Clin J Sport Med 2010;20:379-85. [Crossref] [PubMed]
- Tjong VK, Devitt BM, Murnaghan ML, et al. A Qualitative Investigation of Return to Sport After Arthroscopic Bankart Repair: Beyond Stability. Am J Sports Med 2015;43:2005-11. [Crossref] [PubMed]
- Boileau P, Fourati E, Bicknell R. Neer modification of open Bankart procedure: what are the rates of recurrent instability, functional outcome, and arthritis? Clin Orthop Relat Res 2012;470:2554-60. [Crossref] [PubMed]
- Beranger JS, Klouche S, Bauer T, et al. Anterior shoulder stabilization by Bristow-Latarjet procedure in athletes: return-to-sport and functional outcomes at minimum 2-year follow-up. Eur J Orthop Surg Traumatol 2016;26:277-82. [Crossref] [PubMed]
- Hart D, Funk L. Serious shoulder injuries in professional soccer: return to participation after surgery. Knee Surg Sports Traumatol Arthrosc 2015;23:2123-9. [Crossref] [PubMed]
- Mazzocca AD, Brown FM Jr, Carreira DS, et al. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med 2005;33:52-60. [Crossref] [PubMed]
- Pavlik A, Csépai D, Hidas P, et al. Sports ability after Bankart procedure in professional athletes. Knee Surg Sports Traumatol Arthrosc 1996;4:116-20. [Crossref] [PubMed]
- Mishra DK, Fanton GS. Two-year outcome of arthroscopic bankart repair and electrothermal-assisted capsulorrhaphy for recurrent traumatic anterior shoulder instability. Arthroscopy 2001;17:844-9. [Crossref] [PubMed]
- Ide J, Maeda S, Takagi K. Arthroscopic Bankart repair using suture anchors in athletes: patient selection and postoperative sports activity. Am J Sports Med 2004;32:1899-905. [Crossref] [PubMed]
- Garofalo R, Mocci A, Moretti B, et al. Arthroscopic treatment of anterior shoulder instability using knotless suture anchors. Arthroscopy 2005;21:1283-9. [Crossref] [PubMed]
- Hayashida K, Yoneda M, Mizuno N, et al. Arthroscopic Bankart repair with knotless suture anchor for traumatic anterior shoulder instability: results of short-term follow-up. Arthroscopy 2006;22:620-6. [Crossref] [PubMed]
- Castagna A, Markopoulos N, Conti M, et al. Arthroscopic bankart suture-anchor repair: radiological and clinical outcome at minimum 10 years of follow-up. Am J Sports Med 2010;38:2012-6. [Crossref] [PubMed]
- Ee GW, Mohamed S, Tan AH. Long term results of arthroscopic Bankart repair for traumatic anterior shoulder instability. J Orthop Surg Res 2011;6:28. [Crossref] [PubMed]
- Boileau P, Villalba M, Héry JY, et al. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 2006;88:1755-63. [PubMed]
- Ozturk BY, Maak TG, Fabricant P, et al. Return to sports after arthroscopic anterior stabilization in patients aged younger than 25 years. Arthroscopy 2013;29:1922-31. [Crossref] [PubMed]
- Alentorn-Geli E, Álvarez-Díaz P, Doblas J, et al. Return to sports after arthroscopic capsulolabral repair using knotless suture anchors for anterior shoulder instability in soccer players: minimum 5-year follow-up study. Knee Surg Sports Traumatol Arthrosc 2016;24:440-6. [Crossref] [PubMed]
- Gaunt BW, Shaffer MA, Sauers EL, et al. The American Society of Shoulder and Elbow Therapists' consensus rehabilitation guideline for arthroscopic anterior capsulolabral repair of the shoulder. J Orthop Sports Phys Ther 2010;40:155-68. [Crossref] [PubMed]
- Reinold MM, Wilk KE, Reed J, et al. Interval sport programs: guidelines for baseball, tennis, and golf. J Orthop Sports Phys Ther 2002;32:293-8. [Crossref] [PubMed]
- Blackburn TA, Guido JA. Rehabilitation after ligamentous and labral surgery of the shoulder: guiding concepts. J Athl Train 2000;35:373-81. [PubMed]
- Itoi E, Hatakeyama Y, Urayama M, et al. Position of immobilization after dislocation of the shoulder. A cadaveric study. J Bone Joint Surg Am 1999;81:385-90. [Crossref] [PubMed]
- Ellenbecker TS, Mattalino AJ. Concentric isokinetic shoulder internal and external rotation strength in professional baseball pitchers. J Orthop Sports Phys Ther 1997;25:323-8. [Crossref] [PubMed]
- Manske R, Wilk KE, Davies G, et al. Glenohumeral motion deficits: friend or foe? Int J Sports Phys Ther 2013;8:537-53. [PubMed]
- Ivey FM Jr, Calhoun JH, Rusche K, et al. Isokinetic testing of shoulder strength: normal values. Arch Phys Med Rehabil 1985;66:384-6. [PubMed]
- Ellenbecker TS, Davies GJ. The application of isokinetics in testing and rehabilitation of the shoulder complex. J Athl Train 2000;35:338-50. [PubMed]
- Ellenbecker TS. Muscular strength relationship between normal grade manual muscle testing and isokinetic measurement of the shoulder internal and external rotators. Isokinet Exerc Sci 1996;6:51-6.
- Cools AM, De Wilde L, Van Tongel A, et al. Measuring shoulder external and internal rotation strength and range of motion: comprehensive intra-rater and inter-rater reliability study of several testing protocols. J Shoulder Elbow Surg 2014;23:1454-61. [Crossref] [PubMed]
- Riemann BL, Davies GJ, Ludwig L, et al. Hand-held dynamometer testing of the internal and external rotator musculature based on selected positions to establish normative data and unilateral ratios. J Shoulder Elbow Surg 2010;19:1175-83. [Crossref] [PubMed]
- Ellenbecker TS, Bleacher J. A descriptive profile of bilateral glenohumeral joint internal and external rotation strength in uninjured females using the cybex NORM dynamometer. Phys Ther 1999;79:S80.
- Holt KL, Raper DP, Boettcher CE, et al. Hand-held dynamometry strength measures for internal and external rotation demonstrate superior reliability, lower minimal detectable change and higher correlation to isokinetic dynamometry than externally-fixed dynamometry of the shoulder. Phys Ther Sport 2016;21:75-81. [Crossref] [PubMed]
- Edouard P, Codine P, Samozino P, et al. Reliability of shoulder rotators isokinetic strength imbalance measured using the Biodex dynamometer. J Sci Med Sport 2013;16:162-5. [Crossref] [PubMed]
- Warner JJ, Micheli LJ, Arslanian LE, et al. Patterns of flexibility, laxity, and strength in normal shoulders and shoulders with instability and impingement. Am J Sports Med 1990;18:366-75. [Crossref] [PubMed]
- Saccol MF, Zanca GG, Ejnisman B, et al. Shoulder rotator strength and torque steadiness in athletes with anterior shoulder instability or SLAP lesion. J Sci Med Sport 2014;17:463-8. [Crossref] [PubMed]
- Szuba Ł, Markowska I, Czamara A, et al. Quantitative analysis of peak torque and power-velocity characteristics of shoulder rotator muscles after arthroscopic labral repair. J Sci Med Sport 2016;19:805-9. [Crossref] [PubMed]
- Niederbracht Y, Shim AL. Concentric internal and eccentric external fatigue resistanc of the shoulder rotator muscles in female tennis players. N Am J Sports Phys Ther 2008;3:89-94. [PubMed]
- Lee J, Kim LN, Song H, et al. The effect of glenohumeral internal rotation deficit on the isokinetic strength, pain, and quality of life in male high school baseball players. Ann Rehabil Med 2015;39:183-90. [Crossref] [PubMed]
- Batalha NM, Raimundo AM, Tomas-Carus P, et al. Shoulder rotator cuff balance, strength, and endurance in young swimmers during a competitive season. J Strength Cond Res 2013;27:2562-8. [Crossref] [PubMed]
- Stickley CD, Hetzler RK, Freemyer BG, et al. Isokinetic peak torque ratios and shoulder injury history in adolescent female volleyball athletes. J Athl Train 2008;43:571-7. [Crossref] [PubMed]
- Wong EK, Ng GY. Strength profiles of shoulder rotators in healthy sport climbers and nonclimbers. J Athl Train 2009;44:527-30. [Crossref] [PubMed]
- Moore SD, Uhl TL, Kibler WB. Improvements in shoulder endurance following a baseball-specific strengthening program in high school baseball players. Sports Health 2013;5:233-8. [Crossref] [PubMed]
- Pontillo M, Spinelli BA, Sennett BJ. Prediction of in-season shoulder injury from preseason testing in division I collegiate football players. Sports Health 2014;6:497-503. [Crossref] [PubMed]
- Tucci HT, Martins J, Sposito Gde C, et al. Closed Kinetic Chain Upper Extremity Stability test (CKCUES test): a reliability study in persons with and without shoulder impingement syndrome. BMC Musculoskelet Disord 2014;15:1. [Crossref] [PubMed]
- Goldbeck TG, Davies GJ. Test-retest reliability of the closed kinetic chain upper extremity stability test: a clinical field test. J Sport Rehabil 2000;9:35-45. [Crossref]
- Roush JR, Kitamura J, Waits MC. Reference Values for the Closed Kinetic Chain Upper Extremity Stability Test (CKCUEST) for Collegiate Baseball Players. N Am J Sports Phys Ther 2007;2:159-63. [PubMed]
- Chmielewski TL, Martin C, Lentz TA, et al. Normalization considerations for using the unilateral seated shot put test in rehabilitation. J Orthop Sports Phys Ther 2014;44:518-24. [Crossref] [PubMed]
- Negrete RJ, Hanney WJ, Kolber MJ, et al. Reliability, minimal detectable change, and normative values for tests of upper extremity function and power. J Strength Cond Res 2010;24:3318-25. [Crossref] [PubMed]
- Gorman PP, Butler RJ, Plisky PJ, et al. Upper Quarter Y Balance Test: reliability and performance comparison between genders in active adults. J Strength Cond Res 2012;26:3043-8. [Crossref] [PubMed]
- Falsone SA, Gross MT, Guskiewicz KM, et al. One-arm hop test: reliability and effects of arm dominance. J Orthop Sports Phys Ther 2002;32:98-103. [Crossref] [PubMed]
- Tarara DT, Fogaca LK, Taylor JB, et al. Clinician-friendly physical performance tests in athletes part 3: a systematic review of measurement properties and correlations to injury for tests in the upper extremity. Br J Sports Med 2016;50:545-51. [Crossref] [PubMed]
Cite this article as: Popchak A, Patterson-Lynch B, Christain H, Irrgang JJ. Rehabilitation and return to sports after anterior shoulder stabilization. Ann Joint 2017;2:62.


