
Acute dislocation of the patella: should these patients be operated on more often?
Background
First-time lateral patellar dislocation is a common orthopaedic injury with a high incidence in the general population with a mean of 42 per 100,000 person-years, and particularly in the young female patient aged 10–17 (108/100,000) (1). Patients who are skeletally immature at the time of the first patellar dislocation have a high rate of recurrent patellar instability with an increment of the redislocation rate with time (2). Moreover, 17% of patients will develop a patellofemoral osteoarthritis (PFOA) 20 years following initial dislocation (2). Sanders et al. (3) have demonstrated that osteochondral injury, recurrent patellar instability, and trochlear dysplasia are associated with the development of PFOA. Therefore, we are faced with a frequent lesion, not self-limited, with potential long-term complications such as anterior knee pain, decrease in the activity level, recurrent dislocation and PFOA, the last being a serious problem with a poor solution in the young patient. The orthopaedic surgeon should be aware of both, the high risk of recurrent dislocation and the risk to develop a PFOA when deciding on the treatment. It is therefore necessary to find the best treatment to avoid these possible outcomes.
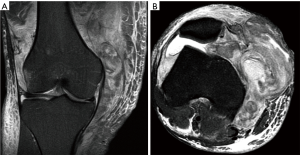
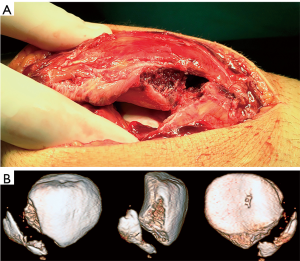
Typically the first-time lateral patellar dislocation is treated conservatively, except in some very specific cases that we will discuss later. In cases with an acute osteochondral fracture of the trochlea and/or patella that requires surgical treatment (refixation), the tear of the medial patellofemoral ligament (MPFL) will be repaired or reconstructed at the same time. Furthermore, in cases with a non-reducible lateral patellar dislocation with rotation as well as in cases with a substantial disruption of the medial patellar stabilizers, MPFL reconstruction would be indicated in the acute phase (Figure 1). Lastly, in those rare cases with a large and displaced bone avulsion fracture of the MPFL, surgical treatment would also be indicated (Figure 2). Controversy remains for the treatment of the rest of the cases and this will be the object of our paper.
Our work hypothesis is that the first acute lateral patellar dislocation should be treated surgically more often. To answer the question we ask ourselves in this review article, we are going to follow four different strategies. First we are going to review the literature published about this subject: conservative versus surgical treatment. Some randomized clinical trials (RCT) already analyze this alternative and given the fact that a RCT is the type of study with the highest scientific evidence, we are going to prioritize them but still do a critical reading, which is one of the basic tools of Evidence Based Medicine’s (EBM) methodology. Not all the published papers, including those published in high impact factor journals, are quality papers, RCT included. Therefore, all the papers should be analyzed thoroughly in a critical way. For our analysis we are going to focus on the design of the paper and the data provided. We will also perform a critical analysis of systematic reviews with the meta-analyses included, because the quality of a systematic review depends not only on the level of evidence of the papers chosen for the revision but also on the quality of the review. The second strategy to answer the question we ask ourselves in this paper is to critically analyze the studies that examine the probability of recurrence after a first lateral patellar dislocation based on predictive models. The third strategy will be to analyze the goals the patient has. Lastly we are going to analyze the cost-effectiveness economic models. Our goal is to determine which patients with a first episode of lateral patellar dislocation will be candidates for a surgical treatment and which will not.
It is terrifying to read John Ioannidis, from Stanford University, when he states regarding medical literature that: “false report probability is likely to exceed 50% for the whole literature” (4) or “currently, many published research findings are false or exaggerated, and an estimated 85% of research resources are wasted” (5). For this reason, we must be very critical when analyzing published studies, and the ones published on the subject we are reviewing are obviously not an exception. The goal of critical analysis is to avoid mistaken conclusions and this is also the final objective of our paper.
Decision based on critical analysis of the medical literature where conservative and surgical treatments are compared
There are several studies in the medical literature that analyze surgical versus conservative treatment for the first-time lateral patellar dislocation (6-16). In some of them, the reported patellar dislocation recurrence rates were lower in the surgical treatment group (10,11,13,15,16). However, other authors reported no difference in recurrence rates with operative or non-operative treatment (6-9,12,14). In most of the studies, the functional result is similar in both types of treatment (6-9,11,12,14,16). That is, surgical treatment does not improve the long-term outcomes. Interestingly, Regalado et al. (16) reported an increment of the redislocation rate with time in both types of treatment in adolescents. At 3 years, patients in the operative group had a redislocation rate of 0% versus 35% for the non-operative group (16). At 6 years of follow-up, the surgical group had a redislocation rate of 33% versus 73% for the non-surgical group (16). Palmu et al. (9), in patients younger than sixteen years of age, reported a similar dislocation recurrence rate of 71% for the non-operative group at the 14-year follow-up but the recurrence rate in the operative group was 67%. These figures would force us to take cautiously the recurrence rates in the studies carried out in the short term. We can conclude that at long-term, surgical stabilization does not reduce the rates of redislocation nor does it produce better subjective functional outcomes. According to Palmu et al. (9) the only significant predictor factor for recurrence was a positive family history of patellar instability.
If we analyze in detail the above mentioned studies we can draw several conclusions: (I) the follow-up times are very heterogeneous, so that the recurrence rates are not comparable; (II) the ages of the patients are not comparable in all the studies; (III) the small number of patients in the studies is a limiting factor that could lead to non-detection of statistically significant differences between the groups; (IV) the conservative treatment protocol is not the same in all studies; and (V) the types of surgical treatment are also different (realignment surgery, MPFL repair and MPFL reconstruction). Therefore, it is difficult to draw conclusions when doing systematic reviews with meta-analysis using these studies.
Erickson et al. (17) conducted a systematic review of the literature in 2015 to identify meta-analyses comparing non-operative and operative treatment of patellar dislocations. Meta-analysis quality and level of evidence were assessed. Patients treated operatively had a 24% rate of redislocations, whereas patients treated non-operatively had a 34.6% rate of redislocations (17). No differences in functional outcome scores were seen between both groups. Two out of four meta-analysis had low Oxman-Guyatt scores (<4), which indicates major flaws (17). Thus, according to the best available evidence, operative treatment of the first-time patellar dislocations may result in a lower rate of recurrence of dislocations than non-operative treatment but does not improve functional outcome scores. Therefore, they conclude that the scientific evidence to recommend surgical treatment is low.
When critically analyzing any of the previously mentioned studies we must check if the two groups that we are going to compare are really homogeneous. If they are not, the results are not going to be valid. We will now critically analyze the study by Bitar et al. (13). It is a RCT (level I of evidence) where results after a first lateral patellar dislocation treated with an MPFL reconstruction are compared with the results after a conservative treatment. The authors conclude that the results after a surgical treatment are better than with a conservative treatment after a 2-year follow-up. They observed a high percentage of recurrences in the conservative group (35%) while in the surgical group there were no cases of recurrence. To evaluate function the authors use the Kujala score that is significantly lower in the conservative treatment group (70.8) than in the surgical group (88.9). The authors conclude that the results of surgical treatment far exceed those of non-surgical treatment. However, when thoroughly analyzing the design of this study several questions come to mind. The information on randomization is unclear and therefore there is a risk of selection bias. Moreover, the allocation concealment is also unclear. All of this is important because if randomization is not adequate, the magnification of the effect of the intervention can be increased by 41% (18). If the randomization is not clear, the effect of the intervention can be increased by 30% (18). Furthermore, the absence of hiding the assigning sequence, can by itself magnify the effect of intervention by 21% (19). Moreover, there is a high risk of bias related to lack of blinding. We must note that if there is no double blind the effect of the intervention can be increased by 17% (18). What is more, if we thoroughly analyze the data they provide we can ask ourselves even more questions. Regarding the presence of predisposing factors according to each group, in the non-operative group there were 75% of knees with trochlear bump versus 50% in the reconstruction group. This is very important because trochlear dysplasia is an important risk factor for patellar dislocation recurrence (20,21). If we consider any predisposing factor for patellar instability the percentage in the non-operative group was of 95% vs. 66% in the reconstruction group. We are in fact comparing two groups that are not comparable. Therefore, results cannot be compared either and we must question the results of this study. Moreover, this paper has a duplicate publication (15). This paper was published in 2012 in the American Journal of Sports Medicine (13) and in 2015 in the Brazilian Journal of Orthopaedic Surgery (15). Duplicate publications are a serious problem because they deny other authors the chance to publish their work because of limited journal space. Another problem with duplicate publications is that they can lead to magnifying the results of one of the therapeutic options when a systematic review with meta-analysis is carried out.
After a critical revision of the medical literature that compares conservative treatment results to surgical treatment results in a first-time lateral patellar dislocation (6-16), we can conclude that current evidence is not conclusive to recommend one treatment over the other. The quality of the evidence is very low. More studies with the current accepted design quality criteria and with long term results, preferably multicentric trials in order to have a larger number of cases, are necessary. This type of study, today, does not exist. Therefore, we must try to find other reasons to defend a surgical treatment rather than a conservative treatment.
Decision based on predictive model analysis and pathoanatomy
One reason that could make us decide between the surgical treatment and the conservative treatment is the recurrence risk seen with conservative treatment. The key question is: Can recurrent instability be predicted after a first-time patellar dislocation? The idea would be to identify those risk factors that can predict conservative treatment failure. We believe it would be interesting to analyze recurrent dislocation predictive models after a first episode of lateral patellar dislocation treated conservatively. Following this criterion, patients with a high recurrence risk would be candidates for a surgical treatment after the first lateral patellar dislocation.
Nowadays in medicine, it is important to be able to predict future outcomes of treatments. In the past, it was based on the orthopaedic surgeon’s experience. Currently, it has been replaced by predictive model analysis, historically used in many business segments and that currently is an important tool in making decisions in orthopaedic surgery. Predictive models, “statistical tools that predict a clinical outcome based on at least two points of patient data”, can assist in the decision-making process aimed at achieving better clinical outcomes, as well as reducing costs (22).
Lewallen et al. (23) in 2013 analyzed what factors predict a lateral patellar dislocation recurrence in pediatric patients and adolescents with a mean age of 15 years (ranging from 9–18 years). They found that success with conservative treatment after a first-time patellar lateral dislocation was 62%, and that almost half of the patients with recurrent lateral patellar dislocation require surgical treatment. However, in skeletally immature patients (open physis) with trochlear dysplasia conservative treatment was successful in only 31% of the cases. Trochlear dysplasia is therefore a risk factor for recurrence of patellar dislocation. The greatest risk of recurrence of dislocation occurs in skeletally immature patients with trochlear dysplasia. The combination of the two factors (trochlear dysplasia and skeletal immaturity) conferred a 69% risk at 5 years (23). The results of this study are in agreement with those of Askenberger et al. (24) who found that trochlear dysplasia is the main anatomic patellar instability risk factor in the skeletally immature children for a primary lateral patellar dislocation.
Sillanpää et al. (25) observed that lateral patellar dislocation recurrence was also related to the MPFL tear site after the first dislocation. An MPFL femoral avulsion was associated with a higher probability of recurrence. For this reason, they suggest considering the MPFL tear site when deciding on the treatment for a primary traumatic patellar dislocation. MPFL injury location and pattern can be assessed by MRI (Figure 1).
Jaquith and Parikh (26) performed a study in children and adolescents in order to predict the recurrence of patellar dislocation after a first episode of dislocation. They analyzed four risk factors: trochlear dysplasia, history of contralateral dislocation, skeletal immaturity and a Caton-Deschamps index greater than 1.45. The recurrence rate with no associated risk factor was 13.8%. However, when one or more risk factors were present the recurrence rate increased considerably. When there was one risk factor present the recurrence rate was 30.1%, with two factors it was 53.6%, with three factors it was 74.8%, and with four it was 88.4%. However, this study is retrospective and therefore other factors such as hyperlaxity, lower limb malalignment or MPFL tear pattern were not included in the predictive model.
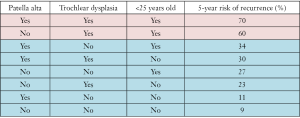
Lewallen et al. (27) in 2015 analyzed the lateral patellar dislocation recurrence risk after one lateral dislocation in all the ages of patients with this type of problem, not just in children and adolescents like Jaquith and Parikh (26). In Table I you can see the 5-year risk of recurrence based on the associated risk factors. In the first two assumptions (see Figure 3) the authors recommend surgical treatment after one episode of lateral patellar dislocation because the recurrence rate is unacceptably high. In the last 6 cases (see Figure 3) surgical treatment is not recommended as a first line of treatment.
Finally, Christensen et al. (28) have found that female patients under eighteen at the time of the first dislocation, trochlear dysplasia, elevated TT-TG distance, and patella alta were at risk for recurrence.
To summarize, the pathoanatomy and the predictive models can help us estimate the dislocation recurrence risk after a first episode treated conservatively. This approach can help us with the decision-making for the optimal treatment for a patient with a first-time lateral patellar dislocation.
Decision based on patient’s goals—return to sports at a pre-injury level
When deciding on the best treatment for any injury, not only must we consider the best evidence available and/or anatomopathological factors, but also the patient’s goals. Among those goals is the return to sports at a pre-injury level. Sport in the current society is so important that the United Nations has declared them a human right: “Sport and play are human rights that must be respected and enforced worldwide”. Practicing sports will demand more from the knee than a sedentary activity, therefore the joint’s stability must be more perfect.
The return to sports in adolescents after first-time patellar dislocations has not been well studied. Oliva et al. (29) found that in adolescent athletes with continued patellar instability after initial non-operative treatment, only 9 out of 24 (37.5%) returned to their pre-injury level of activity. Regalado et al. (16) in 2014 found that 80% of the adolescent patients treated surgically after a first-time lateral patellar dislocation achieve an excellent result regarding the return to sports at a pre-injury level. This percentage was only 47% for patients treated conservatively. These studies suggest that for athletic adolescents, surgery increases the probability of a return to sports compared with the conservative treatment. However, Sillanpää et al. (11) found that 72% of young adult patients with a mean age of 20 (ranging 19–22 years of age) with a first-time lateral patellar dislocation treated surgically returned to sports in comparison with 68% of those treated conservatively.
Economic decision model
The only study published that analyzes the decision-making in an economic model is the one by Nwachukwu et al. (30) in 2017. The authors analyze the cost-utility of three different ways of addressing an acute first-time patellar dislocation in adolescents: (I) non-surgical treatment; (II) non-surgical treatment at first, but if an episode of dislocation is repeated again the patient is operated on; and (III) surgical treatment at first. In their analysis, the authors detail both the direct and indirect costs of each therapeutic strategy. Direct costs included direct medical costs: cost of surgery and physical therapy. Indirect costs were calculated from lost productivity associated with caregiver (parental) work absenteeism. Effectiveness was expressed in quality-adjusted life years (QALYs). The authors showed that both immediate surgical treatment and delayed surgery are cost-effective treatment options. Nevertheless, with a perspective of 10 years, immediate surgery provides the most QALY gains and therefore it would be the most cost effective treatment. These findings could have implications for therapeutic decision-making when we see a patient with a first episode of patellar dislocation.
Conclusions
Based on the data we have analyzed, the answer to the question we ask ourselves in this paper is yes. Primary patellar dislocations should be operated on more often after the first dislocation. We have to think critically and to keep an open mind towards new things.
The role of surgery for first-time traumatic patellar dislocations is emerging as a reasonable treatment strategy. In highly active patients under 25 years of age with a pathoanatomy predisposing to recurrent dislocation (trochlear dysplasia associated or not with patella alta) surgical treatment could be considered as a first line of treatment in the first-time patellar dislocation because the recurrence risk is unacceptably high. This recommendation is based on recurrence predictive models after a first-time patella dislocation and in cost effectiveness economic models. Moreover, we must incorporate individual circumstances and preferences (patient’s goals such as sports) into the decision protocols.
Obviously we need high quality clinical trials describing anatomical abnormalities and MPFL tear site, ideally multicentric ones, which compare surgical and conservative treatments after a first-time lateral patellar dislocation to definitely answer the question we ask ourselves in this paper.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “The Patellofemoral Joint”. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.03.10).The series “The Patellofemoral Joint” was commissioned by the editorial office without any funding or sponsorship. VSA served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gravesen KS, Kallemose T, Blønd L, et al. High incidence of acute and recurrent patellar dislocations: a retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg Sports Traumatol Arthrosc 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Sanders TL, Pareek A, Hewett TE, et al. High rate of recurrent patellar dislocation in skeletally immature patients: a long-term population-based study. Knee Surg Sports Traumatol Arthrosc 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Sanders TL, Pareek A, Johnson NR, et al. Patellofemoral Arthritis After Lateral Patellar Dislocation: A Matched Population-Based Analysis. Am J Sports Med 2017;45:1012-7. [Crossref] [PubMed]
- Szucs D, Ioannidis JP. Empirical assessment of published effect sizes and power in the recent cognitive neuroscience and psychology literature. PLoS Biol 2017;15:e2000797 [Crossref] [PubMed]
- Ioannidis JP. How to make more published research true. PLoS Med 2014;11:e1001747 [Crossref] [PubMed]
- Nikku R, Nietosvaara Y, Kallio PE, et al. Operative versus closed treatment of primary dislocation of the patella. Similar 2-year results in 125 randomized patients. Acta Orthop Scand 1997;68:419-23. [Crossref] [PubMed]
- Buchner M, Baudendistel B, Sabo D, et al. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med 2005;15:62-6. [Crossref] [PubMed]
- Christiansen SE, Jakobsen BW, Lund B, et al. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy 2008;24:881-7. [Crossref] [PubMed]
- Palmu S, Kallio PE, Donell ST, et al. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am 2008;90:463-70. [Crossref] [PubMed]
- Camanho GL, Viegas Ade C, Bitar AC, et al. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy 2009;25:620-5. [Crossref] [PubMed]
- Sillanpää PJ, Mattila VM, Mäenpää H, et al. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation. A prospective randomized study. J Bone Joint Surg Am 2009;91:263-73. [Crossref] [PubMed]
- Apostolovic M, Vukomanovic B, Slavkovic N, et al. Acute patellar dislocation in adolescents: operative versus nonoperative treatment. Int Orthop 2011;35:1483-7. [Crossref] [PubMed]
- Bitar AC, Demange MK, D'Elia CO, et al. Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med 2012;40:114-22. [Crossref] [PubMed]
- Petri M, Liodakis E, Hofmeister M, et al. Operative vs conservative treatment of traumatic patellar dislocation: results of a prospective randomized controlled clinical trial. Arch Orthop Trauma Surg 2013;133:209-13. [Crossref] [PubMed]
- Bitar AC, D'Elia CO, Demange MK, et al. Randomized prospective study on traumatic patellar dislocation: conservative treatment versus reconstruction of the medial patellofemoral ligament using the patellar tendon, with a minimum of two years of follow-up. Rev Bras Ortop 2015;46:675-83. [Crossref] [PubMed]
- Regalado G, Lintula H, Kokki H, et al. Six-year outcome after non-surgical versus surgical treatment of acute primary patellar dislocation in adolescents: a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 2016;24:6-11. [Crossref] [PubMed]
- Erickson BJ, Mascarenhas R, Sayegh ET, et al. Does Operative Treatment of First-Time Patellar Dislocations Lead to Increased Patellofemoral Stability? A Systematic Review of Overlapping Meta-analyses. Arthroscopy 2015;31:1207-15. [Crossref] [PubMed]
- Schulz KF, Chalmers I, Hayes RJ, et al. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-12. [Crossref] [PubMed]
- Pildal J, Hróbjartsson A, Jørgensen KJ, et al. Impact of allocation concealment on conclusions drawn from meta-analyses of randomized trials. Int J Epidemiol 2007;36:847-57. [Crossref] [PubMed]
- Wagner D, Pfalzer F, Hingelbaum S, et al. The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc 2013;21:318-24. [Crossref] [PubMed]
- Nelitz M, Theile M, Dornacher D, et al. Analysis of failed surgery for patellar instability in children with open growth plates. Knee Surg Sports Traumatol Arthrosc 2012;20:822-8. [Crossref] [PubMed]
- Vogenberg FR. Predictive and Prognostic Models: Implications for Healthcare Decision-Making in a Modern Recession. Am Health Drug Benefits 2009;2:218-22. [PubMed]
- Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 2013;41:575-81. [Crossref] [PubMed]
- Askenberger M, Janarv PM, Finnbogason T, et al. Morphology and Anatomic Patellar Instability Risk Factors in First-Time Traumatic Lateral Patellar Dislocations: A Prospective Magnetic Resonance Imaging Study in Skeletally Immature Children. Am J Sports Med 2017;45:50-8. [Crossref] [PubMed]
- Sillanpää PJ, Peltola E, Mattila VM, et al. Femoral avulsion of the medial patellofemoral ligament after primary traumatic patellar dislocation predicts subsequent instability in men: a mean 7-year nonoperative follow-up study. Am J Sports Med 2009;37:1513-21. [Crossref] [PubMed]
- Jaquith BP, Parikh SN. Predictors of Recurrent Patellar Instability in Children and Adolescents After First-time Dislocation. J Pediatr Orthop 2017;37:484-90. [Crossref] [PubMed]
- Lewallen L, McIntosh A, Dahm D. First-time Patellofemoral Dislocation: Risk Factors for Recurrent Instability. J Knee Surg 2015;28:303-9. [Crossref] [PubMed]
- Christensen TC, Sanders TL, Pareek A, et al. Risk Factors and Time to Recurrent Ipsilateral and Contralateral Patellar Dislocations. Am J Sports Med 2017;45:2105-10. [Crossref] [PubMed]
- Oliva F, Ronga M, Longo UG, et al. The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med 2009;37:1814-20. [Crossref] [PubMed]
- Nwachukwu BU, So C, Schairer WW, et al. Economic Decision Model for First-Time Traumatic Patellar Dislocations in Adolescents. Am J Sports Med 2017;45:2267-75. [Crossref] [PubMed]
Cite this article as: Sanchis-Alfonso V, Montesinos-Berry E. Acute dislocation of the patella: should these patients be operated on more often? Ann Joint 2018;3:20.


