
Arthroscopic soft tissue stabilization: single anterior portal technique
Introduction
Open Bankart repair has long been considered the gold standard in treatment of anterior shoulder instability; however, over the past decade, arthroscopic stabilization for anterior instability has gained popularity and is now the favoured technique in many centers. The objectives of an arthroscopic repair mirror those of open methods: the anatomy of the anterior capsulolabral complex is restored and the inferior glenohumeral ligament is re-tensioned. The rise in popularity of arthroscopic management is secondary to advancements in surgical equipment and technique as well as an improved understanding of the underlying pathoanatomy responsible for shoulder instability. The advent of suture anchors over earlier techniques such as transglenoid sutures has resulted in marked improvements in the success of arthroscopic management and allows for multiple points of fixation (1-5). These advancements, along with appropriate patient selection, have yielded similar outcomes between open and arthroscopic methods, with some authors claiming that appropriately addressing underlying pathology as opposed to the surgical approach itself is more important to outcomes (6).
Several soft tissue lesions are associated with anterior glenohumeral instability. The classic lesion, termed Bankart lesion, is a detachment of the anterior inferior portion of the labrum (2,7). This is thought to be the “essential lesion” in anterior shoulder instability and is typically associated with some degree of capsular stretch (2,7,8). Other associated lesions include an anterior labroligamentous periosteal sleeve avulsion (ALPSA) lesion which is characterized by the avulsed labrum healing in a medialized position along the glenoid neck, a humeral avulsion of the glenohumeral ligament (HAGL) lesion where detachment of the glenohumeral ligament occurs off the humerus, and a Hill-Sachs lesion which is an impaction fracture of the posterior humeral articular surface (1,2,7). Further, glenoid bone loss may also accompany anterior instability. This can occur as an acute fracture or, more commonly, secondary to erosion from repeated instability episodes (1). While some of these associated lesions can be addressed arthroscopically if appropriately recognized, bony defects often warrant open approaches. Failing to recognize certain pathoanatomic variables and patient factors will adversely affect results of arthroscopic techniques. Several authors have shown that the most common reason for failure following arthroscopic Bankart repair is significant glenoid bone loss (2,6,9). Generally, glenoid bone loss greater than 20% of the glenoid surface warrants an open procedure (1,2,6). More recent biomechanical and clinical studies out of Korea have shown that perhaps 15-16% bone loss may be a more accurate clinical threshold for failure (10,11). Further, patients with engaging Hill-Sachs lesions are more likely to fail arthroscopic Bankart repair alone (1,8,12). Identification of this lesion requires a dynamic evaluation prior to performing a Bankart repair (1). Appropriate recognition of bony lesions precluding arthroscopic soft tissue repair is essential to patient selection.
Several authors have sited the advantages of arthroscopic stabilization over open procedures (1,6,13). The advantages and disadvantages of arthroscopic Bankart repair are summarized in Table 1. Arthroscopic procedures are less invasive when compared to their open counterpart, resulting in decreased post-operative pain as well as improved cosmesis (1,13,14). Arthroscopic techniques allow for direct intra-articular visualization from various angles with less soft tissue dissection, facilitating the identification of associated lesions as well as a dynamic assessment of the Hill-Sachs lesion (1). Further, appropriate re-tensioning of the inferior glenohumeral ligament can be directly visualized (1). Despite these advantages, no functional advantage to arthroscopic stabilization over open repair has been identified (4). Careful patient section and appropriate management of underlying pathology has resulted in arthroscopic techniques yielding similar functional outcomes compared to open techniques. Consequently, many surgeons now consider arthroscopic techniques the new gold standard for Bankart repair (1).
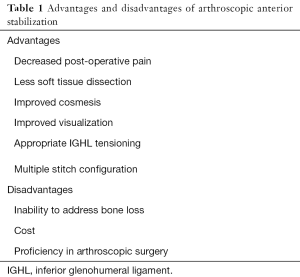
Full table
Patient selection and workup
Key features on history and physical examination are useful in understanding the type of instability a patient is experiencing and may ultimately help determine if an arthroscopic stabilization procedure is an appropriate option. The most important features to obtain in a thorough history are: (I) the direction of instability (anterior or posterior); (II) the degree of dislocation (subluxation or dislocation); (III) the immediate treatment (self-reduction or assisted reduction); (IV) the predominant symptoms (looseness, apprehension, or pain); (V) age of onset; (VI) number of recurrent dislocations; and (VII) activity level (2,6). It is useful to understand the degree of trauma required to elicit an instability event as well as the arm position when this occurs. Dislocations that occur in the absence of trauma should be evaluated for a volitional component (2). Cases of recurrent dislocation that occur with increasing ease should raise concerns for bone loss (1,2). A complete examination of the shoulder should be obtained in all patients. It is important to assess the neurologic status of the extremity as well as range of motion, scapular motion, and rotator cuff strength which, if abnormal, indicate associated injuries (1,2). Examination findings specific to anterior shoulder instability include the apprehension test, relocation test, and anterior release test (15). Further, patients should be evaluated for generalized laxity with tools such as the Beighton score and tests such as the sulcus sign (2,6).
Standard radiographs should include a true glenohumeral anteroposterior view, axillary lateral view, and a scapular-Y view. Further radiographs may be useful in diagnosing associated bony lesions. The West point view is useful in identifying glenoid bone loss and glenoid rim fractures (2). The Stryker Notch view and anteroposterior view in internal rotation are most useful in identifying Hill-Sachs lesions (2). Bony lesions are best evaluated with a CT scan with 3D reconstruction and humeral head digital subtraction (2). This allows for an accurate assessment of the surface area of bone loss using the best-fit circle method described by Huysmans and colleagues (2,16). Magnetic resonance arthrography (MRA) is the gold standard for evaluating soft tissue lesions prior to arthroscopic evaluation and management (1).
Information gleaned from the history, physical examination, and imaging are useful in determining the success of arthroscopic stabilization. Indications and contraindications for arthroscopic management are summarized in Table 2. As previously discussed, significant bone loss on either the glenoid or humeral side represent contraindications to successful arthroscopic management (1,2,6,17-21). Balg and Boileau used key features from history, physical examination, and imaging to estimate the success of arthroscopic repair in a 10-point Injury Severity Index Score (ISIS) (9). This takes into account age, level of sport, type of sport, laxity, Hill-Sachs lesions, and glenoid bone loss (22). Patients with scores of 3 or less were found to have low (5%) rates of recurrence following arthroscopic Bankart repair and those with scores greater than 6 were found to have high (70%) rates of recurrence (1,22,23).
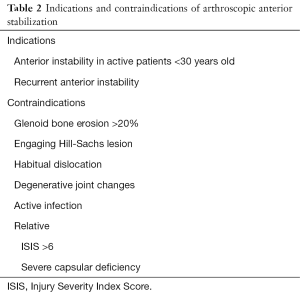
Full table
Surgical technique
Patient positioning
With the patient in the supine position, general anaesthesia is administered. After securing the airway, both shoulders are assessed for range of motion, laxity and instability. The patient is then placed in the lateral decubitus position with the operative shoulder positioned superiorly. Tilting the beanbag back slightly keeps the glenoid face parallel to the floor. All bony prominences are padded and an axillary roll is positioned. Ten pounds of traction is applied to the shoulder and it is placed in 40° of abduction and 20° of forward flexion. While either the lateral decubitus position or the modified beach chair position may be used and is a matter of surgeon preference, the authors prefer the lateral decubitus position as it provides improved access to the axillary pouch and posterior recess. Further, it allows for traction to be applied to the shoulder improving visualization (20). Once the patient is appropriately positioned, the arm is sterilely prepped and draped and a surgical pause is carried out.
Portal placement and diagnostic arthroscopy
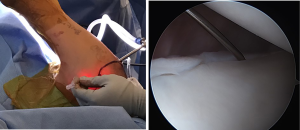
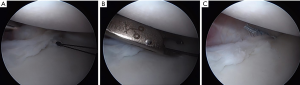
The posterior viewing portal is established first. This is placed in the “soft spot” just lateral to the glenoid and 1cm inferior to the posterior edge of the acromion (20,24). This portal should be placed so that the camera angle replicates the angle of the glenoid face. A drive-through sign, which is the ability to sweep the arthroscope easily from the superior aspect of the glenohumeral joint to the inferior aspect of the glenohumeral joint and into the axillary pouch, may be noted (20,21,25). This sign is indicative of capsular laxity and injury (25). To establish the anterior working portal, a spinal needle is used for localization. The needle is inserted through the rotator interval and is navigated through the joint to ensure that the instruments used for suture shuttling as well as anchor placement can reach the zone of pathology, most importantly the anterior inferior labrum (Figure 1). The ideal angle of approach to the anterior glenoid is 45 degrees particularly for suture anchor drilling (21). Typically, this portal is just superior to the subscapularis tendon and off the anterior corner of the acromion (24). Once the satisfactory position has been selected, the anterior portal is established in line with the spinal needle using an outside-in technique (24).
Traditionally, several authors utilize three standard portals when performing anterior labral repairs (2,20). In addition to the two aforementioned portals, an anterior midglenoid portal can be established (2). Recent literature suggests that use of a single anterior portal yields the same outcomes and avoids portal crowding anteriorly (24). The use of a single anterior portal is our preferred technique. In cases where a single anterior postal is insufficient to place the most inferior suture anchor, this anchor may be placed through a separate stab incision without the use of a cannula (21).
A thorough diagnostic evaluation of the glenohumeral joint is then performed. The labrum is visualized from both the anterior as well as the posterior portal and 70° arthroscope is used as necessary, which allows for identification of a possible ALPSA lesion (2,20,21). The biceps tendon and superior labrum are probed to look for concomitant tears. The rotator cuff is then assessed including the subscapularis, which can be torn in settings of anterior instability. It is important to look for a HAGL lesion, which can occur with or without an associated anterior labral lesion (20,21,26). If present, capsular splits may be repaired in a side-to-side manner (20). When avulsed off the humerus, it is difficult to achieve the correct angle of approach for repair through the anterior portal (20). A second anterior portal or open approach may be required to adequately repair the lesion. Failure to address a HAGL lesion when present results in a significantly higher rate of recurrence following repair (1,2,20,21,26).
A thorough evaluation for articular surface lesions is then carried out. While pre-operative CT imaging is used to estimate glenoid bone loss, this should be reassessed and confirmed at the time of arthroscopy. Following glenoid assessment, the humeral head should be assessed for a bipolar Hill-Sachs lesion. Hill-Sachs lesions are commonly present in anterior instability; however, the majority are not significant (2,8). A Hill-Sachs lesion is best viewed from the standard posterior portal (21). A dynamic assessment is then carried out to determine if the lesion is engaging. A lesion is considered to be engaging if the lesion engages the anterior glenoid rim when the arm is brought into a position of abduction and external rotation (2,8,12). Lesions are more likely to engage if glenoid bone loss is concomitantly present (2,21). Significant Hill-Sachs lesions are those that are engaging or “off-track” lesions, and when present should not be managed with arthroscopic anterior labral repair alone (2,20,21,27). In these instances, a remplissage augmentation should be considered (12,20,21).
Preparing the glenoid
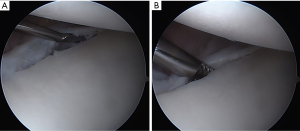
Using an arthroscopic elevator, the labrum and ligamentous complex are thoroughly elevated off the glenoid neck as a single unit (Figure 2A). A grasper is used to assess the mobility of the tissue. The release is adequate once the muscle fibers of the subscapularis are visible and the labrum “floats up” to the level of the glenoid rim (2,20). There is typically a capsular stretch injury with inferior capsular redundancy, requiring the capsulolabral complex to be shifted in an inferior-to-superior direction in order to re-establish physiologic tension (2,20). In cases of patients with ligamentous laxity, a more than physiologic shift may be opted to address concerns of capsular redundancy. The glenoid rim is then gently decorticated using a combination of a burr, shaver or a rasp (Figure 2B). The goal is to create a bleeding bone bed for healing without causing iatrogenic glenoid bone loss (2,20). A small curette may be used to remove 1–2 mm strip of articular cartilage from the anterior glenoid rim to prevent the capsule from healing in a medialized position following repair (20,21).
Anterior capsulolabral repair
The inferior most anchor is placed first. Through the anterior portal, a drill hole is placed on the inferior glenoid at a position 2 mm onto the articular face. This is typically at the 5:00 o’clock or 5:30 o’clock position and placing this first anchor inferior enough to appropriately address the pathology present is critical to the outcome of the repair (28). A suture anchor (Bio-SutureTak, Arthrex; Naples, FL) is impacted into position using a mallet at angle 45 degrees to the glenoid face (2,20). Using the same anterior portal with the sutures from the anchors parked at the side, a tissue penetrator preloaded with a monofilament wire loop is pierced through the capsule and under the torn labrum at the articular margin along the most anteroinferior point (at the 5:00–5:30 o’clock position) on the glenoid (Figure 3A). Tissue is typically grabbed more inferior than the location of the suture anchor in order to perform an inferior to superior capsular shift in addition to a lateral to medial shift. The axillary nerve lies closest to the 6:00 o’clock position and care should be used to avoid this area (2). It is our preference to take a shallower amount of capsular tissue in this area to avoid iatrogenic injury. After passing through the soft tissue, the wire loop is deployed and the penetrator is retracted out of the capsule and removed from the shoulder. It is important to continue feeding the wire while removing the tissue penetrator to avoid de-threading the capsule. With the free ends of the wire parked on the side of the anterior portal, a suture retriever is then introduced through the same anterior portal to bring the looped end of the wire with one limb of the suture anchor simultaneously out of the shoulder to avoid tangling (Figure 3B). Careful suture management is critical when using a single anterior portal technique. Next, the retrieved single limb of suture from the anchor is loaded onto the loop wire which is then shuttled through the capsule and labral complex (Figure 3C). Standard arthroscopic knot-tying technique is then utilized to secure the fixation.
After the lowest anchor, and especially above the equator, we prefer to use knotless anchors (PushLock, Arthrex; Naples, FL), as shown in Figure 4. Knotless anchors avoid potential irritation to the articular cartilage from a prominent suture knot while providing the same degree of fixation to the glenoid (29,30). Each suture is secured and cut before the next anchor is placed in order to simplify suture management (20). The shoulder should be held in neutral to 45 degrees of external rotation when tying sutures to avoid over tensioning (24). These steps are repeated for each anchor used, moving sequentially more superior. An ideal repair has three or more anchors placed inferior to the 3:00 o’clock position, spaced 5–7 mm apart (2,13,20,24). Once completed, the repaired labrum is assessed for stability using a probe. When viewed from the anterior portal, the humeral head should be well centered on the glenoid, indicating balanced soft tissue tensioning (20). Secondary to reduced capsular volume, the arthroscope will now be difficult to maneuver inside the joint and the drive-through sign will be abated (24).

Post-operative management
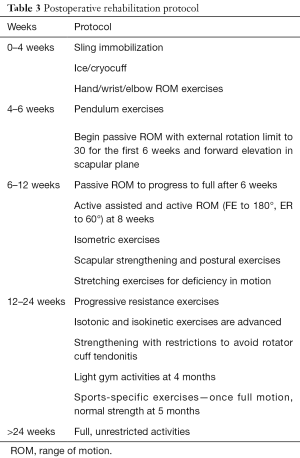
After the wounds are closed, the arm is taken out of traction and placed in an abduction sling. To facilitate the biologic repair process, the shoulder is immobilized in neutral rotation for 4–6 weeks. Return to full, unrestricted activities and sports is at 6 months, postoperatively. The postoperative rehabilitation protocol is shown in Table 3. Modifications in the rehabilitation protocol may be made based on integrity of the tissue at the time of repair and concomitantly performed procedures (2).
Full table
Outcomes
With modern anchors and techniques, the results following arthroscopic anterior stabilization procedures are similar to those of their open counterparts (1). Outcomes are most commonly quantified based on redislocation following repair, but some authors include return to sport, patient reported outcome measures, and the sensation of instability in outcome assessment. In a study by Armangil and colleagues, the single anterior portal technique was specifically investigated (24). They found that with this technique redislocation rates were 5.6% (24). This is in keeping with redislocation rates reported in the literature following arthroscopic repair, which range from 5–18% (1,3,31,32). The most common cause of failure following arthroscopic stabilization is due to glenoid and/or humeral bone deficiencies (2,8,9,33). Other reasons for failure are related to subsequent trauma, age, gender, technical factors, initial causes of instability, and time from instability to surgery (6,19). Many of the causes of failure can be avoided by careful patient selection.
Discussion
The most efficacious management of anterior shoulder instability has been widely investigated in the literature. Surgical management for recurrent instability has long been the standard, with mounting evidence supporting the effectiveness of surgical management following first time dislocation in high risk young individuals (3). Both open and arthroscopic management of anterior shoulder instability yield favorable results (4). In recent decades, arthroscopic procedures have increased dramatically. With this, our understanding of factors predictive of failure as well as overall outcomes following arthroscopic repair have also risen.
Several studies have assessed long-term outcomes following arthroscopic stabilization. A study by Aboalata and colleagues assessed 104 patients who underwent arthroscopic Bankart repair with a minimum of 10-year follow-up (31). They found that the overall patient satisfaction rate was 92.3% and return to pre-injury activity level was 49.5%. Redislocation rates were 18%, influenced significantly by patient age, history of recurrent dislocations, and duration of post-operative rehabilitation (31). Moderate to severe degenerative changes occurred in 12% of patients and was related to the number of dislocation events as well at the number of anchors used (31). These findings are in keeping with a review by Harris and colleagues, which found an 11% redislocation rate and a 26% rate of degenerative changes following arthroscopic stabilization at a mean of 11 years (32). These authors compared outcomes for arthroscopic and open procedures and concluded that the results were similar between the two methods (32).
Factors predictive of inferior outcomes as well as intra-operative and post-operative complications have also been well documented. Appropriately selected patients are imperative to favourable results. Significant glenoid and/or humeral head bone loss is the most common reason for failure following arthroscopic anterior stabilization procedures, but unidentified HAGL lesions and rotator cuff tears also play a significant role (14,34). Further, Bankart repairs performed for patients misdiagnosed as having anterior instability or those who habitually or can voluntarily dislocate their shoulders can result in decreased range of motion, degenerative changes, and poor results with early failure (34). Intra-operative complications include injury to the axillary or musculocutaneous nerves, hardware failure, and insufficient soft-tissue tension related to improperly placed anchors (34). Bioabsorbable tacks are available for glenoid fixation, however, their use has been associated with recurrent effusions, stiffness, and synovitis and therefore their use is not recommended (34). Post-operatively, patients may be affected by stiffness, pain, infection, or chondrolysis (34). Careful attention to patient selection and intra-operative details can minimize these complications and improve results. In cases where recurrence or unsatisfactory results occur, both arthroscopic and open procedures can yield satisfactory results when applied to appropriately selected patients (18).
Pearls and pitfalls
- Appropriate patient selection is critical to the success of arthroscopic procedure. Failure to appreciate significant bone loss will result in a higher rate of recurrent instability. The risk factors outlined by the ISIS are utilized to determine patient suitability for arthroscopic repair. In appropriately selected patients, outcomes following arthroscopic repair approach those of open management.
- When performing labral surgery, our preference is to utilize the lateral decubitus positioning. In our experience, this position gives us improved exposure of the entire glenoid.
- The diagnostic arthroscopy should include an estimation of glenoid bone loss and a dynamic assessment of the Hills-Sachs lesion. Pathology should be viewed from the anterior and posterior portal utilizing combination of both 30° and 70° arthroscope. Associated findings, such as ALPSA and HAGL lesions, should be looked for specifically.
- To successfully utilize the single anterior portal technique, the position is first localized using a spinal needle. The portal must be placed such that instruments can reach all pathologic areas on the anterior glenoid with an appropriate angle of approach. The most difficult area to reach is the inferior pouch, and careful attention should be paid to this area when establishing the anterior portal.
- Careful suture management is critical for a single anterior portal technique to avoid suture tangling.
- If there is difficulty obtaining the appropriate trajectory for drilling or insertion of the inferior anchor using the anterior portal, rather than compromising fixation, a stab incision is made for percutaneous trans-subscapularis anchor placement.
- Overly aggressive passage of the tissue penetrator in the inferior capsule puts the axillary nerve at risk. By taking shallower capsular penetration in this region, the risk of iatrogenic injury is minimized.
- The repair is carried out in an inferior to superior direction, shifting capsulolabral tissue superiorly as each fixation point is secured. Bites taken inferior to the suture anchor can ensure an inferior to superior shift. At least three anchors should be placed, with adequate fixation below the equator on the glenoid.
- At the completion of the repair the anterior labral bumper should be re-established and the humeral head should be centered within the glenoid.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “Trends in Anterior Shoulder Instability”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.10.07). The series “Trends in Anterior Shoulder Instability” was commissioned by the editorial office without any funding or sponsorship. JJS served as the unpaid Guest Editor of the series. AL served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Joint from Jun 2016 to May 2018. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Castagna A, Garofalo R, Conti M, et al. Arthroscopic Bankart repair: Have we finally reached a gold standard? Knee Surg Sports Traumatol Arthrosc 2016;24:398-405. [Crossref] [PubMed]
- Provencher MT, Ghodadra N, Romeo AA. Arthroscopic management of anterior instability: pearls, pitfalls, and lessons learned. Orthop Clin North Am 2010;41:325-37. [Crossref] [PubMed]
- Grumet RC, Bach BR Jr, Provencher MT. Arthroscopic stabilization for first-time versus recurrent shoulder instability. Arthroscopy 2010;26:239-48. [Crossref] [PubMed]
- Archetti Netto N, Tamaoki MJ, Lenza M, et al. Treatment of Bankart lesions in traumatic anterior instability of the shoulder: a randomized controlled trial comparing arthroscopy and open techniques. Arthroscopy 2012;28:900-8. [Crossref] [PubMed]
- van Oostveen DP, Schild FJ, van Haeff MJ, et al. Suture anchors are superior to transglenoid sutures in arthroscopic shoulder stabilization. Arthroscopy 2006;22:1290-7. [Crossref] [PubMed]
- Bak K, Wiesler ER, Poehling GG. Consensus statement on shoulder instability. Arthroscopy 2010;26:249-55. [Crossref] [PubMed]
- Levine WN, Flatow EL. The pathophysiology of shoulder instability. Am J Sports Med 2000;28:910-7. [Crossref] [PubMed]
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94. [Crossref] [PubMed]
- Boileau P, Villalba M, Hery JY, et al. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 2006;88:1755-63. [PubMed]
- Shin SJ, Koh YW, Bui C, et al. What Is the Critical Value of Glenoid Bone Loss at Which Soft Tissue Bankart Repair Does Not Restore Glenohumeral Translation, Restricts Range of Motion, and Leads to Abnormal Humeral Head Position? Am J Sports Med 2016;44:2784-91. [Crossref] [PubMed]
- Shin SJ, Kim RG, Jeon YS, et al. Critical Value of Anterior Glenoid Bone Loss That Leads to Recurrent Glenohumeral Instability After Arthroscopic Bankart Repair. Am J Sports Med 2017;45:1975-81. [Crossref] [PubMed]
- Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from "engaging/non-engaging" lesion to "on-track/off-track" lesion. Arthroscopy 2014;30:90-8. [Crossref] [PubMed]
- Ee GW, Mohamed S, Tan AH. Long term results of arthroscopic Bankart repair for traumatic anterior shoulder instability. J Orthop Surg Res 2011;6:28. [Crossref] [PubMed]
- Arciero RA, Spang JT. Complications in arthroscopic anterior shoulder stabilization: pearls and pitfalls. Instr Course Lect 2008;57:113-24. [PubMed]
- Gagey OJ, Gagey N. The hyperabduction test. J Bone Joint Surg Br 2001;83:69-74. [Crossref] [PubMed]
- Huysmans PE, Haen PS, Kidd M, et al. The shape of the inferior part of the glenoid: a cadaveric study. J Shoulder Elbow Surg 2006;15:759-63. [Crossref] [PubMed]
- Cho NS, Yoo JH, Juh HS, et al. Anterior shoulder instability with engaging Hill-Sachs defects: a comparison of arthroscopic Bankart repair with and without posterior capsulodesis. Knee Surg Sports Traumatol Arthrosc 2016;24:3801-8. [Crossref] [PubMed]
- Shin JJ, Mascarenhas R, Patel AV, et al. Clinical outcomes following revision anterior shoulder arthroscopic capsulolabral stabilization. Arch Orthop Trauma Surg 2015;135:1553-9. [Crossref] [PubMed]
- Porcellini G, Campi F, Pegreffi F, et al. Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg Am 2009;91:2537-42. [Crossref] [PubMed]
- Burkhart S, Lo IK, Brady PC. Burkhart’s View of the Shoulder: A Cowboy’s Guide to Advanced Shoulder Arthroscopy. 1st edition. Philadelphia: Wolters Kluwer, 2006.
- Burkhart S, Lo IK, Brady PC, et al. The Cowboy's Companion: A Trail Guide for the Arthroscopic Shoulder Surgeon. Har/Dvdr edition. Philadelphia: Wolters Kluwer, 2012.
- Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 2007;89:1470-7. [Crossref] [PubMed]
- Phadnis J, Arnold C, Elmorsy A, et al. Utility of the Instability Severity Index Score in Predicting Failure After Arthroscopic Anterior Stabilization of the Shoulder. Am J Sports Med 2015;43:1983-8. [Crossref] [PubMed]
- Armangil M, Basat HC, Akan B, et al. Arthroscopic stabilization of anterior shoulder instability using a single anterior portal. Acta Orthop Traumatol Turc 2015;49:6-12. [PubMed]
- McFarland EG, Neira CA, Gutierrez MI, et al. Clinical significance of the arthroscopic drive-through sign in shoulder surgery. Arthroscopy 2001;17:38-43. [Crossref] [PubMed]
- Flury M, Rickenbacher D, Audige L. Arthroscopic treatment of anterior shoulder instability associated with a HAGL lesion-a case series. J Shoulder Elbow Surg 2016;25:1989-96. [Crossref] [PubMed]
- Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg 2007;16:649-56. [Crossref] [PubMed]
- Frank RM, Mall NA, Gupta D, et al. Inferior suture anchor placement during arthroscopic Bankart repair: influence of portal placement and curved drill guide. Am J Sports Med 2014;42:1182-9. [Crossref] [PubMed]
- Ostermann RC, Hofbauer M, Platzer P, et al. The "Labral Bridge": A Novel Technique for Arthroscopic Anatomic Knotless Bankart Repair. Arthrosc Tech 2015;4:e91-5. [Crossref] [PubMed]
- Ng DZ, Kumar VP. Arthroscopic Bankart repair using knot-tying versus knotless suture anchors: is there a difference? Arthroscopy 2014;30:422-7. [Crossref] [PubMed]
- Aboalata M, Plath JE, Seppel G, et al. Results of Arthroscopic Bankart Repair for Anterior-Inferior Shoulder Instability at 13-Year Follow-up. Am J Sports Med 2017;45:782-7. [Crossref] [PubMed]
- Harris JD, Gupta AK, Mall NA, et al. Long-term outcomes after Bankart shoulder stabilization. Arthroscopy 2013;29:920-33. [Crossref] [PubMed]
- Bushnell BD, Creighton RA, Herring MM. Bony instability of the shoulder. Arthroscopy 2008;24:1061-73. [Crossref] [PubMed]
- Kang RW, Frank RM, Nho SJ, et al. Complications associated with anterior shoulder instability repair. Arthroscopy 2009;25:909-20. [Crossref] [PubMed]
Cite this article as: Sims LA, Shin JJ, Judy RP, Lin A. Arthroscopic soft tissue stabilization: single anterior portal technique. Ann Joint 2017;2:64.


