Outcomes after arthroscopic surgery for femoroacetabular impingement with global pincer: a systematic review
Introduction
Femoroacetabular impingement (FAI) is a condition in which atypical collision between the proximal femur and acetabulum is caused by abnormal morphology of the hip joint (1). While FAI can be caused by an isolated deformity to either the acetabulum (Pincer) or the femoral head and neck junction (Cam), the majority of patients present with elements of both structural abnormalities (2). Pincer-type FAI can occur in focal or global forms, each having varying amounts of acetabular overcoverage. Global overcoverage is more generalized affecting both the anterior and posterior acetabular rims, and can be associated with radiographic signs of a deep hip socket represented by coxa profunda or protrusio acetabuli (3). Protrusio acetabuli is an extreme form of overcoverage in which the femoral head protrudes into the true pelvis (4,5). This condition is defined radiographically as the femoral head extending to or projecting medial to the ilioischial line on an anteroposterior radiograph of the pelvis (6). The acetabulum usually presents with an increased size of the articular surface (7), which is reflected by a lateral center-edge angle (LCEA) classically greater than 39 degrees (8). Protrusio acetabuli with global overcoverage can predispose the young adult to develop hip pain and early osteoarthritis (OA) (9).
Global pincer-type FAI has traditionally been treated with an intertrochanteric valgus osteotomy and medialization of the proximal femur (5,9,10). This procedure acts to reduce the static pressure on the medial joint surface. Biomechanically, however, the dynamic problem of impingement in these hips can remain (4,10). This may explain the limited post-operative success seen with early and midterm surveillance (8,9). Open acetabuloplasty has been attempted to normalize the amount of coverage (10). However, the clinical value of open surgical correction of severe global overcoverage and protrusio has not demonstrated a convincing benefit to patients (11).
Open and arthroscopic management of FAI are equally effective, with the latter showing reduced rates of post-operative complications (12,13). However, the utility for treating global acetabular overcoverage is less understood. Advancement of instrumentation and techniques have broadened the applications of hip arthroscopy to treat complex bony deformities conventionally managed with open surgery (14). There has been no systematic review that has summarized the existing clinical literature on arthroscopic treatment of global pincer-type FAI. Therefore, the purpose of this study was to systematically assess the arthroscopic management of global pincer-type FAI, including clinical and radiological outcomes and complications associated with this procedure. It was hypothesized that arthroscopic treatment of global pincer could provide improvement in pain and function in the short term with minimal rates of complications.
Materials and methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed to evaluate and assess study selection using methodology previously employed by our institution for conducting systematic reviews (15,16).
Search strategy
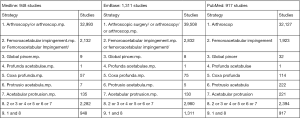
A comprehensive literature search on arthroscopic management of global pincer-type FAI was performed using three online databases, PubMed, EMBASE, and Ovid (MEDLINE), from database inception until September 21st, 2017. Medical Subject Headings (MeSH) terms and designated free-text terms were incorporated for “arthroscopy”, “femoroacetabular impingement”, “global pincer”, “profunda acetabulae”, “coxa profunda”, “protrusio acetabula”, and “acetabular protrusion” (Figure S1).
Study screening
Two authors (M.M. and J.K.) independently assessed the titles, abstracts, and full-text articles identified by the search strategy. Any disagreements were discussed between reviewers. If no consensus was reached, the senior author (O.R.A.) was available to make the final decision regarding study inclusion. We performed additional citation tracking by screening the reference lists of the eligible studies.
Assessment of study eligibility
The research question and eligibility criteria were determined a priori. Original articles were included if (I) full text were available in English; (II) studies were conducted on live human subjects; (III) studies were on arthroscopic management of global pincer-type FAI; and (IV) studies of all levels of evidence reported any outcomes including subjective outcomes, radiographic outcomes, complications, and outcome scores. Imaging studies, animal studies, anatomic and histologic studies, surgical technical reports, book chapters and review articles were excluded.
Data abstraction
Data from original articles were extracted by two reviewers (M.M. and J.K.) into a customized database using a Microsoft Excel spreadsheet (Version 2007, Microsoft, Redmond, WA, USA). Data extraction disagreements were discussed between the two reviewers. If any disagreement was still present, the senior author (O.R.A.) was utilized to resolve any continued disagreementS Data elements included were year of publication, author, study design, age, gender, number of participants, follow up duration, level of evidence, and outcomes.
Quality assessment
The MINORS (methodological index for non-randomized studies) checklist was used to assess the methodologic quality of the included studies (17). The two reviewers (M.M. and J.K.) thoroughly reviewed the guidelines for grading studies using this index. By use of the MINORS checklist, comparative studies can obtain a maximum score of 24, whereas non-comparative studies can be given a maximum score of 16. A score of 0–8 or 0–12 was considered poor quality for non-comparative and comparative studies, respectively, while a score of 9–12 or 13–18 was considered fair quality, and a score of 13–16 or 19–24 was considered excellent quality. Any disagreements were discussed between the reviewers and a senior author until consensus was reached.
Assessment of agreement
Inter-reviewer agreement for the title, abstract, and full-text articles was calculated with the κ statistic. An intra-class correlation coefficient (ICC) was calculated for the quality assessment using the MINORS criteria. The values were categorized a priori as follows: κ/ICC of 0.61 or greater was considered substantial agreement; κ/ICC of 0.21 to 0.60, moderate agreement; and κ/ICC of 0.20 or less, slight agreement (18).
Statistical analysis
Given the non-uniform nature of the studies included in this systematic review in terms of techniques and outcome reporting, the results are presented in a narrative summary fashion. Descriptive statistics including means, proportions, ranges, kappa values, and ICC values were calculated using Minitab® statistical software (Version 17, Minitab Inc., State College, USA).
Results
Search strategy
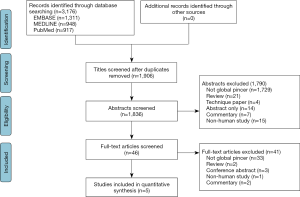
The initial search of three databases resulted in 3,176 titles for screening. A total of 1,270 studies were removed as duplicates, resulting in 1,906 studies available for screening. A systematic screening approach removed articles failing to meet inclusion criteria and resulted in 5 available full-text articles for review (Figure 1). There was substantial agreement among reviewers at the title (κ =0.827; 95% CI, 0.777 to 0.877), abstract (κ =0.843; 95% CI, 0.795 to 0.891), and full-text (κ =1.00) screening stages.
Study characteristics
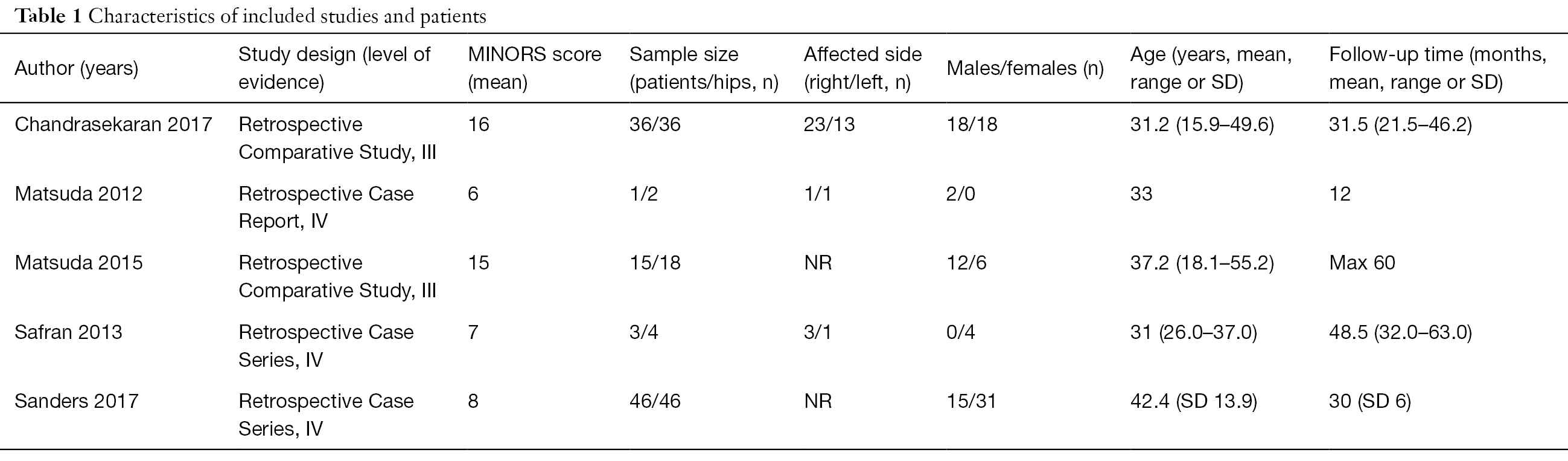
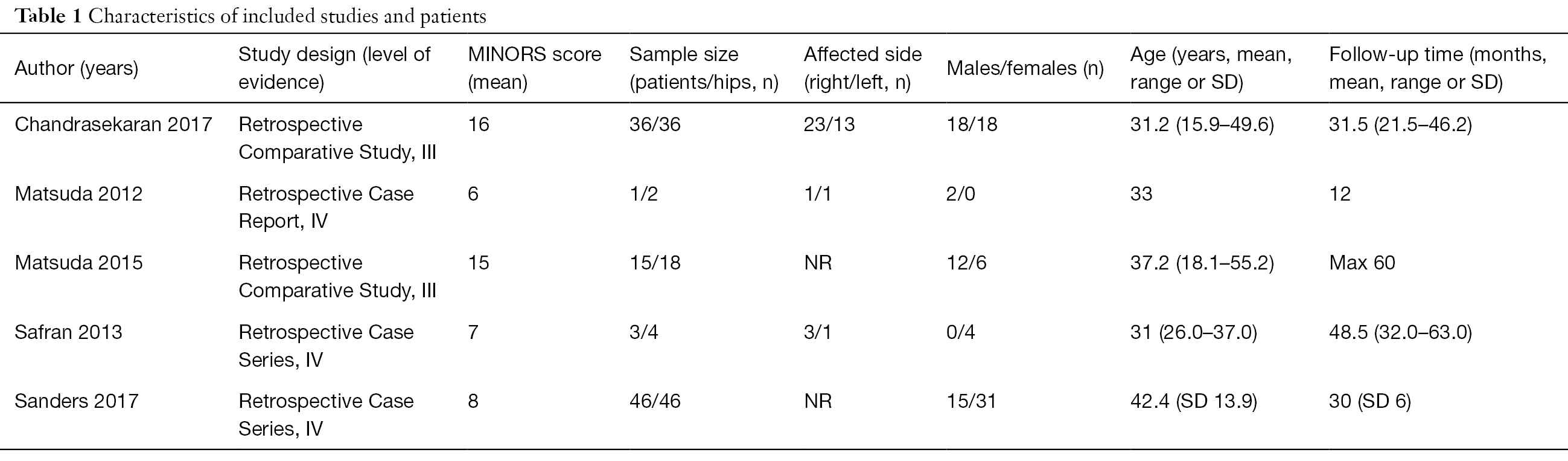
In total, 101 patients (106 hips) with a mean age of 35.0 (range, 15.9 to 55.2) years underwent hip arthroscopy for the management of global pincer-type FAI. Of the included cases, 55.7% were female and they were followed up for a mean of 30.5 (range, 12 to 63) months (Table 1).
Full table
Study quality
We identified 1 case report, 2 case series, and 2 comparative studies, which had a level of evidence of IV, IV, and III, respectively (Table 1). The median MINORS score for the non-comparative studies was 7 out of 16 (range, 6 to 8) demonstrating low quality evidence. Further, the median MINORS score for the comparative studies was 15.5 out of 24 (range, 15 to 16) demonstrating fair quality evidence. Overall, 100% of studies had a clearly stated aim and loss of follow up less than 5%. However, only 40% of studies had unbiased assessment of study endpointS Overall, there was substantial inter-rater agreement for the MINORS score with an ICC of 0.798 (95% CI, 0.749 to 0.847).
Pre-operative diagnoses and management
Of the 106 cases included in this systematic review, 100 (94.3%) were diagnosed with coxa profunda, while 6 (5.7%) were diagnosed with protrusio acetabula (Table S1). Two studies reported a LCEA >40° as inclusion criteria for global overcoverage (19,20), one study used LCEA >35° with radiographic signs of coxa profunda (21), one study used LCEA ≥50° with radiographic signs of protrusio acetabuli (22), and one case report was of a 33-year-old male with bilateral coxa profunda with a LCEA of 56° on the right hip and 46° on the left hip (23). Plain radiographs were obtained pre-operatively for all 106 cases, including the anteroposterior view, 45° Dunn view, false profile view, and cross-table lateral or frog leg lateral view. Magnetic resonance imaging was obtained in two studies for 48 cases to assess for the status of the articular cartilage and labrum (21,23). Non-operative measures were reported by 1 study including 4 cases, which included image-guided local anesthetic injections (22).
Full table
Operative procedures and findings
Of the 106 cases included in this review, 106 (100%) underwent acetabuloplasty; 91 (85.9%) underwent femoroplasty; 35 (33.0%) underwent labrum repair; 5 (4.7%) underwent labrum reconstruction; 19 (17.9%) underwent partial or complete labrectomy; 33 (31.1%) underwent chondroplasty, of which 21 (19.8%) were specified as acetabular chondroplasty and 10 (9.4%) were specified as femoral head chondroplasty; 2 (1.9%) underwent acetabular microfracture; 1 (0.9%) underwent femoral head microfracture; 24 (22.6%) underwent ligamentum teres treatment, 10 (9.4%) underwent iliopsoas release; 1 (0.9%) underwent trochanteric bursectomy; and 7 (6.6%) underwent removal of a loose body. Of the 36 cases for which capsular treatment was reported, 20 (55.6%) underwent capsular repair and 16 (44.4%) underwent capsular release. Intraoperative findings were reported by three studies for 42 cases, and they included the degree of acetabular and femoral head chondral lesions, as graded by the Outerbridge criteria and the acetabular labrum articular disruption grading system. Additionally, the location and sizes of labral injuries were described by these studies. The details are summarized in Table S1.
Outcomes
Standardized outcome scores
Of the 3 studies including 86 cases (19,21,22), which reported on Modified Harris Hip Score (mHHS) outcomes, the mean improvement from pre-operative to post-operative scores was 53.9 to 80.7 (Table S2). Of the 3 studies including 56 cases (19,20,23), which reported on Non-Arthritic Hip Score (NAHS) outcomes, the mean improvement from pre-operative to post-operative scores was 50.5 to 79.1. With regards to the single study including 36 cases (19), which reported on the Hip Outcome Score Sports-Specific Subscale and Activities of Daily Living Subscale, the mean post-operative scores were 46.0 and 66.3, respectively. With regards to the single study including 46 cases (21), which reported on the Activity of Daily Living Score (ADL), Activity of Daily Living Rating (ADLR), Sports Score, Sports Rating, level of function, and International Hip Outcome Tool (IHOT), the mean post-operative scores were 81.5, 81.8, 65.3, 65.9, 14.0, and 69.7, respectively.
Subjective outcomes
Two studies including 54 cases (19,20), reported on patient satisfaction. In one study, the mean satisfaction at 24 months post-operatively for both the global and focal pincer groups was 4.2 (5-point Likert scale) (20). In another comparative study, the global pincer group has significantly lower patient satisfaction scores compared to the control group with focal pincer: 6.61 versus 7.91 (scale out of 10), respectively (P=0.019) (19). Additionally, 2 other studies including 6 cases reported that patients were highly satisfied with their post-operative outcomes (22,23). One study including 36 cases reported a post-operative visual analogue score (VAS) of 5.84 (range 0–10) (19). Additionally, one study including 4 cases reported that all patients returned to work post-operatively (22).
Radiographic outcomes
One study on global pincer treated arthroscopically reported a mean post-operative LCEA correction of 28.8±5.3° (19). Sanders et al. showed a mean pre-operative LCEA of 39.9±2.4° and obtained a mean post-operative correction of 30.8±1.8° (21). Of the 4 studies including 60 cases (19,21-23), which reported on LCEA outcomes, the mean improvement from the pre-operative to post-operative period was 48.9° to 37.9°. Of the 2 studies including 82 cases (19,21), which reported on alpha angle outcomes, the mean improvement from the pre-operative to post-operative radiographs were 62.3° to 48.1°. Of the 2 studies including 82 cases (19,21), which reported on radiographic crossover sign outcomes, the mean prevalence from the pre-operative to post-operative period was 37.8% to 8.5%. One study including 36 cases reported that the percentage of crossover improved from 16.1% preoperatively to 5.0% postoperatively (19). Further, 1 study including 46 studies reported Tönnis angles (21), which improved from 0.5° preoperatively to 2.3° postoperatively. Additionally, 1 study including 36 cases reported acetabular inclination (19), which improved from –1.19° preoperatively to 4.46° postoperatively. The same study reported that 17 (47.2%) cases had a positive ischial spine sign preoperatively, while 7 (19.4%) cases had a positive ischial spine sign postoperatively.
Revision procedures and complications
Of the 2 studies including 54 cases (19,22), which reported on the number of revision arthroscopic procedures, 2 (3.7%) cases underwent revision arthroscopic procedures by a mean time of 6.67 months post-operatively at a mean age of 29 years. Both patients were found to have new labral tears that were repaired and one patient had a full-thickness acetabular cartilage defect treated with microfracture. Of the 2 studies including 54 cases (19,20), which reported on the number of conversions to total hip arthroplasty (THA), 5 (9.3%) cases were converted to THA by a mean time of 13.1 months post-operatively (mean age of 40.9 years). A comparative study between 15 global pincer patients and 125 focal pincer patients showed no significant differences in THA conversion rates (5.5% and 6.2%, respectively) (20). In contrast, Chandrasekaran et al. reported that patients undergoing hip arthroscopic surgery for symptomatic global overcoverage and profunda (n=39) had a significantly higher incidence of conversion to THA than the matched cohort with normal coverage (n=39) (4 versus 0 patients) (P=0.040) (19). Of the 106 cases included in this review, there was 1 complication (0.9%), which included transient pudendal neurapraxia lasting 3 months before complete spontaneous resolution.
Discussion
Key findings
Overall, five studies evaluating the arthroscopic management of global pincer-type FAI were identified in the literature. Two studies showed significant post-operative improvement in patient-reported outcomes (19,20). Sanders et al. only reported mean post-operative functional outcome scores at 2.5 years (21). While there were no pre-operative scores for comparison, the values were similar to previously reported scores for traditional FAI (24-26). It is difficult to know whether the results are generalizable to protrusio acetabuli, the most severe form of global pincer-type FAI. Previous work has suggested that it may act via a different pathomechanism than the much more prevalent coxa profunda (10). A case report and small case series on arthroscopic treatment of protrusio acetabuli have reported successful short-term outcomes (22,23). However, it is important to be mindful that arthroscopic treatment of global acetabular overcoverage presents technical challenges that need to be appreciated by the experienced surgeon.
Sanders et al. found that an increased Tönnis OA score was associated with worse functional outcomes following arthroscopically corrected global overcoverage (21). This is similar to a study of open acetabular rim resection that compared patients with and without protrusio acetabuli (11). The authors found that having a Tönnis OA score ≥1 was a significant predictor for failure, defined as conversion to THA, progression of OA, and a Merle d’Aubigne-Postel score <15 at latest follow-up (P=0.001). A recent systematic review concluded that the presence of OA was a strong predictor of poor outcomes following hip arthroscopy (27).
The rate of conversion to THA was poorly reported in studies of arthroscopic global pincer correction. With respect to open procedures, the survival of globally over-covered hips was found to be markedly inferior to focal FAI (11). However, it is important to emphasize that this study only included protrusio acetabuli, thus preventing generalized conclusions. A recent review by Nwachukwu et al. comparing open and arthroscopic treatments of classic FAI at a minimum 36-month follow-up reported that the heterogeneity of outcome measures made it difficult to compare treatment groups (28). However, the rates of conversion to THA were 7% and 9.5% for open and arthroscopic groups, respectively (P=0.06). A study of open and arthroscopic treatments of symptomatic global pincer-type FAI is required to facilitate comparisons between both treatment arms.
Strengths
This was the first paper to systematically review this novel arthroscopic approach to the management of globally over-covered hips. While this paper serves to bring awareness to the rising innovation and new frontiers of hip arthroscopy, it highlights the importance of maintaining evidence-based practice. Our expansive search strategy across multiple databases and broad inclusion criteria ensured that all relevant articles were included. Furthermore, the excellent agreement amongst the two reviewers at all screening stages and quality assessment suggests that a thorough methodology was employed in the preparation of this review.
Limitations
The methodologic quality in this review is limited by the quantity and quality of studies available on arthroscopic treatment of global pincer-type FAI. The paucity of comparative studies on arthroscopic versus open management of global pincer-type FAI precludes definitive conclusions on their respective indications and relative efficacy. The reporting of data within the studies was inconsistent, including information regarding pre-operative diagnosis, arthroscopic technique, and clinical outcome scores. Given the difficult learning curve for arthroscopic global pincer correction, there may be expertise bias underlying the favorable outcomes in some studies. Thus, results may not be generalizable to surgeons who are not as familiar with this condition and surgical techniques.
Future directions
There is a current lack of consensus on the radiographic definitions of global and focal pincer morphology. The crossover sign may be seen in both dysplasia (29) and global pincer deformities with some degree of acetabular retroversion (6). Additionally, the relative position of the acetabular fossa to the pelvis may not be indicative of acetabular coverage. One study detected no difference in the LCE angle or acetabular index between hips with and without coxa profunda (30). Future research is needed to improve our understanding of the complex 3-dimensional morphology of acetabular overcoverage, and apply this knowledge to the operating room setting. The lowest recommended limit for anterolateral rim reduction during focal pincer resection is generally a LCEA of 20° (31). However, the amount of surgical correction that should be achieved for the treatment of global overcoverage is not known. A recent CT-based analysis of asymptomatic patients reported a normal CEA of 31°, which offers some idea as to an acceptable target for correction (32). However, there is likely an individualized LCEA value that is needed to maintain proper hip health, with an associated interplay between parameters of acetabular morphology (e.g., coverage, depth, version) and spinopelvic orientation, all of which mutually influence the impact of dynamic loading of the joint. Future directions will define the ideal candidate and the surgical strategies needed to achieve optimal success.
Conclusions
The clinical relevance of this study is that patients with global pincer-type FAI who are managed with arthroscopic surgery may expect significant short-term improvement in pain and function. While the degree of clinical improvement appears to be of lower magnitude and survivorship compared to patients with focal overcoverage, this type of osseous deformity is still correctable with arthroscopic treatment by the experienced surgeon. High quality studies are needed to better ascertain the ideal indications and methods of achieving successful outcomes.

Full table
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “Future Perspectives in Hip Preservation and Arthroscopy”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.01.05). The series “Future Perspectives in Hip Preservation and Arthroscopy” was commissioned by the editorial office without any funding or sponsorship. RPC served as the unpaid Guest Editor of the series. ORA served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Joint from Aug 2017 to Jul 2019. ORA reports that he is a member of the Speakers bureau for Conmed. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003;112-20. [PubMed]
- Clohisy JC, Baca G, Beaulé PE, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med 2013;41:1348-56. [Crossref] [PubMed]
- Larson CM. Arthroscopic management of pincer-type impingement. Sports Med Arthrosc Rev 2010;18:100-7. [Crossref] [PubMed]
- Liechti EF, Ferguson SJ, Tannast M. Protrusio acetabuli: joint loading with severe pincer impingement and its theoretical implications for surgical therapy. J Orthop Res 2015;33:106-13. [Crossref] [PubMed]
- Verburg A, Elzenga P. Intertrochanteric valgization osteotomy for treatment of primary protrusion of the acetabulum (Otto-Chrobak pelvis). Arch Chir Neerl 1978;30:207-15. [PubMed]
- Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol 2007;188:1540-52. [Crossref] [PubMed]
- Steppacher SD, Lerch TD, Gharanizadeh K, et al. Size and shape of the lunate surface in different types of pincer impingement: theoretical implications for surgical therapy. Osteoarthritis Cartilage 2014;22:951-8. [Crossref] [PubMed]
- Hooper JC, Jones EW. Primary protrusion of the acetabulum. J Bone Joint Surg Br 1971;53:23-9. [Crossref] [PubMed]
- McBride MT, Muldoon MP, Santore RF, et al. Protrusio acetabuli: diagnosis and treatment. J Am Acad Orthop Surg 2001;9:79-88. [Crossref] [PubMed]
- Leunig M, Nho SJ, Turchetto L, et al. Protrusio acetabuli: new insights and experience with joint preservation. Clin Orthop Relat Res 2009;467:2241-50. [Crossref] [PubMed]
- Hanke MS, Steppacher SD, Zurmühle CA, et al. Hips With Protrusio Acetabuli Are at Increased Risk for Failure After Femoroacetabular Impingement Surgery: A 10-year Followup. Clin Orthop Relat Res 2016;474:2168-80. [Crossref] [PubMed]
- Botser IB, Smith TW Jr, Nasser R, et al. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy 2011;27:270-8. [Crossref] [PubMed]
- Matsuda DK, Carlisle JC, Arthurs SC, et al. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy 2011;27:252-69. [Crossref] [PubMed]
- Matsuda DK, Gupta N, Hanami D. Hip arthroscopy for challenging deformities: global pincer femoroacetabular impingement. Arthrosc Tech 2014;3:e197-204. [Crossref] [PubMed]
- Kay J, de Sa D, Memon M, et al. Examining the Role of Perioperative Nerve Blocks in Hip Arthroscopy: A Systematic Review. Arthroscopy 2016;32:704-15.e1. [Crossref] [PubMed]
- Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [Crossref] [PubMed]
- Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003;73:712-6. [Crossref] [PubMed]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. [Crossref] [PubMed]
- Chandrasekaran S, Darwish N, Chaharbakhshi EO, et al. Minimum 2-Year Outcomes of Hip Arthroscopic Surgery in Patients With Acetabular Overcoverage and Profunda Acetabulae Compared With Matched Controls With Normal Acetabular Coverage. Am J Sports Med 2017;45:2483-92. [Crossref] [PubMed]
- Matsuda DK, Gupta N, Burchette RJ, et al. Arthroscopic surgery for global versus focal pincer femoroacetabular impingement: are the outcomes different? J Hip Preserv Surg 2015;2:42-50. [Crossref] [PubMed]
- Sanders TL, Reardon P, Levy BA, et al. Arthroscopic treatment of global pincer-type femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc 2017;25:31-5. [Crossref] [PubMed]
- Safran MR, Epstein NP. Arthroscopic management of protrusio acetabuli. Arthroscopy 2013;29:1777-82. [Crossref] [PubMed]
- Matsuda DK. Protrusio acetabuli: contraindication or indication for hip arthroscopy? And the case for arthroscopic treatment of global pincer impingement. Arthroscopy 2012;28:882-8. [Crossref] [PubMed]
- Gupta A, Redmond JM, Stake CE, et al. Does Primary Hip Arthroscopy Result in Improved Clinical Outcomes?: 2-Year Clinical Follow-up on a Mixed Group of 738 Consecutive Primary Hip Arthroscopies Performed at a High-Volume Referral Center. Am J Sports Med 2016;44:74-82. [Crossref] [PubMed]
- Philippon MJ, Briggs KK, Yen YM, et al. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br 2009;91:16-23. [Crossref] [PubMed]
- Sansone M, Ahldén M, Jonasson P, et al. Good Results After Hip Arthroscopy for Femoroacetabular Impingement in Top-Level Athletes. Orthop J Sports Med 2015;3:2325967115569691 [Crossref] [PubMed]
- Kemp JL, MacDonald D, Collins NJ, et al. Hip arthroscopy in the setting of hip osteoarthritis: systematic review of outcomes and progression to hip arthroplasty. Clin Orthop Relat Res 2015;473:1055-73. [Crossref] [PubMed]
- Nwachukwu BU, Rebolledo BJ, McCormick F, et al. Arthroscopic Versus Open Treatment of Femoroacetabular Impingement: A Systematic Review of Medium- to Long-Term Outcomes. Am J Sports Med 2016;44:1062-8. [Crossref] [PubMed]
- Troelsen A, Rømer L, Jacobsen S, et al. Cranial acetabular retroversion is common in developmental dysplasia of the hip as assessed by the weight bearing position. Acta Orthop 2010;81:436-41. [Crossref] [PubMed]
- Anderson LA, Kapron AL, Aoki SK, et al. Coxa profunda: is the deep acetabulum overcovered? Clin Orthop Relat Res 2012;470:3375-82. [Crossref] [PubMed]
- Espinosa N, Beck M, Rothenfluh DA, et al. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. Surgical technique. J Bone Joint Surg Am 2007;89:36-53. [Crossref] [PubMed]
- Larson CM, Moreau-Gaudry A, Kelly BT, et al. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res 2015;473:1247-54. [Crossref] [PubMed]
Cite this article as: Coughlin RP, Memon M, Kay J, Simunovic N, Duong A, Ayeni OR. Outcomes after arthroscopic surgery for femoroacetabular impingement with global pincer: a systematic review. Ann Joint 2018;3:14.