
Treating complications of operative management for patellofemoral pain
Background
Sokol and Wilson (1) define a surgical complication as “an undesirable and unintended result of an operation affecting the patient that occurs as a direct result of the operation”. Complications associated with surgical treatment can occur regardless of the quality of care or competence of the surgeon, resulting in increased hospital stays, readmissions, repeat surgeries, additional medical treatment, costs, and legal issues. Thus, limiting complications can improve quality of care.
Anterior knee pain (AKP) is a musculoskeletal condition often with a vague and typically multifactorial etiopathogenesis, having been involved factors such as the loss of homeostasis as well as functional, mechanical and structural alterations; all of these things lead the treatment to be complicated (2). A plethora of treatment options have been described with different levels of agreement. The great number of variables associated with AKP, most of which lack valid measurement tools, can explain this confusion. Moreover, there is a complete lack of studies that justify the variability of the different therapeutic approaches. Thus, a patient with AKP is an ideal candidate to undergo surgeries with little scientific basis. In fact, many treatments for AKP have no medical basis [e.g., intra-articular injections of PRP (Platelet-Rich-Plasma)]. Furthermore, many doctors do not follow standards of care, because they do not consider non-surgical treatments. Also, patients may push the orthopaedic surgeon to operate, because a previous conservative treatment, which many times is incomplete and inadequate, has failed. It may be difficult to convince these patients to start another physiotherapy treatment because many people believe that surgery is the panacea. This belief is particularly false in AKP surgery. Surgeons have the moral responsibility to do their best for their patients and to ensure that any proposed surgical procedure is appropriate and valid. All surgical procedures carry risks of complications; thus, it is important to prevent unnecessary surgeries.
According to the current literature, most patients with AKP must be treated non-surgically (3). In my experience, most surgeries for these patients are to solve complications from previous, poorly performed or badly indicated surgeries for AKP. Therefore, caution is necessary when recommending surgical treatment, particularly among “well-meaning, trigger-happy orthopaedic surgeons” educated in an exclusively structural, anatomical, and biomechanical view of this pathology. These surgeons operate on what magnetic resonance imaging (MRI) shows (i.e., patellar chondropathy, lateral patellar subluxation and/or patellar tilt). Operating based only on these findings is a big mistake. Surgeons must be careful when proposing a treatment based exclusively on the presence of structural anomalies. Indeed, the wrong algorithms based on the classic biomechanical or structural paradigm are the main causes of poor outcomes and complications of operative management of AKP (2,4,5). Finally, we must not forget an incorrect postoperative physical therapy that can lead to surgical failures and complications. In sum, the worst and most challenging cases of AKP occur secondary to a surgical procedure that was intended to correct structural anomalies, but such anomalies later were found not to be related to the patient’s symptomatology.
In patients for whom AKP is secondary to chronic lateral patellar instability, medial patellofemoral ligament (MPFL) reconstruction surgery often is performed (6). Lateral retinaculum (LR) release is a popular procedure associated with MPFL reconstruction. In a 2016 study of 6,190 patients, the most common procedure associated with patellar stabilization was LR release (43.7%) (7). However, LR release also may contribute to disabling iatrogenic AKP.
Non-specific complications of surgeries for treating AKP include infection, deep venous thrombosis, complex regional pain syndrome, compartment syndrome, and arthrofibrosis. This paper focuses on specific complications related to patellofemoral surgery performed to manage patellofemoral pain. The three most serious complications after surgery to eliminate AKP are iatrogenic medial patellar instability (IMPI) and multidirectional patellar instability, patella infera (or patella baja), and patellofemoral osteoarthritis (PFOA). The goals of this review paper are to provide best practices for avoiding complications of patellofemoral surgery, to give diagnostic advice for evaluating the failed patellofemoral surgery patient, and to present operative salvage procedures to treat these cases.
Iatrogenic medial patellar instability—multidirectional patellar instability
An important source of postsurgical AKP is IMPI, which frequently causes chronic and disabling AKP in addition to important psychological problems (8). In a previous study, we compared the psychological involvement in patients with typical AKP with that of patients with AKP secondary to IMPI. We observed that the latter group had higher rates of kinesiophobia (100% vs. 80%), catastrophizing (41% vs. 37%), anxiety (59% vs. 37%), and depression (24% vs. 11%) (8). Moreover, patients with IMPI have severely limited functional abilities, and many cannot work. Paradoxically, the pain and disability of IMPI is often much worse than the pain and disability the patient had before the surgery. The patient often feels the patella moving laterally, which can lead to an erroneous diagnosis of lateral patellar instability, which in turn leads to another unnecessary surgery to reconstruct the MPFL, which creates new complications and iatrogenesis.
The first step to diagnose a pathologic condition is to know its existence. IMPI is a missed epidemic with many undetected cases. Over-release of the LR with resection of the vastus lateralis tendon is the most important cause of IMPI (8-11). IMPI also results from poor patient selection: LR release in patients with trochlear dysplasia, patella alta, or hyperelasticity, or release of the LR in patients with patellar tilt without a tight LR (8,9,11). In sum, IMPI is a major complication of LR release. This iatrogenic condition could be prevented by avoiding the over-release of the LR and by selecting the surgical indication, only releasing a tight LR (8). Moreover, LR lengthening, which is an alternative to LR release, maintains lateral soft-tissue integrity and avoids IMPI (12).
Physical findings are crucial for diagnosis. The most important are pain and tenderness in the area of the defect of the LR, increment of passive medial patellar mobility in comparison with the normal knee, positive medial apprehension, and a positive gravity subluxation test (13). IMPI is a functional problem. Therefore, we can diagnose it by using provocative testing, such as the “Fulkerson relocation test” (14). Fulkerson relocation test involves pushing the patella medially with the knee extended, then flexing abruptly and letting go of the patella. If positive, the patient experiences the same feeling that he or she has habitually. All patients will experience significant pain relief with a “reverse” McConnell taping (8).
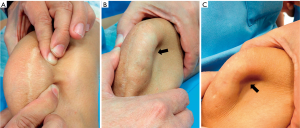
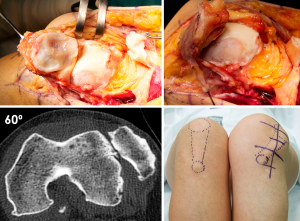
Concomitant lateral patellar instability associated with IMPI must always be ruled out. In these cases, we would be facing a multidirectional patellar instability (Figure 1). LR release is a surgical procedure that some orthopaedic surgeons perform in patients with lateral patellar instability (7). This approach can result in concomitant episodes of medial and lateral patellar subluxation or true dislocation (15). In a patient with multidirectional patellar instability we can see during physical examination a “sulcus sign” (Figure 1) similar to that of multidirectional shoulder instability.
The major problem at diagnosis is that the classical radiological studies for these patients are normal. Normal imaging tests paired with disproportionate pain can lead to an incorrect diagnosis that the patient’s condition is fundamentally psychiatric. The only way to diagnose and quantify medial patellar instability is through dynamic radiological studies, such as stress axial radiography (Figure 2) (16). In some cases, medial displacement of the patella can be observed even without applying a medial force to displace it, as occurs in medial patellar instability secondary to an over-release of the LR associated with an over-medialization of the tibial tuberosity (Figure 3).


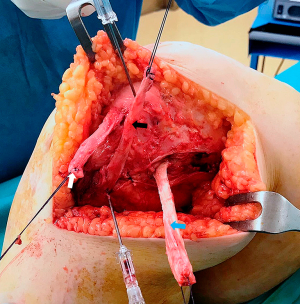
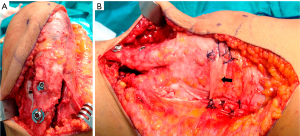
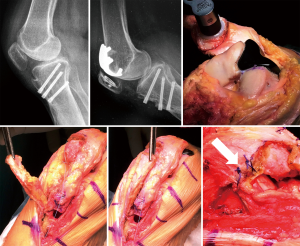
Surgical techniques to treat IMPI include direct repair of the LR, LR reconstruction, lateral patellofemoral ligament reconstruction, lateral patellotibial ligament reconstruction, and arthroscopic medial retinacular release (17). High patient satisfaction has been reported after surgery, with significant improvements in pain and functional stability (17). Andrish’s technique (i.e., reconstruction of the deep layer of the LR using the iliotibial band) is my preferred first line of treatment for these severely disabled patients (9). It is anatomic with relatively good results (9). However, this “salvage” procedure does not address the primary cause of pain that led the patient to have surgery, which may explain its 65% success rate (9). In severe cases of medial patellar instability, my advice is to reconstruct both the lateral patellotibial ligament (18) and the lateral patellofemoral ligament (19) (Figure 4). In cases of medial patellar instability secondary to an over-release of the LR associated with an over-medialization of the tibial tuberosity, a reconstruction of the deep layer of the LR associated with an anterolateral transfer of the tibial tubercle must be performed (Figures 5,6) (20). Saper and Shneider (21) described a surgical technique to treat episodes of both medial and lateral patellar subluxation after failed isolated LR release for patellar instability. Simultaneous medial and lateral patellofemoral ligament reconstructions provide good clinical outcomes in this subgroup of patients.

Patella infera
Another devastating complication after surgical treatment of AKP is patella infera, also called patella baja. This complication can provoke severe knee pain and severely restrict range of motion in the knee. Left untreated, it causes early PFOA (22). Weale et al. (23) have demonstrated that, for each millimeter of patellar tendon shortening, there is a 1-degree of loss of knee flexion. Patella infera is caused by an association of two factors. First, it often occurs in combination with arthrofibrosis following knee surgery, especially in the context of infrapatellar contracture syndrome. In some cases, it is secondary to distal realignment surgery, and in exceptional cases, a patella infera follows patellar tendon contracture after arthroscopic denervation of the inferior pole of the patella (Figure 7). Second, it occurs during painful post-operative rehabilitation with no active quadriceps contractions or in patients with paralysis of the quadriceps (Figure 8).

Surgery is indicated when the Caton-Deschamps ratio is less than or equal to 0.6 (24). Two surgical treatments have been described, lengthening of the patellar tendon or osteotomy of the tibial tuberosity, depending on the length of the patellar tendon (24-27). Figure 9 shows a patient with severe patella infera and visible PFOA who sought help for disabling AKP after distal realignment surgery. Because the length of the patellar tendon was normal, a patellofemoral arthroplasty associated with a tibial tubercle osteotomy to heighten the patella was performed. Figure 10 shows a similar case with a short patellar tendon. To heighten the patella in this case, a Z-plasty lengthening of the patellar tendon was performed. Another option for patellar tendon lengthening is a coronal tenotomy. This approach is feasible, because in patients with patella infera, the shortening of the tendon is always associated with a thickening of the same (Figure 7) (27).

Patellofemoral osteoarthritis
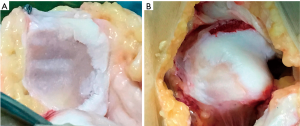
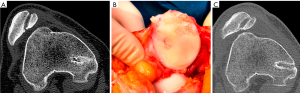
Another important complication after patellofemoral surgery to treat AKP in the young patient is symptomatic secondary diffuse patellofemoral articular damage (Figure 11). The problem with this type of lesion lies not in the lesion itself but in the age of the patients, who are too young for “metal and plastic.” Fresh allograft transplantation should be considered as a salvage treatment procedure in these patients (28-32). Before considering any resurfacing technique, the patellofemoral joint (PFJ) and the skeletal mal-alignment of the extremity must be optimized to obtain satisfactory results (33). A resurfacing technique is not a substitute for a patella realignment. In cases where the patellar tracking and skeletal mal-alignment of the extremity are correct, an isolated resurfacing technique can be performed (Figure 12). In any of these surgical resurfacing techniques, overstuffing of the PFJ should be avoided.
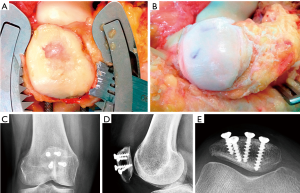
Patellofemoral chondropathy, or PFOA, could also be the result from inadequate MPFL reconstruction (34). A relatively common mistake in MPFL reconstruction surgery is to place the femoral attachment point excessively anterior, which provokes patellar instability and AKP (34). This pain is more severe if there is an associated severe trochlear dysplasia. These symptoms are due to a significant increase of the PFJ reaction force and pressure over the medial patellofemoral cartilage, which leads to painful PFOA. In these cases, resection of the previous graft and new MPFL reconstruction using an anatomic femoral attachment are mandatory. In cases with severe trochlear dysplasia, MPFL reconstruction associated with sulcus-deepening trochleoplasty should be considered (Figure 11). In these cases, pain and instability disappear after trochleoplasty even though the PFOA is left alone.
Discussion
According to the homeostasis theory, the joints are much more than mechanical structures; they are “living systems metabolically active” (35). The PFJ is no exception. The loss of both osseous and soft tissue homeostasis is more important than structural anomalies (i.e., chondropathy, patellar tilt, and patellar subluxation) in the genesis of AKP (35). It has been shown that the relation between AKP and these structural anomalies is poor, and their presence alone is not sufficient evidence to warrant surgical correction (2,4,5,35). Although the structural paradigm is not valid in most patients with AKP, it is valid in a subgroup of these patients (36,37). In some cases, intractable and disabling AKP is related to skeletal malalignment of the limbs in the coronal, sagittal, and transverse planes (37). Skeletal malalignment is not synonymous with patellofemoral malalignment (i.e., patellar tilt, patellar subluxation). Correcting these skeletal malalignments correlates with the disappearance of AKP. This biomechanical approach is compatible with the biological perspective.
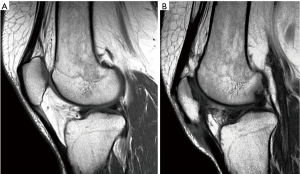
This paper highlights the importance of patellofemoral instability (IMPI and multidirectional patellar instability) in the pathogenesis of postsurgical AKP. Moreover, pain also relates to overload in the PFJ in a subset of patients with AKP. Good femoropatellar kinematics and congruence are more important than the presence of normal articular cartilage (38). Indeed, even patients with severe chondropathy of the PFJ can be asymptomatic (Figures 13,14). The question is whether articular cartilage is essential. In other words, it is necessary to replace the PFJ? Patellofemoral resurfacing techniques, including patellofemoral arthroplasty, are indicated only in select cases. An interesting surgical technique for treating severe AKP in a patient with a failed MPFL reconstruction surgery associated to a severe trochlear dysplasia and PFOA would be a trochleoplasty associated with MPFL reconstruction. The satisfactory outcomes of trochleoplasty result from increasing the space between the patella and the femoral trochlea, which unloads the PFJ. This approach produces a Maquet effect and suggests a relationship between AKP and patellofemoral overload. Moreover, in patients with intractable AKP and lateral/distal patellar softening, a short steep anteromedial tibial tuberosity osteotomy to unload the affected zone will provided pain relief in the majority of these patients (36). To summarize, any significant deviation in patellofemoral alignment should be corrected before considering cartilage procedures in the PFJ.
Conclusions
The results of conservative treatment for AKP can be frustrating. That does not mean that orthopedic surgeons should rush to perform a surgical treatment. Surgery is not a panacea. Indeed, a poorly indicated or poorly performed surgical treatment can be disastrous for the patient. Cautious is thus essential when determining the surgical indication. Orthopedic surgeons must never forget the principles of Hippocratic medicine: “Primum non nocere.” We must not cause harm or make an already bad situation much worse. By reducing the large number of unnecessary surgeries to treat AKP and by paying attention to technical details, we also can reduce considerably the number of surgical complications. Ideally, treating a complication should address the problem that led to the primary surgery and the damage caused by the failed surgical procedure.
Acknowledgments
The author acknowledges Joan Carles Monllau, MD, PhD for providing me the 9th & 10th illustrations.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “The Patellofemoral Joint”. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.03.09). The series “The Patellofemoral Joint” was commissioned by the editorial office without any funding or sponsorship. VSA served as the unpaid Guest Editor of the series. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sokol DK, Wilson J. What is a surgical complication? World J Surg 2008;32:942-4. [Crossref] [PubMed]
- Sanchis-Alfonso V. Anterior Knee Pain and Patellar Instability. London: Springer, 2011.
- Sanchis-Alfonso V, McConnell J, Monllau JC, et al. Diagnosis and treatment of anterior knee pain. J ISAKOS 2016;1:161-73. [Crossref]
- Sanchis-Alfonso V, Dye SF. How to Deal With Anterior Knee Pain in the Active Young Patient. Sports Health 2017;9:346-51. [Crossref] [PubMed]
- Post WR, Dye SF. Patellofemoral Pain: An Enigma Explained by Homeostasis and Common Sense. Am J Orthop (Belle Mead NJ) 2017;46:92-100. [PubMed]
- Sanchis-Alfonso V. Guidelines for medial patellofemoral ligament reconstruction in chronic lateral patellar instability. J Am Acad Orthop Surg 2014;22:175-82. [Crossref] [PubMed]
- Arshi A, Cohen JR, Wang JC, et al. Operative management of patellar instability in the United States: An evaluation of national practice patterns, surgical trends, and complications. Orthop J Sports Med 2016;4:2325967116662873 [Crossref] [PubMed]
- Sanchis-Alfonso V, Merchant AC. Iatrogenic Medial Patellar Instability: An Avoidable Injury. Arthroscopy 2015;31:1628-32. [Crossref] [PubMed]
- Sanchis-Alfonso V, Montesinos-Berry E, Monllau JC, et al. Results of isolated lateral retinacular reconstruction for iatrogenic medial patellar instability. Arthroscopy 2015;31:422-7. [Crossref] [PubMed]
- Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med 1988;16:383-8. [Crossref] [PubMed]
- Song GY, Hong L, Zhang H, et al. Iatrogenic medial patellar instability following lateral retinacular release of the knee joint. Knee Surg Sports Traumatol Arthrosc 2016;24:2825-30. [Crossref] [PubMed]
- Unal B, Hinckel BB, Sherman SL, et al. Comparison of Lateral Retinaculum Release and Lengthening in the Treatment of Patellofemoral Disorders. Am J Orthop (Belle Mead NJ) 2017;46:224-8. [PubMed]
- Nonweiler DE, DeLee JC. The diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am J Sports Med 1994;22:680-6. [Crossref] [PubMed]
- Fulkerson JP. A clinical test for medial patella tracking. Tech Orthop 1997;12:165-9. [Crossref]
- Miller PR, Klein RM, Teitge RA. Medial dislocation of the patella. Skeletal Radiol 1991;20:429-31. [Crossref] [PubMed]
- Teitge RA, Faerber WW, Des Madryl P, et al. Stress radiographs of the patellofemoral joint. J Bone Joint Surg Am 1996;78:193-203. [Crossref] [PubMed]
- Moatshe G, Cinque ME, Kruckeberg BM, et al. Medial Patellar Instability: A Systematic Review of the Literature of Outcomes After Surgical Treatment. Arthroscopy 2017;33:1587-93. [Crossref] [PubMed]
- Hughston JC, Flandry F, Brinker MR. Surgical correction of medial subluxation of the patella. Am J Sports Med 1996;24:486-91. [Crossref] [PubMed]
- Teitge RA, Torga Spak R. Lateral patellofemoral ligament reconstruction. Arthroscopy 2004;20:998-1002. [Crossref] [PubMed]
- Fulkerson JP. Anterolateralization of the tibial tubercle. Tech Orthop 1997;12:165-9. [Crossref]
- Saper MG, Shneider DA. Simultaneous medial and lateral patellofemoral ligament reconstruction for combined medial and lateral patellar subluxation. Arthrosc Tech 2014;3:e227-31. [Crossref] [PubMed]
- Caton J, Deschamps G, Chambat P, et al. Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot 1982;68:317-25. [PubMed]
- Weale AE, Murray DW, Newman JH, et al. The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br 1999;81:790-5. [Crossref] [PubMed]
- Guido W, Christian H, Elmar H, et al. Treatment of patella baja by a modified Z-plasty. Knee Surg Sports Traumatol Arthrosc 2016;24:2943-47. [Crossref] [PubMed]
- Drexler M, Dwyer T, Marmor M, et al. The treatment of acquired patella baja with proximalize the tibial tuberosity. Knee Surg Sports Traumatol Arthrosc 2013;21:2578-83. [Crossref] [PubMed]
- Dejour D, Levigne C, Dejour H. Postoperative low patella. Treatment by lengthening of the patellar tendon. Rev Chir Orthop Reparatrice Appar Mot 1995;81:286-95. [PubMed]
- Bruhin VF, Preiss S, Salzmann GM, et al. Frontal Tendon Lengthening Plasty for Treatment of Structural Patella Baja. Arthrosc Tech 2016;5:e1395-e1400. [Crossref] [PubMed]
- Torga Spak R, Teitge RA. Fresh osteochondral allografts for patellofemoral arthritis: long-term followup. Clin Orthop Relat Res 2006;193-200. [Crossref] [PubMed]
- Gracitelli GC, Meric G, Pulido PA, et al. Fresh osteochondral allograft transplantation for isolated patellar cartilage injury. Am J Sports Med 2015;43:879-84. [Crossref] [PubMed]
- Cameron JI, Pulido PA, McCauley JC, et al. Osteochondral Allograft Transplantation of the Femoral Trochlea. Am J Sports Med 2016;44:633-8. [Crossref] [PubMed]
- Gracitelli GC, Meric G, Briggs DT, et al. Fresh osteochondral allografts in the knee: comparison of primary transplantation versus transplantation after failure of previous subchondral marrow stimulation. Am J Sports Med 2015;43:885-91. [Crossref] [PubMed]
- Meric G, Gracitelli GC, Görtz S, et al. Fresh osteochondral allograft transplantation for bipolar reciprocal osteochondral lesions of the knee. Am J Sports Med 2015;43:709-14. [Crossref] [PubMed]
- Prince MR, King AH, Stuart MJ, et al. Treatment of Patellofemoral Cartilage Lesions in the Young, Active Patient. J Knee Surg 2015;28:285-95. [Crossref] [PubMed]
- Sanchis-Alfonso V, Montesinos-Berry E, Ramirez-Fuentes C, et al. Failed medial patellofemoral ligament reconstruction: Causes and surgical strategies. World J Orthop 2017;8:115-29. [Crossref] [PubMed]
- Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res 2005;100-10. [Crossref] [PubMed]
- Fulkerson JP. Why does distal patella articular softening happen? Orthopaedics Today Europe The Official Newspaper of EFORT 2015;18:53-6.
- Teitge RA. Osteotomy for Treatment of PF Instability, Anterior Knee Pain or PF Chondrosis due to Abnormal Skeletal Torsion. 2016 AAOS Annual Meeting, ICL 410.
- Blønd L, Donell S. Does the patellofemoral joint need articular cartilage? Knee Surg Sports Traumatol Arthrosc 2015;23:3461-3. [Crossref] [PubMed]
Cite this article as: Sanchis-Alfonso V. Treating complications of operative management for patellofemoral pain. Ann Joint 2018;3:27.


