Evaluation of anterior knee pain patient: clinical and radiological assessment including psychological factors
Introduction
Anterior knee pain (AKP) is one of the most common reasons for consultation due to knee pathology among teenagers and young adults (1). A careful clinical history and physical evaluation along with imaging studies are crucial to arriving at an accurate diagnosis, which will be the cornerstone for developing an appropriate therapeutic program.
It is also important to assess the psychological state in patients with AKP. Numerous misconceptions and clichés still exist with regard to the disorder. One of the false beliefs is that the psychological profile of the patient might explain his or her pain. This belief arises from the fact that many patients with AKP have disabling pain and significant disability, but the physical signs and radiological findings are unremarkable. Nevertheless, psychological factors are not the responsible for the pain, although they may modulate it (2,3). Moreover, it has been shown that young female adults with long-standing AKP demonstrated impaired conditioned pain modulation (4). That is to say, AKP might have an important central component that needs to be studied so as to understand its extent and the therapeutic implications. Interestingly, psychological factors might underlie persistent unexplained pain and poor function after a correct conservative or surgical treatment.
The objective of this review is to analyze how patients with AKP should be assessed during consultation. The whole picture for each patient must be considered in order to identify all potentially modifiable factors so as to personalize treatment and obtains the best results possible.
Clinical history—pearls and tools
The main symptom of patients with AKP is peripatellar and/or retropatellar pain. The onset is usually insidious and without trauma, although there is usually an associated overload factor that may explain the pain. The identification of activities that provoke pain is crucial to the success of treatment; therefore, they should be reflected in the clinical history. Usually, the pain is aggravated by activities such as climbing and descending stairs, squatting, using the clutch when driving a vehicle with manual transmission (left AKP), wearing high-heeled shoes, and sitting with prolonged knee flexion (“movie or theatre sign”). In general, the patient cannot localize a specific area of pain with a finger. In most of the cases, he or she sweeps his or her finger along an area over the anterior aspect of the knee. In a few cases, the pain may be popliteal. Pain diagrams, or drawings on which patients locate the zone of knee pain, could be useful.
AKP is often described as dull with episodes of sharp pain. A Visual Analogue Scale (VAS) can be used to quantify the pain. It is a sensitive outcome measure for AKP, with a difference of 2 cm being considered clinically relevant (5). In addition, the VAS allows quantitative evaluation of the response to treatment. In patients with disproportionate pain, in time or degree, that has a sudden onset after knee injury or surgery, complex regional pain syndrome (CRPS) should be considered. Severe and disproportionate pain is an indicator of CRPS, which is classified as neuropathic pain, which is particularly challenging to deal with. Several questionnaires have been published for screening of neuropathic pain: the Douleur Neuropathique 4 scale (DN4) (6), the Leeds Assessment of Neuropathic Symptoms and Signs (LANSS) pain scale (7), and the self-completed LANSS (S-LANSS) (8). The sensitivity and specificity of the DN4 is around 95% and 97% and those of the LANSS pain scale are around 80% and 100%, respectively (9). Although there is no validated method to classify pain types in patients with AKP, we advise the use of the DN4 (9).
Aside from pain, other symptoms of AKP are a giving-way sensation and crepitus. Determine if the pain is associated with a lateral patellar instability is essential because both the treatment and the prognosis are very different in patients with AKP due to patellar instability compared with those without patellar instability. Crepitus is common, but it is clinically irrelevant in most cases. Symptoms in both knees are frequent, and one knee may be affected more than the other over time.
Moreover, patients with AKP present disability to a great or lesser degree. Self-administered scales such as the International Knee Documentation Committee evaluation (IKDC), the Kujala test, and the Tegner activity scale are useful for quantifying the disability. It is also important to know the patient’s activity level prior to the treatment and what he or she wants to achieve through treatment in order to offer realistic goals.
In patients with AKP, the incidence of anxiety, depression, kinesiophobia, and catastrophization is high (2,3,10). Even in cases with clear structural findings, psychological factors must be considered because they will moderate pain sensation as well as impairment. Moreover, they could affect the return to normal life. Thus, recognizing and quantifying the presence of these psychological factors are important to gain a complete view of the patient and to plan the best treatment. Self-administered screening tests for anxiety and depression (Hospital Anxiety and Depression Scale) (11), catastrophizing (Pain Catastrophizing Scale) (12), and kinesiophobia (Tampa Scale for Kinesiophobia) (13) should be incorporated into the clinical history in all cases.
Finally, among the clinical history antecedents, surgical interventions in the painful knee must be considered. One of the causes of disabling AKP after surgery is iatrogenic medial patellar instability (IMPI) that is secondary to excessive lateral retinacular release (10). Inappropriate physiotherapy could also be responsible for iatrogenic AKP. Therefore, it is essential that the patient describe exercises that are being done with the physiotherapist or in the gym.
Physical examination
The first objective of a physical examination is to pinpoint the painful area and try to reproduce the pain with physical exploration maneuvers. The location of the pain is important because it can reveal which structure is injured. Tenderness over the lateral retinaculum is a frequent finding. Lateral retinaculum tightness can be assessed with the patellar glide test. To determine if AKP has its source in the articular surface, the axial patellar compression test is used. Moreover, the sustained knee flexion test allows ruling out pain due to an increment in intraosseous patellar pressure (14). The inferior pole of the patella should be palpated in all cases because pain is very frequently located in this area. Hoffa’s test should also be performed because Hoffa’s fat pad can be a source of disabling AKP (15). Pain improvement after an infiltration with local anesthesia of the painful area or after unloading the area with functional taping provides evidence for the origin of pain (10).
When dealing with AKP, the most challenging issue is probably identifying the neuropathic subset. Several tools can help to identify neuropathic pain, which is distinct from nociceptive pain. The clinical examination remains the gold standard. A patient with CRPS presents with skin changes such as erythema and edema around the anterior aspect of the knee, with an allodynic (pain due to a stimulus that does not provoke pain normally) or a hyperalgesic (heightened response to a stimulus that is usually painful) pain response to any palpation on the anterior aspect of the knee, with patellar mobility restriction. The pain is not located in a specific nerve territory. Hyperalgesia can be proved by reduced pressure pain thresholds (PPTs) with pressure algometry on the patella (16). PPTs have been shown to normalize after successful treatment in adolescent females with AKP (17). Identification of these cases is important to evaluate clinical prognosis and recovery. However, pressure algometry should be used to quantify the pain at baseline and to monitor improvement of hyperalgesia with the treatment, rather than as a diagnostic method, because there is no specific value that serves as a threshold value for hyperalgesia.
Unilateral AKP can be due to the loss of full knee extension. Even small degrees of extension loss can cause AKP. Therefore, evaluating the passive range of knee mobility is crucial for all AKP patients.
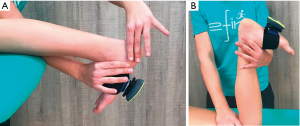
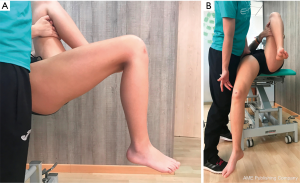
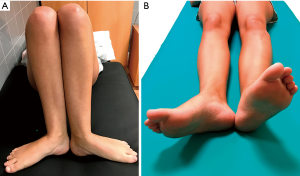
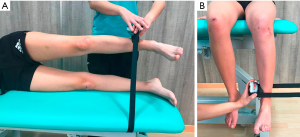
Patients with AKP present less flexibility of the anterior hip structures, quadriceps, iliotibial band, gastrocnemius, soleus, and hamstrings muscles compared to those without AKP (1,18), although only a shortened quadriceps muscle has shown to predict AKP development (19). Therefore, identifying the flexibility of all these structures is mandatory in order to restore it (Figures 1-4). All flexibility tests can be measured with different reproducible and precise tools like standard goniometer or digital inclinometer.


Baker et al. (20) showed that patients with AKP have abnormal proprioception of the knee. Thus, proprioception should be evaluated in these patients. Reproduction of active or passive joint position can be used to evaluate proprioception. For active joint position sense, both non-weight-bearing and weight-bearing tests can be sued. Proprioception has to be evaluated at a minimum of four angles of knee flexion.
If the patient has had previous knee surgery, existing scars should be evaluated. Tinel’s sign must be performed to detect neuromas that could be a source of iatrogenic AKP. If IMPI is suspected the Fulkerson relocation test is useful because it will reproduce the symptomatology (21).
It is mandatory to examine the entire lower limb
Most orthopedic surgeons are focused only on examining the knee when they see a patient with AKP in the office. This approach is a great mistake. There are other important etiological factors for AKP development distant from the knee. Therefore, an evaluation of skeletal mal-alignment in the three planes (coronal, transversal, and sagittal) is crucial. Moreover, examination of the hip is very important because alterations in this anatomical region can be responsible for the knee pain.
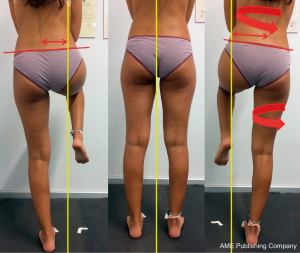
The patient should remain standing, barefoot, with their feet together. From the front, skeletal malalignment in the coronal plane (valgus/varus alignment), the patella orientation (neutral, convergent, or divergent), the morphology of the forefeet (pronatus, hallux valgus), and quadriceps and abdominal muscles volume are noted. In some patients a squinting patella with an apparent varus (miserable malalignment) is observed (Figures 5,6). From the back, a pelvic tilt, a varus or valgus alignment of the knee, a varus or valgus alignment of the calcaneus, and muscular volume of gastrocnemius, isquiosural, and gluteus muscles can be assessed. Finally, the anterior or posterior pelvic tilt, genu recurvatum, or flexum of the knees can be assessed from the side.

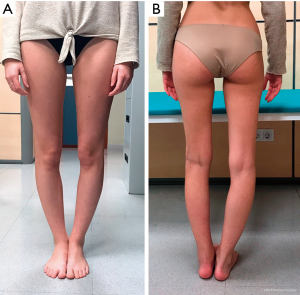
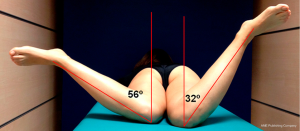
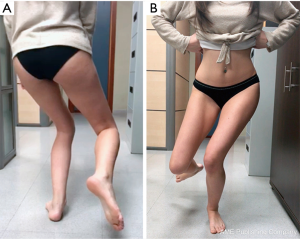
A clear relation exists between external tibial torsion and AKP (22). Excessive external tibial torsion can be isolated (Figure 7) or secondary to an excessive femoral anteversion. Isolated external tibial rotation can reduce the contact area and increase patellofemoral joint (PFJ) stress (23). However, isolated internal tibial rotation has little impact on the PFJ contact area and pressure (23). Excessive internal femoral torsion is also related to AKP. During weight bearing, internal rotation of the femur underneath the patella contributes to lateral patellar tilt and displacement (24). Internal femoral rotation has been associated with a reduced PFJ contact area and a patellar cartilage overload at 15° and 45° knee flexion (25). The increase in femoral anteversion, which is clearly related to AKP, is evidenced by an internal rotation of the hip greater than external rotation. For evaluation of the rotations of the hip, the patient lies in the prone decubitus position. When hip internal rotation is greater than 50°, abnormal and excessive femoral anteversion is generally present, resulting in the presence of squinting patellae (Figure 8). However, we can also see squinting patellae in cases with external tibial torsion without femoral anteversion. Finally, squinting patellae can also be a consequence of internal tibial rotation secondary to a pronated foot.
An alteration of the kinematics of the hip that appears as a result of hip musculature weakness (hip abductor and external rotator muscles) can contribute to the development of AKP (26). Therefore, hip muscle strength must be assessed in order to address muscle imbalances. Traditional manual muscle testing or a handheld dynamometer could be used depending on the availability (Figure 9).
In a previous preliminary study, we observed that an association may exist between Cam femoroacetabular impingement (FAI) and AKP (27). Therefore, evaluation of Cam FAI should be performed during the physical examination of AKP patients, especially when the pain continues after appropriate conservative treatment. In this case AKP is secondary to a functional femoral external rotation as a defense mechanism to prevent hip pain.
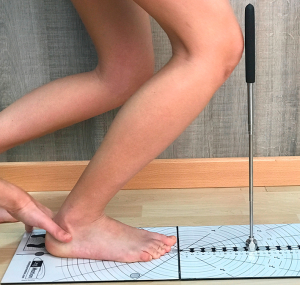
Finally, examination of the feet is important because pronated feet play an important role in the genesis of AKP. A functional hallux limitus could be another predisposing factor for AKP (28). Functional hallux limitus can be demonstrated by a loss of dorsal flexion of the first metatarsophalangeal joint with the ankle in dorsal flexion. Limited ankle dorsiflexion range of motion has been linked with AKP, and it has also been related to altered kinematics of the knee, implying that this impairment may be involved in the pathogenesis of AKP. Therefore, ankle dorsiflexion should be evaluated in all AKP patients (Figure 10) (29).
Functional tests—examine for altered/dysfunctional body movement patterns
The current trend in evaluating a patient with AKP is to use functional tests that simulate activities that the patient performs during living activities rather than apply conventional patellar tests. The final objective is to detect faulty body movement patterns in order to retrain them.
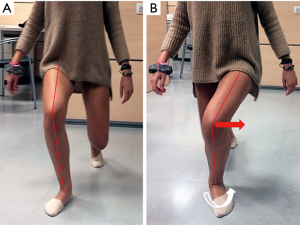
The first functional activity that should be evaluated is the gait since it is a common activity. During normal gait, the knee flexes 5° at the moment of heel strike and then continues to flex up to 10° to 15° (30). Afterward, the knee begins to extend until reaching full knee extension before the heel lifts (30). In AKP patients some functional impairment is apparent during gait, and AKP patients are frequently found to arrive at heel strike with the knee completely extended. In some cases, the gait evaluation reveals external rotation of the affected lower limb which is apparent through analysis of the foot progression angle (Figure 11). If nothing relevant is found during normal walking, the patient is asked to walk with long steps. The exaggerated movement will amplify subtle alterations of the gait such as femur adduction, internal hip rotation, and contralateral pelvic drop that may predispose the patient to developing AKP (Figure 12).

AKP patients have poor control of limb alignment while undertaking unilateral limb loading tests. The single leg squat is the most commonly used functional test to demonstrate the mechanics of the lower limb in AKP patients (Figure 13). This test allows detection of different movement strategies according to the proximal control of the patient. Another functional test for evaluating the lower-limb biomechanics is the one-leg stance (Figure 14), which permits evaluation of pelvi-femoral stability. Going down stairs is also a frequent and problematic action in patients with AKP; therefore, the forward down test (Figure 15) is also very useful when the patient can perform it. To perform this test well, a patient needs good balance and good control of the quadriceps eccentric phase. However, some patients have no pain in daily living activities, and they only feel knee pain when they exercise or participate in sports. In those cases, high-intensity functional testing, such as the tuck jump test (Figure 16), is useful (31).


Imaging
AKP is basically a clinical diagnosis. The only objective of imaging studies is to quantify the pathology when appropriate and rule out other knee conditions that could simulate patellofemoral pathology.
A standing whole-limb anteroposterior view radiograph to evaluate limb alignment in the coronal plane, a true lateral view to measure recurvatum or flexion contracture, and axial X-rays to evaluate patellofemoral mal-tracking should be obtained for all patients with AKP. These X-rays are the first step for imaging. In cases in which IMPI is suspected, stress axial radiography is mandatory to identify and quantify medial patellar instability (32). The difference between the displacement of both sides carries more importance than the absolute amount of displacement.
When patient response to conservative treatment is not adequate, other imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) are indicated.
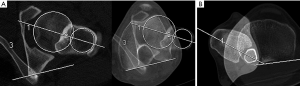
CT allows the measurement of knee parameters such as the tibial tubercle-trochlear groove distance (TT-TG), which is widely used to indicate and plan distal realignment surgeries. However, the value of the TT-TG distance continues to be a controversial issue. Some recent studies have shown that MRI may underestimate the TT-TG distance compared with CT (33,34). Therefore, the values of the TT-TG distance determined by CT cannot be extrapolated to those determined by MRI. The TT-TG distance is also influenced by multiple other factors. Tibial torsion, knee joint rotation, and small changes in femoral alignment and axial CT scan orientation have a significant effect on TT-TG measurement (35-37). In addition, the TT-TG distance can vary depending on the slices selected and the landmarks of the distal femur and tibial tuberosity retained by the radiologist (38,39). Moreover, it has shown that not all patients with a pathological TT-TG distance (i.e., >20 mm) have lateralization of the tibial tubercle (33,35,40). The tibial tubercle-posterior cruciate ligament (TT-PCL) distance has been recently introduced as a measurement not influenced by the rotation of the knee or the shape of the trochlea (35). The TT-PCL distance measures true lateralization of the tibial tubercle. Another recently described measurement, the TT-TG index, allows correlation of the distance with individual joint size (41). These new methods for determining the tibial tubercle position could facilitate the therapeutic approach. However, no pathological distance or index should be interpreted in isolation. Caution should be taken if the imaging technique including patient positioning and measurement method are not standardized. Clinical correlation is mandatory in all cases.
When a torsional abnormality is observed clinically, it must be quantified by means of CT (Figure 17). Three-dimensional CT (3D-CT) could be useful in patients with AKP after medial patellofemoral ligament (MPFL) reconstruction to detect femoral tunnel malposition.
MRI is useful for evaluating cartilage lesions and detecting intraosseous edema, or soft tissue impingement. Imaging findings such as lateral displacement of the patella are frequently seen in asymptomatic patients. It is also very common to detect patellofemoral chondropathies with MRI, but most are asymptomatic. For this reason, the therapeutic indication should be based on the correlation between clinical and imaging findings.
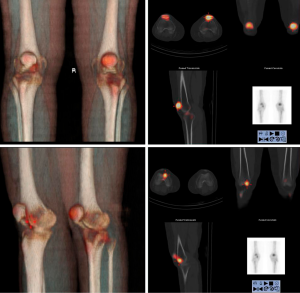
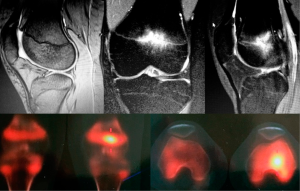
Single-photon emission CT-CT (SPECT-CT) provides information about structure and bone metabolism (Figure 18). It reveals the metabolic and geographic pattern of bone homeostasis, which is the normal osseous metabolic status of the joint. Näslund et al. (42) found that nearly 50% of AKP patients show scintigraphically diffuse bone uptake in one or more compartments of the knee. Not only has a relationship been shown between scintigraphic hyper-uptake and pain, but it has also been observed that the pain intensity and greater uptake are positively correlated (43,44). Ro du et al. (45) have shown that a higher degree of scintigraphic uptake in the PFJ in patients with chronic AKP, particularly in the patella, is associated with a poorer response to conservative management. Furthermore, an association has been documented between restoration to a normal bone scan and pain resolution after conservative treatment (43). SPECT-CT can also be helpful in cases of difficult diagnosis (Figure 19) and in selected cases such as workers’ compensation patients.
Currently, the subjectivity of pain can be captured by functional MRI (fMRI). fMRI has identified many brain pain centers that work together as a network. This “pain neuromatrix” can account for the multidimensional experience of pain (46) (Figure 20).

Conclusions
Most orthopedic surgeons focused only on examining the knee when they see a patient with AKP in the office. This approach is a great mistake because other important etiological factors distant from the knee can be responsible for the pain. Therefore, the entire lower extremity should be examined. AKP is basically a clinical diagnosis, with imaging studies used to confirm the clinical impression. The AKP patient is experiencing chronic pain, and therefore, the evaluation should include psychological factors, which are important in patients with chronic pain. Addressing the whole patient helps to identify potentially modifiable factors so an appropriate therapeutic program can be developed to achieve the best outcomes.
Acknowledgments
The authors acknowledge Antonio Darder, MD, for providing us figure 19.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “The Patellofemoral Joint”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.03.15). The series “The Patellofemoral Joint” was commissioned by the editorial office without any funding or sponsorship. VSA served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sanchis-Alfonso V, McConnell J, Monllau JC, et al. Diagnosis and treatment of anterior knee pain. JISAKOS 2016;1:161-73. [Crossref]
- Domenech J, Sanchis-Alfonso V, Lopez L, et al. Influence of kinesiophobia and catastrophizing on pain and disability in anterior knee pain patients. Knee Surg Sports Traumatol Arthrosc 2013;21:1562-8. [Crossref] [PubMed]
- Doménech J, Sanchis-Alfonso V, Espejo B. Changes in catastrophizing and kinesiophobia are predictive of changes in disability and pain after treatment in patients with anterior knee pain. Knee Surg Sports Traumatol Arthrosc 2014;22:2295-300. [Crossref] [PubMed]
- Rathleff MS, Petersen KK, Arendt-Nielsen L, et al. Impaired Conditioned Pain Modulation in Young Female Adults with Long-Standing Patellofemoral Pain: A Single Blinded Cross-Sectional Study. Pain Med 2016;17:980-8. [PubMed]
- Crossley KM, Bennell KL, Cowan SM, et al. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil 2004;85:815-22. [Crossref] [PubMed]
- Bouhassira D, Attal N, Alchaar H, et al. Comparison of pain syndromes associated with nervous or somatic lesions anddevelopment of a new neuropathic pain diagnostic questionnaire (DN4). Pain 2005;114:29-36. [Crossref] [PubMed]
- Bennett M. The LANSS Pain Scale: the Leeds assessment of neuropathic symptoms and signs. Pain 2001;92:147-57. [Crossref] [PubMed]
- Bennett MI, Smith BH, Torrance N, et al. The S-LANSS score for identifying pain of predominantly neuropathic origin: validation for use in clinical and postal research. J Pain 2005;6:149-58. [Crossref] [PubMed]
- Hamdan A, Luna JD, Del Pozo E, et al. Diagnostic accuracy of two questionnaires for the detection of neuropathic pain in the Spanish population. Eur J Pain 2014;18:101-9. [Crossref] [PubMed]
- Sanchis-Alfonso V, Merchant AC. Iatrogenic Medial Patellar Instability: An Avoidable Injury. Arthroscopy 2015;31:1628-32. [Crossref] [PubMed]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. [Crossref] [PubMed]
- Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess 1995;7:524-32. [Crossref]
- Kori KS, Miller RP, Todd DD. Kinesiophobia: a new view of chronic pain behavior. Pain Mang 1990;3:35-43.
- Hejgaard N, Arnoldi CC. Osteotomy of the patella in the patellofemoral pain syndrome. The significance of increased intraosseous pressure during sustained knee flexion. Int Orthop 1984;8:189-94. [Crossref] [PubMed]
- Dragoo JL, Johnson C, McConnell J. Evaluation and treatment of disorders of the infrapatellar fat pad. Sports Med 2012;42:51-67. [Crossref] [PubMed]
- Rathleff MS, Roos EM, Olesen JL, et al. Lower mechanical pressure pain thresholds in female adolescents with patellofemoral pain syndrome. J Orthop Sports Phys Ther 2013;43:414-21. [Crossref] [PubMed]
- Rathleff MS, Roos EM, Olesen JL, et al. Self-reported Recovery is Associated With Improvement in Localized Hyperalgesia Among Adolescent Females With Patellofemoral Pain: Results From a Cluster Randomized Trial. Clin J Pain 2016;32:428-34. [Crossref] [PubMed]
- Piva SR, Goodnite EA, Childs JD. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther 2005;35:793-801. [Crossref] [PubMed]
- Witvrouw E, Lysens R, Bellemans J, et al. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med 2000;28:480-9. [Crossref] [PubMed]
- Baker V, Bennell K, Stillman B, et al. Abnormal knee joint position sense in individuals with patellofemoral pain syndrome. J Orthop Res 2002;20:208-14. [Crossref] [PubMed]
- Fulkerson JP. A clinical test for medial patella tracking. Tech Orthop 1997;12:144. [Crossref]
- Teitge RA. Patellofemoral syndrome a paradigm for current surgical strategies. Orthop Clin North Am 2008;39:287-311. [Crossref] [PubMed]
- Lee TQ, Yang BY, Sandusky MD, et al. The effects of tibial rotation on the patellofemoral joint: assessment of the changes in in situ strain in the peripatellar retinaculum and the patellofemoral contact pressures and areas. J Rehabil Res Dev 2001;38:463-9. [PubMed]
- Powers CM, Ward SR, Fredericson M, et al. Patellofemoral kinematics during weight-bearing and non-weightbearing knee extension in persons with lateral subluxation of the patella: a preliminary study. J Orthop Sports Phys Ther 2003;33:677-85. [Crossref] [PubMed]
- Liao TC, Yang N, Ho KY, et al. Femur rotation increases patella cartilage stress in females with patellofemoral pain. Med Sci Sports Exerc 2015;47:1775-80. [Crossref] [PubMed]
- Khayambashi K, Mohammadkhani Z, Ghaznavi K, et al. The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: a randomized controlled trial. J Orthop Sports Phys Ther 2012;42:22-9. [Crossref] [PubMed]
- Sanchis-Alfonso V, Tey M, Monllau JC. A Novel Association between Femoroacetabular Impingement and Anterior Knee Pain. Pain Res Treat 2015;2015:937431.
- Vallotton J, Echeverri S. Clinical examination of the patellofemoral patient. In: Zaffagnini S, Dejour D, Arendt EA. editors. Patellofemoral Pain, Instability, and Arthritis. Springer Berlin Heidelberg, 2010:41-9.
- Rabin A, Portnoy S, Kozol Z. The Association of Ankle Dorsiflexion Range of Motion With Hip and Knee Kinematics During the Lateral Step-down Test. J Orthop Sports Phys Ther 2016;46:1002-9. [Crossref] [PubMed]
- Harris-Hayes M, Cornbleet S, Holtzman G. Movement system syndromes of the knee. In: Sahrmann S. Movement system impairment syndromes of the extremities, cervical and thoracic spines. St. Louis, Mo.: Elsevier/Mosby, 2011:354-406.
- Herrero-Herrero M, García-Massó X, Martínez-Corralo C, et al. Relationship between the practices of physical activity and quality of movement in adolescents: a screening tool using self-organizing maps. Phys Sportsmed 2017;45:271-9. [Crossref] [PubMed]
- Teitge RA, Faerber WW, Des Madryl P. Stress radiographs of the patellofemoral joint. J Bone Joint Surg Am 1996;78:193-203. [Crossref] [PubMed]
- Anley CM, Morris GV, Saithna A, et al. Defining the Role of the Tibial Tubercle-Trochlear Groove and Tibial Tubercle-Posterior Cruciate Ligament Distances in the Work-up of Patients With Patellofemoral Disorders. Am J Sports Med 2015;43:1348-53. [Crossref] [PubMed]
- Ho CP, James EW, Surowiec RK, et al. Systematic technique-dependent differences in CT versus MRI measurement of the tibial tubercle-trochlear groove distance. Am J Sports Med 2015;43:675-82. [Crossref] [PubMed]
- Seitlinger G, Scheurecker G, Högler R, et al. Tibial tubercle-posterior cruciate ligament distance: new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med 2012;40:1119-25. [Crossref] [PubMed]
- Yao L, Gai N, Boutin RD. Axial scan orientation and the tibial tubercle-trochlear groove distance: error analysis and correction. AJR Am J Roentgenol 2014;202:1291-6. [Crossref] [PubMed]
- Worden A, Kaar S, Owen J, et al. Radiographic and Anatomic Evaluation of Tibial Tubercle to Trochlear Groove Distance. J Knee Surg 2016;29:589-93. [Crossref] [PubMed]
- Lustig S, Servien E, Aït Si Selmi T, et al. Factors affecting reliability of TT-TG measurements before and after medialization: A CT-scan study. Rev Chir Orthop Reparatrice Appar Mot 2006;92:429-36. [Crossref] [PubMed]
- Yin L, Chen C, Duan X, et al. Influence of the image levels of distal femur on the measurement of tibial tubercle-trochlear groove distance-a comparative study. J Orthop Surg Res 2015;10:174. [Crossref] [PubMed]
- Heidenreich MJ, Camp CL, Dahm DL, et al. The contribution of the tibial tubercle to patellar instability: analysis of tibial tubercle-trochlear groove (TT-TG) and tibial tubercle-posterior cruciate ligament (TT-PCL) distances. Knee Surg Sports Traumatol Arthrosc 2017;25:2347-51. [Crossref] [PubMed]
- Hingelbaum S, Best R, Huth J, et al. The TT-TG Index: a new knee size adjusted measure method to determine the TT-TG distance. Knee Surg Sports Traumatol Arthrosc 2014;22:2388-95. [Crossref] [PubMed]
- Näslund JE, Odenbring S, Näslund UB, et al. Diffusely increased bone scintigraphic uptake in patellofemoral pain syndrome. Br J Sports Med 2005;39:162-5. [Crossref] [PubMed]
- Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res 2005;100-10. [Crossref] [PubMed]
- Draper CE, Fredericson M, Gold GE, et al. Patients with patellofemoral pain exhibit elevated bone metabolic activity at the patellofemoral joint. J Orthop Res 2012;30:209-13. [Crossref] [PubMed]
- Ro du H. Value of SPECT-CT Imaging for Middle-Aged Patients with Chronic Anterior Knee Pain. BMC Musculoskelet Disord 2015;16:169. [Crossref] [PubMed]
- Damasio AR, Grabowky TJ, Bechara A, et al. Subcortical and cortical brain activity during the feeling of self-generated emotions. Nat Neurosci 2000;3:1049-56. [Crossref] [PubMed]
Cite this article as: Sanchis-Alfonso V, Coloma-Saiz J, Herrero-Herrero M, Prades-Piñón J, Ramírez-Fuentes C. Evaluation of anterior knee pain patient: clinical and radiological assessment including psychological factors. Ann Joint 2018;3:26.