
Arthroscopic Latarjet—learning curve, results, and complications
Learning curve
Nourissat et al. described an arthroscopically assisted, mini-open Latarjet technique in 2006 (1). The following year, Boileau et al. described the first clinical application performing an arthroscopic Bristow in 40 high-risk patients with recurrent glenohumeral instability (2). Lafosse et al. then described an all-arthroscopic Latarjet technique performed in the beach chair position using two screws (3). In the time since these first clinical applications of the arthroscopic Latarjet, a learning curve has been described in achieving efficient and effective completion (3-5).
While different versions have been published, in general the arthroscopic Latarjet is performed through five major steps: coracoid preparation, drilling, and osteotomy; glenoid preparation; subscapularis splitting with axillary nerve protection; coracoid transfer and fixation; and at our institution a Bankart repair. In a survey by the French Arthroscopy Society, the most difficult steps involved subscapularis splitting, coracoid transfer, and hardware placement (6). They evaluated the learning experience of five surgeons’ first 25 cases each and noted recurrent instability in 6%, neurologic injury in 0.8%, need for revision in 0.8%, and 8% hematoma; showing that even in the early performance of the arthroscopic Latarjet, it could be safely completed.
Further learning curve analysis has been performed by Kany et al., who prospectively evaluated 104 patients and compared their first 30 patients to their last 30 (with 44 procedures in between) (4). They noted three complications during their initial phase (two bone block fractures and one malpositioned screw) and none in their second phase. Their accuracy of positioning the bone block significantly improved in their second cohort of patients and their surgical duration decreased from 103 minutes to 76 minutes. Many studies have similarly found a decrease in operative time when analyzing their learning curves (4,5,7,8). Cunningham et al. reduced their operative time from 183 to 150 minutes after ten cases, then to 95 minutes after another ten cases which matched their open Latarjet duration (5). Although we have seen a learning curve with the arthroscopic Latarjet, this has also been shown with the open Latarjet by Dauzère et al. (9). The authors evaluated their first 69 open Latarjet procedures and found that with experience, their surgical duration decreased along with early complications. It is important to further contextualize these learning curves by noting that there have been learning curves demonstrated for other arthroscopic procedures including hip arthroscopy and arthroscopic rotator cuff repairs (10,11).
As surgeons have a learning curve, so to do procedures. With increasing knowledge and experience, the arthroscopic technique has been refined and guided systems developed to increase reproducibility and potentially reduce complications (12,13). That being said, there is a learning curve for an individual surgeon to anticipate in the form of comfort of the operation, surgical duration and potentially in accurate graft positioning. Therefore, when a surgeon is first performing the procedure they should keep in the mind the option to convert intra-operatively to the open technique; Cunningham et al. converted from arthroscopic to open during 3 of their first 10 cases but none of their remaining 18 cases required intra-operative conversion (5).
In general, we recommend a step-wise learning approach including a surgical observership and cadaver training prior to performance on patients. With proper preparation, the arthroscopic Latarjet can be performed safely and reproducibly. For the procedure to become widespread, it must be safe, but should also reliably produce good results. Indeed, evidence is growing that supports the efficacy of the arthroscopic performance.
Results
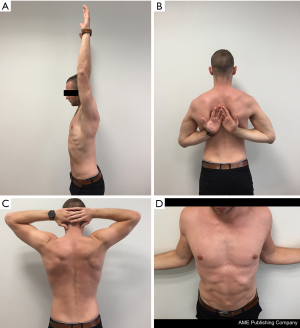
The Latarjet procedure, whether open or arthroscopic, is typically performed in high-risk instability patients (significant bone loss, revision surgery, high-level contact and young athletes) which can increase failure rates (14). Still, overall it performs well and in most cases superiorly when compared to an arthroscopic Bankart repair: Bankart recurrence rates between 0–37.5% (15,16) vs. open Latarjet recurrence rates between 0.3–11.6% (17-19). In fact, many comparative studies conclude that the open Latarjet procedure outperforms a Bankart repair, particularly in the long-term for stability (18,20,21). In this section, we evaluate the arthroscopic Latarjet keeping these baseline comparisons to the open procedure and to the arthroscopic Bankart, while being mindful that the Latarjet is typically reserved for complex patients. In general, benefits of the arthroscopic technique include decreased bleeding, less post-operative pain, ability to treat concomitant pathology, and better cosmesis (Figures 1,2). A summary of specific surgical results in the literature following arthroscopic Latarjet are outlined in Table 1 and presented below in detail. Surgical tips and pearls to improve results are listed in Table 2.

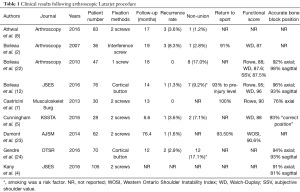
Full table
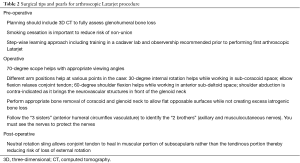
Full table
Recurrence rates
Post-operative recurrence was noted between 0–8.3% of patients with the majority reporting recurrence rates <4% (Table 1) (2,5,7,8,12,22-24). These results compare well with the open Latarjet published in literature, especially given that between 10–49% of these cases are performed in the revision setting (7,8,12,22-24).
Union rates
Union was noted in 83–100% of patients. Smoking was a factor significantly associated with non-union (12,24) and we strictly counsel our Latarjet patients on smoking cessation prior to proceeding with bone block fixation. While most patients achieve union within 2–6 months, we have noted many patients diagnosed with partial or non-union progress to complete union up to 1 year after surgery.
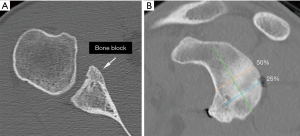
Bone block positioning
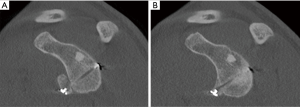
Computed tomography (CT) evaluation of bone block positioning is more accurate than plain films and we only included those studies that used CT for accuracy. The goal of the Latarjet is to recreate the anteroinferior glenoid which is the location typically eroded or fractured in recurrent instability patients (25,26). The optimal position is flush to the glenoid rim (within −5 and +3 mm) and sub-equatorial (4,12) (Figure 3A,B). Accurate positioning was obtained in both axial and sagittal planes in 76–96% of patients (4,5,7,12,22,24). This is an improvement on the open technique as malpositioning of the bone block has been reported in the open Latarjet of 20.6% (27), 53% (28), and up to 67% (29). Positioning is an important factor as an excessively medially placed graft can result in recurrent instability (30) and osteolysis, while a laterally placed graft can accelerate arthritis (27-29).
Return to sport/activity, functional scores, and range of motion (Figure 2)
Return to sport was noted in 91–100% of patients (2,7,12,23). Excellent functional scores were obtained with consistent values of the Rowe and Walch-Duplay scores >90 (2,5,7,12,22) and Western Ontario Shoulder Instability Index (WOSI) of 90.6 (23). A concern with any instability surgery is loss of external rotation post-operatively, particularly in patients who perform overhead sports. The results demonstrate that some degree of loss of external rotation can be expected, between 9–17° (2,7,22). We believe this can be improved by placing patients in neutral rotation slings post-operatively to prevent the conjoint tendon from healing within the tendinous portion of the subscapularis, which can restrict motion.
Studies directly comparing arthroscopic with open Latarjet
Nourissat and the French Arthroscopic Society performed a multicentre analysis of 99 arthroscopic Latarjet patients compared with 85 open Latarjet patients (31). They found that the arthroscopic group had significantly less pain within the first post-operative week. While the arthroscopic group had better WOSI scores at 3 months, by 6 months the open group had better WOSI scores. The same society also compared three groups of patients receiving either open or arthroscopic Latarjet in 390 cases (open Latarjet with two screws, arthroscopic Latarjet with two screws, and arthroscopic Latarjet with suture button) (32). They noted similar recurrence rates and Rowe scores for all techniques: 4.5% and 92.8 for arthroscopic screw fixation, 3% and 95.3 for arthroscopic suture button fixation, and 1% and 83.9 for open Latarjet. There was a significant difference in external rotation at last follow-up: 68.4° for arthroscopic screw, 70.4° for arthroscopic suture button, and 61.1° for open, favoring arthroscopic performance.
Marion et al. prospectively followed 22 open and 36 arthroscopic patients to a mean follow-up of 29.8 months (33). While surgical duration was 15 minutes longer in the arthroscopic group, they noted significantly less pain during the first post-operative week, similar to Nourissat et al. Three patients required revision in the arthroscopic group [8.3%; all involving hardware-related complications (twisted screw with recurrence, prominent screw, and bone-block fracture)] while none in the open group had reoperation. The WOSI scores were similar between the arthroscopic and open groups (82.3 vs. 78.5). On CT evaluation, 59.1% of the arthroscopic grafts were subequatorial compared to 50% of the open grafts.
Randelli et al. performed a systematic review of 23 Latarjet studies (17 open Latarjet with 1,058 shoulders total vs. 6 arthroscopic Latarjet with 259 shoulders total) to identify clinical results and a cost analysis (19). They found a significantly better rate of healing in the open compared to the arthroscopic group (88.6% vs. 77.6%), a non-significant trend towards lower revision surgery in the open group (3.9% vs. 7.8%), and a lower rate of recurrence in the open group (0.3% vs. 3.3%). In contrast, they noted better accuracy of graft positioning in the arthroscopic group (87% vs. 78%). While making some assumptions based on operating time and instrument costs, they determined the arthroscopic Latarjet cost on average 1,295 euros, or twice more than the open technique. They stated that because both techniques produced excellent clinical results (optimal-excellent in 85–100% of arthroscopic and 73–100% of open cases), the higher direct instrument costs of the arthroscopic procedure resulted in it being less cost efficient.
Kordasiewicz et al. compared 62 arthroscopic Latarjet patients with 47 open Latarjet patients each fixed with two screws (34). Their arthroscopic surgical duration was faster (110 vs. 120 minutes) and the arthroscopic group had lower rates of non-union (1.7% vs. 11.9%). They noted similar rates of recurrence for the arthroscopic and open groups (4.8% vs. 6.2%) while revision surgery was required in 9.7% of the arthroscopic group vs. 9.3% of the open group. However, the functional scores for the open group had a higher trend (Rowe 87.8, Walch Duplay 83.9 vs. Rowe 78.9, Walch Duplay 76.7) and there was less loss of external rotation in the open group (7° vs. 14°).
According to current literature, arthroscopic Latarjet performs well regarding stability, functional outcomes, safety, and union rates while allowing more accurate positioning of the bone block. More studies, with higher number of patients and longer outcomes will allow for more definitive conclusions to be drawn.
Complications
Neurologic injury
The open and arthroscopic Latarjet technique should be approached carefully because there are risks to neurologic structures both anteriorly and posteriorly. This was highlighted by Delaney et al. in a neuro-monitoring study of the open Latarjet procedure where they noted that 76.5% of their 34 patients had nerve alert episodes during the procedure, most commonly affecting the musculocutaneous and axillary nerves (35). The most common occurrences were during glenoid exposure and graft placement; it is possible that the amount of retraction necessary to expose the glenoid during an open performance could result in traction injuries. In fact, 20.6% of the patients in that series had axillary nerve deficits post-operatively (fortunately all resolved at a mean 86 days). Using an open Latarjet technique, neurologic injuries have been reported in up to 10% of patients (17,36,37).
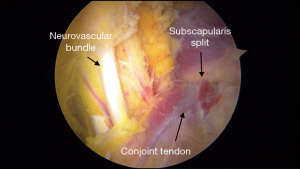
We feel arthroscopic performance can reduce the risk of both direct and traction-related neurologic injuries. First, the surgeon has excellent direct visualization of the axillary and musculocutaneous nerves to facilitate protection of the nerves (Figure 4). Second, less retraction is required for exposure and the coracoid graft does not need to be exteriorized during preparation, both of which reduces risks of traction injuries. In our two published series evaluating 76 and 70 patients respectively, we have not identified any post-operative neurologic deficits (12,24). In a 5-year follow-up study from Lafosse’s group, 1 out of 64 (1.6%) patients was noted to have some wasting of the anterior deltoid (23). Some may argue that these rates are low because they were performed by pioneers of the arthroscopic Latarjet, however, in three studies evaluating learning curve experience, the rate of neurologic injuries were still very low (4,7,9). Dauzère et al. noted one case (1.5%) of axillary nerve palsy which resolved by 3 months (9), Kany et al. similarly found only one transient axillary nerve palsy (0.9%) (4), while Castricini et al. did not encounter any neurologic injuries (7). No injuries to the suprascapular nerve have been described in the arthroscopic Latarjet technique, however, the risk is present if fixation is made >2 cm medial to the posterior glenoid rim (38).
Hardware related
Athwal et al. presented their “North American” experience with the arthroscopic Latarjet and reported similar adverse event rates as in previous open Latarjet reports (8). In a series of 83 patients involving five surgeons, they found a 28% adverse event rate (18% “problem” rate and 10% complication rate). It is interesting to note that 14% of their 28% adverse events appeared to be hardware related (screw backout/bending/failure, graft fracture, hardware removal surgery). Similarly, Dumont et al. found a 12.5% rate of hardware removal for prominent screws (23). This phenomenon of hardware related complications is not unique to the arthroscopic performance as shown by Butt et al. in a systematic review of open Latarjet (all performed using screws) (17). They found hardware-related problems in 6.5% and these were the most common cause for revision surgery. Griesser et al. noted a similar finding in a systematic review of predominantly open Latarjet procedures (90%) (39). Although the rate of re-operation was low (7%), 35% of these were related to symptomatic hardware.
A potential solution to reduce hardware-related complications is the use of non-rigid fixation such as cortical buttons (Figure 5A,B), suture-anchor constructs, or implant-less (12,40,41). Boileau et al. and Gendre et al. used cortical button fixation in 76 and 70 patients respectively and found union rates of 91% and 83% (12,24). No hardware related complications were reported in either of these series. Three reasons may explain this: (I) the button is low profile; (II) the labrum was repaired making the hardware extra-articular, and (III) because re-modelling most commonly affects the proximal pole of the graft (42-44), using a button construct nearer to the distal pole reduces the likelihood of exposed hardware (Figure 5A,B). Zhao et al. reported on 52 patients with a mean follow-up of 39 months using suture anchor fixation of iliac crest allograft (40). They obtained 100% union with no hardware related problems.
Non-union or osteolysis
Remodeling and/or osteolysis has been described after a Latarjet typically affecting the proximal aspect of the coracoid graft (42-44). Following open Latarjet, Di Giacomo et al. found on average 59.5% of total osteolysis on CT at a mean follow-up of 17.5 months (42) while Zhu et al. found an overall incidence of resorption at 1 year of 90.5%, with 49.2% being major-complete using their classification system (43). Kordasiewicz et al. noted partial osteolysis occurring around the proximal screw in 53.3% of their arthroscopic Latarjet patients (34). Haeni et al. evaluated resorption following arthroscopic Latarjet using three-dimensional (3D) CT volume measurements and also noted that the superior half of the graft underwent significant osteolysis by 6 months post-operatively (44). It appears whether the Latarjet procedure is performed open or arthroscopically, the surgeon should expect some degree of graft resorption, particularly proximally. As mentioned above, this may be a source of hardware-related complications if screw heads become prominent and is a reason to consider alternative modes of fixation, such as cortical-buttons.
Conclusions
The arthroscopic Latarjet is an effective procedure for dealing with high-risk glenohumeral instability patients. While it is complex and has an associated learning curve, it can be performed safely and efficiently as demonstrated by surgeons in different practice settings. It allows excellent intra-articular and extra-articular visualization giving the potential to lower neurovascular complications and improve the accuracy of graft placement and fixation. The benefits of arthroscopy are also apparent including better cosmesis, lower post-operative pain, and the flexibility to treat concomitant lesions. Functional results, return to sport, and union rates compare favourably with the open technique. Multiple graft options are available with many modes of fixation options. Detailed systematic and guided techniques are now available increasing the feasibility of the arthroscopic technique. For these reasons, we believe the frequency of the arthroscopic Latarjet will continue to increase with time.
Acknowledgments
The authors would like to thank Agnes Uranovicz for technical support.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Albert Lin and Jason J. Shin) for the series “Trends in Anterior Shoulder Instability” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: The series “Trends in Anterior Shoulder Instability” was commissioned by the editorial office without any funding or sponsorship. PB is an unpaid consultant for Smith and Nephew. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nourissat G, Nedellec G, O'Sullivan NA, et al. Mini-open arthroscopically assisted Bristow-Latarjet procedure for the treatment of patients with anterior shoulder instability: a cadaver study. Arthroscopy 2006;22:1113-8. [Crossref] [PubMed]
- Boileau P, Bicknell RT, El Fegoun AB, et al. Arthroscopic Bristow Procedure for Anterior Instability in Shoulders With a Stretched or Deficient Capsule: The “Belt-and-Suspenders” Operative Technique and Preliminary Results. Arthroscopy 2007;23:593-601. [Crossref] [PubMed]
- Lafosse L, Lejeune E, Bouchard A, et al. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy 2007;23:1242.e1-5. [Crossref] [PubMed]
- Kany J, Flamand O, Grimberg J, et al. Arthroscopic Latarjet procedure: is optimal positioning of the bone block and screws possible ? A prospective computed tomography scan analysis. J Shoulder Elbow Surg 2016;25:69-77. [Crossref] [PubMed]
- Cunningham G, Benchouk S, Kherad O, et al. Comparison of arthroscopic and open Latarjet with a learning curve analysis. Knee Surg Sports Traumatol Arthrosc 2016;24:540-5. [Crossref] [PubMed]
- Lafosse, L, Walch G, Barth, J, et al. Arthroscopic Versus Open Latarjet. In: Boileau P. editor. Nice Shoulder Course 2016. Sauramps Medical, 2016:97-105.
- Castricini R, De Benedetto M, Orlando N, et al. Arthroscopic Latarjet procedure: Analysis of the learning curve. Musculoskelet Surg 2013;97:93-8. [Crossref] [PubMed]
- Athwal GS, Meislin R, Getz C, et al. Short-term Complications of the Arthroscopic Latarjet Procedure: A North American Experience. Arthroscopy 2016;32:1965-70. [Crossref] [PubMed]
- Dauzère F, Faraud A, Lebon J, et al. Is the Latarjet procedure risky? Analysis of complications and learning curve. Knee Surg Sports Traumatol Arthrosc 2016;24:557-63. [Crossref] [PubMed]
- Konan S, Rhee SJ, Haddad FS. Hip arthroscopy: analysis of a single surgeon's learning experience. J Bone Joint Surg Am 2011;93:52-6. [Crossref] [PubMed]
- Guttmann D, Graham RD, MacLennan MJ, et al. Arthroscopic rotator cuff repair: the learning curve. Arthroscopy 2005;21:394-400. [Crossref] [PubMed]
- Boileau P, Gendre P, Baba M, et al. A guided surgical approach and novel fixation method for arthroscopic Latarjet. J Shoulder Elbow Surg 2016;25:78-89. [Crossref] [PubMed]
- Rosso C, Bongiorno V, Samitier G, et al. Technical guide and tips on the all-arthroscopic Latarjet procedure. Knee Surg Sports Traumatol Arthrosc 2016;24:564-72. [Crossref] [PubMed]
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94. [Crossref] [PubMed]
- Hobby J, Griffin D, Dunbar M, et al. Is arthroscopic surgery for stabilisation of chronic shoulder instability as effective as open surgery? A systematic review and meta-analysis of 62 studies including 3044 arthroscopic operations. J Bone Joint Surg Br 2007;89:1188-96. [Crossref] [PubMed]
- Owens BD, DeBerardino TM, Nelson BJ, et al. Long-term follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocations in young athletes. Am J Sports Med 2009;37:669-73. [Crossref] [PubMed]
- Butt U, Charalambous CP. Complications associated with open coracoid transfer procedures for shoulder instability. J Shoulder Elbow Surg 2012;21:1110-9. [Crossref] [PubMed]
- An VV, Sivakumar BS, Phan K, et al. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elbow Surg 2016;25:853-63. [Crossref] [PubMed]
- Randelli P, Fossati C, Stoppani C, et al. Open Latarjet versus arthroscopic Latarjet: clinical results and cost analysis. Knee Surg Sports Traumatol Arthrosc 2016;24:526-32. [Crossref] [PubMed]
- Zimmermann SM, Scheyerer MJ, Farshad M, et al. Long-Term Restoration of Anterior Shoulder Stability: A Retrospective Analysis of Arthroscopic Bankart Repair Versus Open Latarjet Procedure. J Bone Joint Surg Am 2016;98:1954-61. [Crossref] [PubMed]
- Bessière C, Trojani C, Carles M, et al. The open latarjet procedure is more reliable in terms of shoulder stability than arthroscopic bankart repair. Clin Orthop Relat Res 2014;472:2345-51. [Crossref] [PubMed]
- Boileau P, Mercier N, Roussanne Y, et al. Arthroscopic Bankart-Bristow-Latarjet procedure: The development and early results of a safe and reproducible technique. Arthroscopy 2010;26:1434-50. [Crossref] [PubMed]
- Dumont GD, Fogerty S, Rosso C, et al. The Arthroscopic Latarjet Procedure for Anterior Shoulder Instability: 5-Year Minimum Follow-up. Am J Sports Med 2014;42:2560-6. [Crossref] [PubMed]
- Gendre P, Thélu CE, d'Ollonne T, et al. Coracoid bone block fixation with cortical buttons: An alternative to screw fixation? Orthop Traumatol Surg Res 2016;102:983-7. [Crossref] [PubMed]
- Sugaya H, Moriishi J, Dohi M, et al. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am 2003;85-A:878-84. [Crossref] [PubMed]
- Saito H, Itoi E, Sugaya H, et al. Location of the glenoid defect in shoulders with recurrent anterior dislocation. Am J Sports Med 2005;33:889-93. [Crossref] [PubMed]
- Mizuno N, Denard PJ, Raiss P, et al. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg 2014;23:1691-9. [Crossref] [PubMed]
- Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am 1998;80:841-52. [Crossref] [PubMed]
- Hovelius L, Sandström B, Olofsson A, et al. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg 2012;21:647-60. [Crossref] [PubMed]
- Lunn JV, Castellano-Rosa J, Walch G. Recurrent anterior dislocation after the Latarjet procedure: outcome after revision using a modified Eden-Hybinette operation. J Shoulder Elbow Surg 2008;17:744-50. [Crossref] [PubMed]
- Nourissat G, Neyton L, Metais P, et al. Functional outcomes after open versus arthroscopic Latarjet procedure: A prospective comparative study. Orthop Traumatol Surg Res 2016;102:S277-9. [Crossref] [PubMed]
- Metais P, Clavert P, Barth J, et al. Preliminary clinical outcomes of Latarjet-Patte coracoid transfer by arthroscopy vs. open surgery: Prospective multicentre study of 390 cases. Orthop Traumatol Surg Res 2016;102:S271-6. [Crossref] [PubMed]
- Marion B, Klouche S, Deranlot J, et al. A Prospective Comparative Study of Arthroscopic Versus Mini-Open Latarjet Procedure With a Minimum 2-Year Follow-up. Arthroscopy 2017;33:269-77. [Crossref] [PubMed]
- Kordasiewicz B, Małachowski K, Kicinski M, et al. Comparative study of open and arthroscopic coracoid transfer for shoulder anterior instability (Latarjet)-clinical results at short term follow-up. Int Orthop 2017;41:1023-33. [Crossref] [PubMed]
- Delaney RA, Freehill MT, Janfaza DR, et al. 2014 Neer Award Paper: neuromonitoring the Latarjet procedure. J Shoulder Elbow Surg 2014;23:1473-80. [Crossref] [PubMed]
- Shah AA, Butler RB, Romanowski J, et al. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am 2012;94:495-501. [Crossref] [PubMed]
- Ho E, Cofield RH, Balm MR, et al. Neurologic complications of surgery for anterior shoulder instability. J Shoulder Elbow Surg 1999;8:266-70. [Crossref] [PubMed]
- Hawi N, Reinhold A, Suero EM, et al. The Anatomic Basis for the Arthroscopic Latarjet Procedure: A Cadaveric Study. Am J Sports Med 2016;44:497-503. [Crossref] [PubMed]
- Griesser MJ, Harris JD, McCoy BW, et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg 2013;22:286-92. [Crossref] [PubMed]
- Zhao J, Huangfu X, Yang X, et al. Arthroscopic glenoid bone grafting with nonrigid fixation for anterior shoulder instability: 52 patients with 2- to 5-year follow-up. Am J Sports Med 2014;42:831-9. [Crossref] [PubMed]
- Anderl W, Kriegleder B, Heuberer PR. All-arthroscopic implant-free iliac crest bone grafting: new technique and case report. Arthroscopy 2012;28:131-7. [Crossref] [PubMed]
- Di Giacomo G, Costantini A, de Gasperis N, et al. Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: a computed tomography scan study of twenty-six patients. J Shoulder Elbow Surg 2011;20:989-95. [Crossref] [PubMed]
- Zhu YM, Jiang CY, Lu Y, et al. Coracoid bone graft resorption after Latarjet procedure is underestimated: a new classification system and a clinical review with computed tomography evaluation. J Shoulder Elbow Surg 2015;24:1782-8. [Crossref] [PubMed]
- Haeni DL, Opsomer G, Sood A, et al. Three-dimensional volume measurement of coracoid graft osteolysis after arthroscopic Latarjet procedure. J Shoulder Elbow Surg 2017;26:484-9. [Crossref] [PubMed]
Cite this article as: Saliken D, Boileau P. Arthroscopic Latarjet—learning curve, results, and complications. Ann Joint 2017;2:70.


