
The synergistic effect of medial and lateral patellar retinaculum on the stability of patella in full extension
Introduction
Among patients with patellar dislocation, a large portion of them have lateral patellar dislocation, but few of them have medial patellar dislocation. Such categorization of patellar dislocation is almost always due to iatrogenic causes (1-3). What are the reasons? The lateral force vector is larger than that of the medial from the perspective of tensile strength test (4,5). Three distinct structures, a broad tissue band linking the iliotibial band (ITB) to the patella, the patellofemoral, and patellomeniscal ligaments, constitute the lateral soft tissues (6). The ITB was the strongest, with a mean tensile strength of 582N. The medial patellofemoral ligament (MPFL) had a mean tensile strength of 208N (7). Another reason may be the Q angle. The force of the quadriceps acts along the axis of the femur and is resisted by the patellar tendon tension. These two forces are not collinear but diverge by approximately fifteen degrees (8). The Q angle provides a lateral horizontal tension on the patella. The vast majority of patients have lateral patellar displacement (LPD) and tilt. Sallay et al. found that the incidence of a MPFL tear in acute traumatic patellar dislocation was 94% (9). We think that medial retinacular may prevent LPD.
Lateral retinacular release (LRR) is a surgical procedure used to treat excessive lateral pressure syndrome (ELPS) and lateral patellar dislocation and tilt. The occurrence of medial patellar tilt is common (10). However, the chance of medial patellar displacement is relatively low, unless there is also over-tightened MPFL reconstruction (11). Therefore, lateral patellar retinaculum may restrict patellar medial tilt. As a result, the biomechanical characteristics of medial and lateral patellar stabilization are different. The purpose of this cadaveric study was to evaluate the synergistic effect of medial and lateral patellar retinaculum on the stability of patella.
Methods
Materials preparing and model establishment
Eight fresh-frozen specimens of the knee were separated within 24 hours from donors with no history of knee surgery or disease (mean age 47 years, range 34–60, male 5, female 3). All of the specimens had normal bone structures and intact skin. The distal femur and proximal tibia approximating to about 20 cm from the joint line were reserved for each specimen, and the skin and subcutaneous tissues of the knee joints were resected. Then the all specimens had placed onto the homemade knee joint immobilization apparatus. These knee joints were sealed in polyethylene bags and frozen at −20 °C. On the one day before they were used, the knees were thawed in another freezer set to 5 °C.
The specimens were fixed on homemade immobilization apparatus of the knee and placed in their persistent extending position, with rotation impossible. The pulley on the homemade knee joint immobilization apparatus provided a transverse vector force on the patella.
The experimental procedure and investigation parameters
Step 1: normal state. The prepared specimen was placed onto the homemade knee joint immobilization apparatus. CT scan was performed on patellofemoral joint with the integrity of medial and lateral soft tissues, and the scan images were saved (Group N).
Step 2: an anchor was fixed at the midpoint of the medial border of the patella, and a becket was fixed on the medial femoral epicondyle. Then, a force of 2 kg was hung on the other side of the anchor to impose a transverse medial force on the patella using the pulley and becket. CT scan was performed and the images were saved (Group M1). The same procedures were performed on the lateral patella, and this group was named Group L1 (Figure 1A,B).
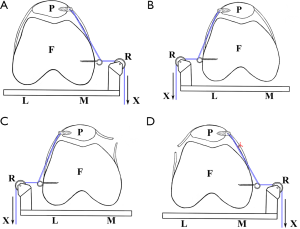
Step 3: a longitudinal dissection was made along the medial border of the patella to separate the medial retinaculum and capsule from the patella. A force of 2 kg was hung on the lateral side of the patella. The lateral patellar retinaculum endured the force of 2 kg (Figure 1C). CT scan was performed on the patellofemoral joint with the dissected medial soft tissues, and the scan images were saved (Group L2). The extreme situations of lateral retinaculum contracture and medial retinaculum relaxation were simulated.
Step 4: the dissected medial soft tissues were sutured in-situ. A longitudinal dissection was made along the lateral border of the patella to separate the lateral retinaculum and capsule from the patella. The next procedures were similar to Step 3 (Figure 1D). CT scan was performed on the patellofemoral joint and the images were saved (Group M2). This group simulated LRR and over-tightened MPFL reconstruction.
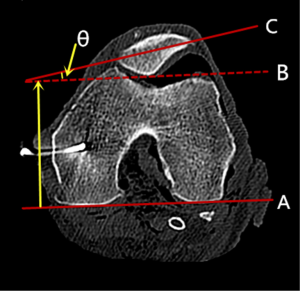
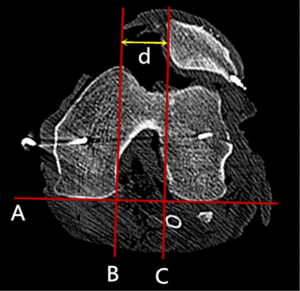
Finally, the scanned images of these five groups were analyzed for the measurement of patellar tilt angle (PTA) (Figure 2) and the LPD (Figure 3). CT images were measured using the software program SIENET Magicview-DICOM.
Statistics analysis
All the data were expressed as mean ± standard deviation and performed using SPSS version 16.0. The independent student t-test was used to compare PTA and LPD values between Group N and Group M1, Group N and Group L1, Group N and Group L2, Group N and Group M2, Group L2 and Group M2, respectively. A P value of less than 0.01 was considered statistically significant.
Results
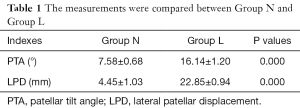
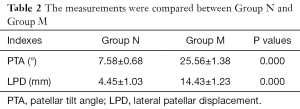
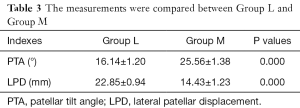
PTA (°) and LPD (mm) of Group N were 7.58±0.68 and 4.45±1.03, respectively, and they were in the normal range. PTA (°) and LPD (mm) of Group M1 and Group L1 were not significantly different compared to Group N (P≥0.01). PTA (°) and LPD (mm) values of Group L2 were 16.14±1.20 and 22.85±0.94, respectively, significantly higher compared to Group N (P≤0.01). PTA (°) and LPD (mm) of Group M2 were 25.56±1.38 and 14.43±1.23, respectively, significantly higher compared to Group N (P≤0.01). PTA and LPD showed significant differences between Group L2 and Group M2 (P≤0.01). In Group L2, PTA (°) was significantly beyond the normal range, indicating patellar lateral tilt; and LPD (mm) was significantly beyond the normal range, indicating patellar lateral displacement. In Group M2, PTA (°) was significantly beyond the normal range, indicating patellar medial tilt; and LPD (mm) was significantly beyond the normal range, indicating patellar medial displacement.
Discussion
Instability of the patellofemoral joint is a multifactorial problem. Patellar stability relies on the normal limb alignment, the well-developed osseous architecture of the patella and the trochlea, the integrity of the soft-tissue constraints, and the interplay of the quadriceps femoris muscle (5,12). The medial and lateral passive soft tissue restraints are particularly important for patellar tracking and stability (13). In this study we used cadaveric knees with normal bone structures to explore the individual contribution of medial and lateral patellar retinaculum to the stability of the patella.
Medial soft tissue restraints attached to the patella are crucial in preventing lateral patellar dislocation as forces are transferred through the extensor mechanism (14-20). In this study, the medial soft tissues were transsected. The patella was given a lateral transverse force vector. PTA and LPD of lateral stress group were measured using CT scans and showed significant differences compared to Group N (Table 1). These data indicate that the role of medial stabilizer is pulling the patella medial and avoiding LPD. Meanwhile, pulling the patella backward to match the femoral trochlea could maintain a good medial patellofemoral joint cooperation relationship. Therefore, medial patellar retinaculum has two functions: to avoid LPD by medial transverse force vector; and to avoid anterolateral patellar tilt by posterior force vector.
Full table
Many orthopaedic surgeons have attributed medial patellar instability complication caused by over-released of the LRR to all lateral release procedures (1,2,20-22). An isolated LRR has been reported to be ineffective for the treatment of patellar instability (23), and most studies have shown disappointing mid and long-term results (24,25). In our experiments, the lateral soft tissues were transsected. The patella was given a medial transverse force vector. PTA and LPD of medial stress group were measured by using CT scan and showed significant differences compared to Group N (Table 2). These data indicate that the role of lateral stable structure is pulling the patella lateral and avoiding medial patellar displacement. Meanwhile, pulling the patella posterior to match femoral trochlea could maintain a good lateral patellofemoral joint cooperation relationship. Therefore, lateral patellar retinaculum has two functions: to avoid medial patellar displacement by lateral transverse force vector; and to avoid anteromedial patellar tilt by posterior force vector.
Full table
In addition, we compared PTA values of Group L2 and Group M2 by independent student t-test, and the results suggest that the lateral retinaculum injury has stronger effect on patellar tilt than medial retinaculum injury has. Moreover, we compared LPD values of Group L2 and Group M2 and the results indicate that the medial retinaculum injury has stronger effect on patellar displacement than lateral retinaculum injury has (Table 3). Taken together, our results suggest that the medial retinaculum has two functions: to avoid LPD by medial transverse force vector; and to avoid anterolateral patellar tilt by posterior force vector. The most important function of lateral retinaculum is the posterior force vector to restrict anteromedial patellar tilt, while the function of lateral transverse force vector restricting medial patellar displacement is relatively weak.
Full table
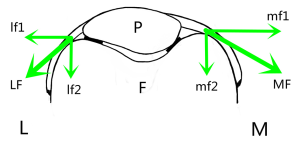
Cutting of medial retinaculum had more impact on lateral patellar displacement (LPD: 22.85±0.94 mm) than cutting of the lateral retinaculum had on medial patellar displacement (LPD: 14.43±1.23 mm). The quadriceps-patella-patellar tendon (tubercle of tibia) complexus also provided a transverse lateral vector force to the patella and made up the deficiency of the lateral tension of lateral patellar retinaculum. The complexus and lateral patellar retinacular transverse resultant force together to counter the medial patellar retinacular transverse force. Through the counterweight mechanism, the patella stays a stable state at all range of angles of knee flexion. Thus complexus plays a crucial role in regulating and controlling the patellar stability.
Considering the special anatomical structure of the normal patella and femoral trochlea, the lateral trochlear surface is nearly vertical to the posterior femoral condyles line on the axial view. However, the medial trochlear surface is more inclined (20,26,27). They are both providing buttresses to patella thereby maintaining the patella’s centred position in the trochlea (20). The forces to the patella provided by medial and lateral retinaculum were decomposition by the femoral trochlear geometrical shape (Figure 4). We found similar lateral patellar tilt and medial patellar tilt between Group L2 and Group M2. Therefore the transverse tension of medial and that of lateral patellar retinaculum have synergistic effect and help the patella to keep balance and match relation with femoral trochlea. Because the lateral trochlear surface is nearly vertical, the most significant effect of lateral patellar retinaculum is to keep the patellar rotation balance, so as to effectively restrain patellar medial tilt.
During the treatment, for patients with normal bone structures (femoral trochlear, patella, tubercle of tibia, et al.), surgeries such as the isolated LRR or medial patellofemoral ligament (MPFL) reconstruction procedure are not recommended, especially considering the muscles (11,14). Among the 168 cases of medial patellar instability reported in the literature, 153 (91%) occurred in patients who had undergone previous LRR, either isolated or associated with realignment surgery (28,29). Redislocation of the patella was observed in 28% of patients after isolated quadricepsplasty surgery (30). Therefore, orthopaedic surgeons should pay special attention to the adaptation of isolated LRR during the treatment of patellar instability (23,31). They could select limited LRR (not over-release) or lateral retinacular reconstruction (28). Moreover, MPFL reconstruction should be abandoned, because the decreased occurrence of patellar redislocation was associated with tighten MPFL reconstruction (12). Large medial tension may lead to the iatrogenic medial patellar instability and accelerate the speed of femoral trochlear and patellar chondral abrasions (32,33). Therefore, individualized surgery should be used for different patients based on their own conditions during the treatment, so that lateral and medial patellar retinaculum can function cooperatively to restore normal knee activity.
The results of the cadaveric study indicate that medial patellar retinaculum prevents LPD and lateral patellar tilt. Lateral patellar retinaculum provides a retractive force to prevent medial patellar tilt. Medial and lateral retinaculum show synergistic effect to stabilize the patella. However, the study has the following limitations: the most important of these relates to the use of isolated joints, rather than studying the knee as an integral part of the functioning, loaded, lower limb. This study only measured the medial and lateral passive soft tissue restraints. The symptoms of patellar instability often appear as a sudden dynamic event which cannot be simulated. Also the muscle factors cannot be assessed. Further patellofemoral joint biomechanical and clinical studies should be conducted.
Conclusions
Medial patellar retinaculum plays an important role to prevent LPD and lateral patellar tilt. And lateral patellar retinaculum can provide a retractive force to prevent medial patellar tilt. Medial and lateral retinaculum show synergistic effect to stabilize the patella.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.12.06). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was approved by the Medical Ethical Committee of the Third Hospital of Hebei Medical University (K2017-002-012) and was conducted in accordance with the Helsinki Declaration of 1964 (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sanchis-Alfonso V, Merchant AC. Iatrogenic Medial Patellar Instability: An Avoidable Injury. Arthroscopy 2015;31:1628-32. [Crossref] [PubMed]
- Hughston JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am 1994;76:1328-44. [Crossref] [PubMed]
- Sawyer GA, Cram T, LaPrade RF. Lateral patellotibial ligament reconstruction for medial patellar instability. Arthrosc Tech 2014;3:e547-50. [Crossref] [PubMed]
- Reider B, Marshall JL, Koslin B, et al. The anterior aspect of the knee joint. J Bone Joint Surg Am 1981;63:351-6. [Crossref] [PubMed]
- Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am 2008;90:2751-62. [Crossref] [PubMed]
- Merican AM, Sanghavi S, Iranpour F, et al. The structural properties of the lateral retinaculum and capsular complex of the knee. J Biomech 2009;42:2323-9. [Crossref] [PubMed]
- Mountney J, Senavongse W, Amis AA, et al. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br 2005;87:36-40. [PubMed]
- Türkmen F, Acar MA, Kacira BK, et al. A new diagnostic parameter for patellofemoral pain. Int J Clin Exp Med 2015;8:11563-6. [PubMed]
- Sallay PI, Poggi J, Speer KP, et al. Acute dislocation of the patella: A correlative pathoanatomic study. Am J Sports Med 1996;24:52-60. [Crossref] [PubMed]
- Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med 2006;34:1478-85. [Crossref] [PubMed]
- Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med 2006;34:1254-61. [Crossref] [PubMed]
- Zaffagnini S, Dejour D, Grassi A, et al. Patellofemoral anatomy and biomechanics: current concepts. Joints 2013;1:15-20. [PubMed]
- Amis AA, Firer P, Mountney J, et al. Anatomy and biomechanics of the medial patellofemoral ligament. Knee 2003;10:215-20. [Crossref] [PubMed]
- Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 1998;26:59-65. [Crossref] [PubMed]
- Conlan T, Garth WP, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 1993;75:682-93. [Crossref] [PubMed]
- Hall JE, Micheli LJ, McManama GB. Semitendinosus tenodesis for recurrent subluxation or dislocation of the patella. Clin Orthop Relat Res 1979;31-5. [PubMed]
- Arnbjörnsson A, Egund N, Rydling O, et al. The natural history of recurrent dislocation of the patella: long-term results of conservative and operative treatment. J Bone Joint Surg Br 1992;74:140-2. [PubMed]
- Baker RH, Carroll N, Dewar FP, et al. The semitendinosus tenodesis for recurrent dislocation of the patella. J Bone Joint Surg Br 1972;54:103-9. [PubMed]
- Senavongse W, Amis AA. The effects of articular, retinacular, or muscular deficiencies on patellofemoral joint stability. J Bone Joint Surg Br 2005;87:577-82. [Crossref] [PubMed]
- Rhee SJ, Pavlou G, Oakley J, et al. Modern management of patellar instability. Int Orthop 2012;36:2447-56. [Crossref] [PubMed]
- Christoforakis J, Bull AM, Strachan RK, et al. Effects of lateral retinacular release on the lateral stability of the patella. Knee Surg Sports Traumatol Arthrosc 2006;14:273-7. [Crossref] [PubMed]
- Lattermann C, Toth J, Bach BR. The role of lateral retinacular release in the treatment of patellar instability. Sports Med Arthrosc 2007;15:57-60. [Crossref] [PubMed]
- Kolowich PA, Paulos LE, Rosenberg TD, et al. Lateral release of the patella: indications and contraindications. Am J Sports Med 1990;18:359-65. [Crossref] [PubMed]
- Aglietti P, Pisaneschi A. BIase P De. Recurrent dislocation of patella: three kinds of surgical treatment. Ital J Orthop Traumatol 1992;18:25-36. [PubMed]
- Lattermann C, Toth J, Bach BR Jr. The role of lateral retinacular release in the treatment of patellar instability. Sports Med Arthrosc 2007;15:57-60. [Crossref] [PubMed]
- Panagiotopoulos E, Strzelczyk P, Herrmann M, et al. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 2006;14:7-12. [Crossref] [PubMed]
- Shih YF, Bull AM, Amis AA. The cartilaginous and osseous geometry of the femoral trochlear groove. Knee Surg Sports Traumatol Arthrosc 2004;12:300-6. [Crossref] [PubMed]
- Sanchis-Alfonso V, Montesinos-Berry E, Monllau JC. Results of isolated lateral retinacular reconstruction for iatrogenic medial patellar instability. Arthroscopy 2015;31:422-7. [Crossref] [PubMed]
- Udagawa K, Niki Y, Matsumoto H, et al. Lateral patellar retinaculum reconstruction for medial patellar instability following lateral retinacular release: A case report. Knee 2014;21:336-9. [Crossref] [PubMed]
- Bergman NR, Williams PF. Habitual dislocation of the patella in flexion. J Bone Joint Surg Br 1988;70:415-9. [PubMed]
- Gerbino PG, Zurakowski D, Soto R. at al. Long-term functional outcome after lateral patellar retinacular release in adolescents: an observational cohort study with minimum 5-year follow-up. J Pediatr Orthop 2008;28:118-23. [Crossref] [PubMed]
- Tom A, Fulkerson JP. Restoration of native medial patellofemoral ligament support after patella dislocation. Sports Med Arthrosc 2007;15:68-71. [Crossref] [PubMed]
- Beck P, Brown NA, Greis PE, et al. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med 2007;35:1557-63. [Crossref] [PubMed]
Cite this article as: Lu J, Wang Y, Niu Y, Bai W, Liang S, Ma H, Duan G, Wang F. The synergistic effect of medial and lateral patellar retinaculum on the stability of patella in full extension. Ann Joint 2017;2:80.


