
Different osteotomy solutions influence future total knee arthroplasty in patients with multiapical lower extremity deformities
Introduction
Malalignment of the mechanical axis of the lower limb and rotational deformity result in abnormal forces transmitted across the knee joint (1,2). This subsequently causes osteoarthritis, affecting the quality of life by inducing pain, triggering additional deformities, and limiting daily routine activities (3-7). Proximal tibial osteotomy, firstly described by Jackson et al. (8), represents a surgical technique for treating young individuals with lower limb varus malalignment. Corrective osteotomies for varus include: lateral closing-wedge osteotomy of the distal femur, medial opening-wedge osteotomy of the distal femur, medial opening-wedge osteotomy of the proximal tibia, lateral closing-wedge osteotomy of the proximal tibia, and combined osteotomy for cases with complex deformities (9-11). A successful osteotomy leads to complete alignment restoration, improved joint function, and alleviated pain. It may also delay the need for total knee arthroplasty (TKA) or even help avoid TKA (12,13). However, TKA remains necessary in cases with further knee degeneration. The ideal orthopedic osteotomy is to recover the original anatomy and mechanical axis of femur and tibia as far as possible. Generally, multi-level osteotomy is necessary for the severe deformity patients. However, the increase site of osteotomy, which means higher incidence of nonunion and longer recovery time, is not accepted by the patients. Thus, single-level osteotomy is usually used to recover the lower limb force line as a compromise method after communication with patients. But the tilt of tibia plateau would follow. Although many cases about lower limb deformity combined with osteoarthritis have been reported that mechanical axis deformity could be corrected partially by individualized osteotomy during arthroplasty of knee. It’s still unclear that how far such compromise would affect the knee arthroplasty in the future. Therefore, whether an anatomically perfect correction should be performed or the magnitude of correction compromised in view of potential future TKA remains an open question. In addition, it is not known which of single- and multi-level osteotomies is more beneficial. For the answers of these questions, we made a simulation of osteotomy plan on lower limb deformity patient and the subsequent TKA in this study.
Methods
A 25-year-old female from a healthy non-consanguineous couple, with no familial history, was admitted to our hospital with a chief complaint of severe varus deformity in both lower extremities. The deformity had progressed since the age of 2 years. A lateral thrust upon walking on both sides was revealed.
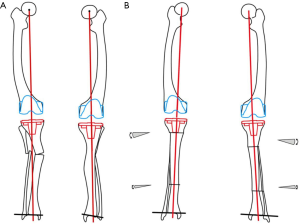
The study received approval from the Institutional Review Board. Informed consent was provided. Presurgical assessment comprised patient history collection and physical exams. A corrected mechanical axis was sketched on full-length radiographs as shown in Figure 1. The joint lines on the frontal and sagittal planes presented an orientation typical to mechanical and anatomic axes. The work by Paley (14) was used as a reference for nomenclature and standard values. A joint line can be traced to link the hip, knee, and ankle. The angle between this joint line and the mechanical or anatomic axis is termed joint orientation angle. Angles are named based on their axis of measure, mechanical (m) or anatomic (a); they may be determined medially (M), laterally (L), anteriorly (A), or posteriorly (P). An angle may be based on the proximal (P) or distal (D) joint orientation of the femur (F) or tibia (T). Examples are the mechanical lateral distal femoral angle (mLDFA), anatomic LDFA (aLDFA), and anatomic posterior proximal tibial angle (aPPTA) (Figure 1).
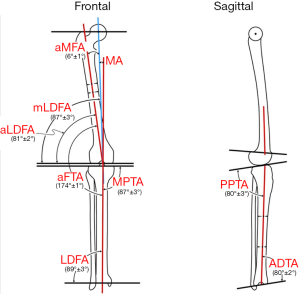
Joint orientation angles, such as medial proximal tibial angle (MPTA) and LDTA, were determined as proposed previously (15). Meanwhile, anteroposterior (AP) and lateral radiography of the tibia was performed for PPTA measurements.
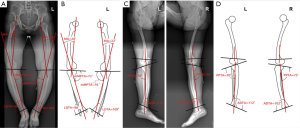
Frontal and sagittal plane deformities were measured on weight-bearing full-length radiographs (Figure 2). The physiological joint angles of the lower extremity were shown in Table 1.

Full table
Preoperative planning
Since the mLDFA and MPTA were abnormal, 87° (normal value) for the MPTA was used to derive the mechanical axis of the proximal tibia (PMA). We drew a line (anatomical axis of the distal tibia, DAA) from the midpoint of the tibial plafond parallel to the tibial shaft. LDTA was measured from the ankle’s plafond line to the latter line. Since LDTA was abnormal, 90° (normal value) was employed in orienting the mechanical axis of the distal tibia (DMA). The intersection between the PMA and DMA lines is termed center of rotation of angulation (CORA). The magnitude of angulation (Mag) is assessed between the proximal and distal axis lines. The intersection is lateral to the bone shaft (resolved apex CORA, with Mag values of 32° and 31° on the left and right sides, respectively; Figure 3A). Therefore, the current case represents a multi-apical angular deformity. A 3rd mechanical axis (green-colored, Figure 3B) was drawn as a representative of mid-diaphysis, and its intersection with the PMA and DMA lines was labeled as proximal and distal CORAs; Mag values of 21° and 11°, respectively, were found for the left side.

Single- or multi-level osteotomy could be used to correct multi-apical angular deformities. In single-level osteotomy, the PMA and DMA lines intersected laterally to the center of femoral and tibial shaft. The mechanical axis was realigned by osteotomy with 32° and 31° angular corrections around the resolved CORAs of left and right tibias, respectively (Figure 3C). Then, ankle and knee joint alignments regained their normal orientations, and the anatomic axis twisted. In multi-level osteotomy, the middle axis identified two CORAs on each side. The mechanical axis was realigned by two osteotomy procedures with 21° and 11° angular corrections, respectively, around the proximal and distal CORAs, on the left side, with 20.5° and 10° on the right, accordingly. The anatomic axes were realigned (Figure 3D).
Surgery and postoperative assessment
All surgical procedures were carried out by the same group. Multi-level osteotomy was not selected due to the theoretically higher incidence of nonunion. Closing wedge osteotomy was performed, which converged on the closing wedge CORA. Each osteotomy side was perpendicular to long bone’s long axis. Meanwhile, an oblique fibular osteotomy was performed in the midshaft by means of a micro-sagittal saw. Hydroxyapatite-coated half pins were used to stabilize the monolateral frame externally fixating the tibia. After surgery, the patient was followed up for 13 months until the most recent visit. Weight-bearing was allowed two weeks postoperatively. Supervised physical therapy targeting range of motion (ROM) values for the knee and ankle was administrated. Follow-up occurred every 2 months until frame removal. Then, the patient was required to return at 3, 6, and 12 months, respectively, for ROM assessment. Postoperative assessment of joint orientation angles and the mechanic/anatomic axis was performed by radiography.
Two-dimensional (2D) pre-TKA templating
2D pre-TKA templating was performed on an AP view weight-bearing full-length radiograph of the lower limbs. The templating of posterior-stabilized high-flex implant (NexGen, Zimmer, Warsaw, USA) was performed for pre-TKA planning. The simulated surgical specifications were as described previously (16).
Three-dimensional (3D) pre-TKA templating
DICOM data from multislice CT scan (Sensation 64, Siemens Medical Systems, Germany) from the hip to ankle were obtained and transferred to the planning workstation for 3D reconstruction. The operating windows comprised three multiplanar reformation (MPR) views (frontal, sagittal, and axial planes); all reformatted images could be edited and assessed at the same time. Digitally reconstructed radiographs (DRRs) were displayable in all directions.
A pre-TKA planning program allowed the surgeon to “navigate” the prosthetic components into the 3D space to the proper position, and the surgeon could dynamically change the component sizes. The three centers of reference (hip, knee, and ankle) were identifiable on the same acquisition. After volume reconstruction and the identification of mechanical axes, the pre-TKA plan determined the sizes and positions of various components according to general principles, beyond constitutional deformities. The femoral component was aligned orthogonally to the femoral mechanical axis on the frontal plane, supported by the anterolateral part of the cortical bone on the sagittal plane, and oriented along the surgical bi-epicondylar axis on the transverse plane (identified on CT scan by a line joining the bony prominence and sulcus on the medial epicondyle). The tibial component was aligned orthogonally to the mechanical axis of the tibia on the frontal plane, along the anatomic tibial angle on the sagittal plane as well as the medial third of the tibial tuberosity on the transverse plane. The surgical bi-epicondylar axis and Whiteside line were used as references for balancing the ligaments and patellar tracking.
Results
The appearance of lower extremities was improved. The average location of CORA was 17 cm from the knee joint orientation line on the left side, and 12 cm on the right. On assessment of deformity correction, the MPTA improved from 76° to 87° on the left side, and from 72° to 96° on the right (Figure 4A,B and Table 2). The mechanical lateral distal tibial angle (mLDTA) changed from 109° to 101° on the left side, and from 98° to 90° on the right (Figure 4A,B and Table 2).
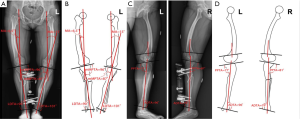
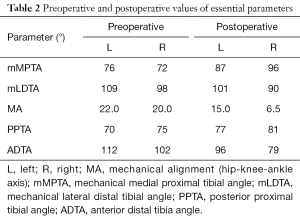
Full table
The mechanical alignments (MAs) on both sides were significantly improved after correction (Table 2). PPTA and anterior distal tibia angle (ADTA) got significantly corrected and approximated to the normal values, immediately after surgery or at the last visit (Figure 4C,D, Table 2). Bony union was observed for both sides at the last visit (Figure 5).

Full preoperative knee and ankle ROM values were maintained on both sides until last follow-up. Time from the primary surgery to full weight-bearing ability was 3 months. No pain or other complications, such as nerve injury, compartment syndrome, patella baja, osteomyelitis, delayed wound healing, pin site infection, and implant insufficiency, were observed.
The corresponding templates were used to size each side of the postoperative (actual single-level osteotomy) radiograph and simulated image of multi-level osteotomy (Figure 6). The depths of distal femoral and proximal tibial bone cuts were assessed parallel to the corresponding putative mechanical axes (Table 3). The appropriately sized components of the femoral and tibial sides were selected to allow covering of the resected surface without overhang (17) (Table 3).
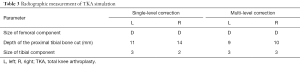
Full table
3D pre-TKA templating was performed on both sides, which were corrected by single-level osteotomy. After 3D reconstruction, the proximal cutting plane for the tibia with a 3° posterior angle is shown in Figure 7. The used implant sizes and a 3D anatomic model that includes bone surfaces topped by implants are depicted as well.
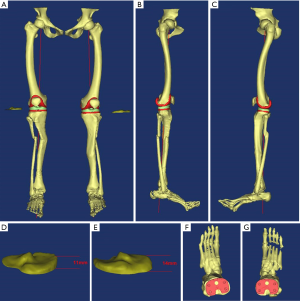
3D analysis showed that the distance from the tip of the medial tibial plateau to resection was 14 mm on the right side, with a compromised correction. This distance was 11 mm on the left side, accordingly. Attributed to angulation of tibial anatomical axis, an impingement of the tibial stem upon the proximal lateral tibial cortex would likely occur on the right side.
Discussion
Several patients present with knee osteoarthritis complicated with extra-articular deformity. Some have fracture sequelae, of which the femoral or tibial fracture extends beyond the knee’s capsuloligamentous envelope, healing in a poor position. Most studies preferred to associate prosthesis and osteotomy. Therapeutic strategies would be inconsistent in patients with knee osteoarthritis who received previous osteotomies for correction. Mechanical axis derangement resulting from a varus or valgus deformity in the lower extremity accelerates knee degeneration, with additional deformities (18-20). Correcting such deformities is critical and advocated for young adults. The current case could be treated by either uniapical or multiapical osteotomy. When uniapical osteotomy was selected, the mechanical axis was realigned with a 31°–32° angular correction around the resolved tibial CORA (Figure 2). All affected joint orientations regained their normal features. However, delayed union and nonunion should not be overlooked. Lateral closing wedge osteotomy was performed due to its potential of healing because of two diaphyseal areas placed side by side. Meanwhile, medial opening wedge techniques need transverse autografts or allografts. External fixation was used in the present case. Large angular corrections are generally unsuitable for medial distraction plate since nonunion may occur (21). Even so, the healing time was 11 months for the left side, and bony union was not complete on the right at the last follow-up, 13 months after operation. Choosing multi-level osteotomy also resulted in realigned mechanical axis. Whether the incidence of nonunion is increased in multi-level osteotomy remains unknown, though the risk of nonunion could be minimized by practicing metaphyseal osteotomies, in the region with best potential for bone union. Therefore, the formulation and implementation of the osteotomy scheme was also impeded. As the case mentioned above, deformity also occurred at femur. However, due to the delayed union after tibia osteotomy, the planed second stage femur osteotomy was not accepted by the patient. Simultaneously, while the tibia osteotomy for the right side, we increased the magnitude of correction to compensate the deviation of lower limb mechanical axis caused by femur deformity as much as possible. However, the coming tilt of tibia plateau would make it more difficult for the future TKA.
TKA due to degeneration is another major concern. Malalignment represents the dominant reason for failure, overloading the bone and ligaments, with subsequent bone loss, fractures, and ligament instability. For the tibia, restoring a more physiological movement and achieve even load distribution following TKA is feasible: in frontal alignment, the tibia should be placed to align its center with the mechanical tibial axis to the highest degree possible (17,22,23). Based on the theories above, the osteotomy thickness of tibial plateau need to be increased, so as to achieve the cutting plane being perpendicular to the mechanical axis. In the case, the depth of the proximal tibial bone cut of left side was 11 mm. On the right side, the osteotomy depth reached 14 mm because of the tilt of plateau. Due to the cone-like structure of the tibia, a larger thickness of the bone resection leads to a smaller area of the tibial platform, which requires smaller sized components. A smaller size tibial component was used on the left side and matching of the corresponding femur component was also limited.
The extension and flexion gap will therefore be out of balance. What’s more, the probability of ligament injury will get higher if the bone resection increases. Specifically, the collateral ligament on the vertex side gets loose, and the contralateral ligament needs releasing, but an equal ligament balance under the circumstances of both extension and flexion can be hardly achieved. It is believed that intra-articular compensatory osteotomy can only correct frontal deformity that <20° and <30° in the femur and the tibia, respectively, and a highly constrained knee is required as well (24). As we all know, posterior-stabilized knee implants require only slight ligament attenuation. In mildly attenuated, loose, or imbalanced medial collateral ligaments, constrained condylar knee implants represent the most efficient option (25,26). Meanwhile, rotating hinge knee prostheses should be preferably employed in more serious cases (27). For constrained condylar knee implants and hinge knee prostheses, the stem needed to be accommodated in the medullary cavity. However, the anatomic axis was zigzagged, which is more manifest for single-level osteotomy solutions and makes it difficult to implant prostheses. Even though there has been offset for stem in the current prosthesis, it’s still difficult to put it into the medullary cavity for these cases. For the reason of impingement of the stem upon the proximal lateral tibial cortex, hinge knees with tibial stem extensions, which are essential for the cases of ligament compromise impairment, cannot be used.
In summarized, we tried to identify various factors to be considered in the treatment of lower extremity deformity cases by the simulation of osteotomy plan on lower limb deformity and the subsequent TKA, and hoped the current treatment plan would not be regrettable in the future treatment of joint degeneration. Corrective osteotomy is not the end of the treatment for patients with multiapical lower limb deformities. With regard to the present case, we operated the abnormal anatomy of the bone to correct the mechanical axis. Apart from bone healing and alignment restoration, TKA due to future degeneration must be taken into serious consideration. Bone stock, bone healing, soft tissue balance, biomechanical force, joint motion, limb appearance, prosthesis adaption, are all concerned in this activity. A sufficient and excellent preoperative plan of osteotomy is necessary not only for achieving present correction of alignment, but also for achieving a successful TKA yet to come and avoiding potential complications. Limitations also existed in the study: (I) we only focused on tibia osteotomy without further femur osteotomy because of the patient’s choice; (II) no biomechanical analysis of muscle strength and ligament balance has been implemented; (III) though TKA simulation had been performed on bilateral lower limbs deformity with different magnitude of correction, the change of mechanical axis on coronal and sagittal plane were analyzed and the rotational deformity had not been concerned.
Acknowledgments
Funding: The study was funded by the Science and Technology Planning Project of Guangdong Province (grant number: 2014A020215009, 2014A020212060, 2013B051000024), and by the Science and Technology Planning Project of Guangzhou City, China (grant number: 201803010011).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.03.12). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by Sun Yat-sen Memorial Hopspital Ethics Committee (No. SYSEC-KY-KS-2018-013). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sharma L, Song J, Felson D T, et al. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 2001;286:188-95. [Crossref] [PubMed]
- Coventry MB. Upper tibial osteotomy for osteoarthritis. J Bone Joint Surg Am 1985;67:1136-40. [Crossref] [PubMed]
- Iorio R, Healy WL. Unicompartmental arthritis of the knee. J Bone Joint Surg Am 2003;85-A:1351-64. [Crossref] [PubMed]
- Cole B J, Harner CD. Degenerative arthritis of the knee in active patients: evaluation and management. J Am Acad Orthop Surg 1999;7:389-402. [Crossref] [PubMed]
- Hochberg MC, Altman RD, Brandt KD, et al. Guidelines for the medical management of osteoarthritis. Part II. Osteoarthritis of the knee. American College of Rheumatology. Arthritis Rheum 1995;38:1541-6. [Crossref] [PubMed]
- Grelsamer RP. Unicompartmental osteoarthrosis of the knee. J Bone Joint Surg Am 1995;77:278-92. [Crossref] [PubMed]
- Catagni MA, Guerreschi F, Ahmad TS, et al. Treatment of genu varum in medial compartment osteoarthritis of the knee using the Ilizarov method. Orthop Clin North Am 1994;25:509-14. [PubMed]
- Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br 1961;43-B:746-51. [Crossref] [PubMed]
- Dietrick TB, Bugbee WD. Distal Femoral Osteotomy Utilizing a Lateral Opening-Wedge Technique. Techniques in Knee Surgery 2005;4:186-92. [Crossref]
- Derek T, Cooke V. Osteotomy and osteoarthritis. Orthopedics 1999;22:281, 288.
- Healy WL, Anglen JO, Wasilewski SA, et al. Distal femoral varus osteotomy. J Bone Joint Surg Am 1988;70:102-9. [Crossref] [PubMed]
- Niemeyer P, Koestler W, Kaehny C, et al. Two-Year Results of Open-Wedge High Tibial Osteotomy with Fixation by Medial Plate Fixator for Medial Compartment Arthritis With Varus Malalignment of the Knee. Arthroscopy 2008;24:796-804. [Crossref] [PubMed]
- Agneskirchner JD, Hurschler C, Wrann CD, et al. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy 2007;23:852-61. [Crossref] [PubMed]
- Paley D, Herzenberg JE, Tetsworth K, et al. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994;25:425-65. [PubMed]
- Paley D. Principles of Deformity Correction. Springer-Verlag Berlin Heidelberg, 2002:688.
- Pietsch M, Djahani O, Hochegger M, et al. Patient-specific total knee arthroplasty: the importance of planning by the surgeon. Knee Surg Sports Traumatol Arthrosc 2013;21:2220-6. [Crossref] [PubMed]
- Scott WN. Insall & Scott Surgery of the Knee. 5th Edition. Churchill Livingstone, 2011:150-2
- Wright JM, Crockett HC, Slawski DP, et al. High tibial osteotomy. J Am Acad Orthop Surg 2005;13:279-89. [Crossref] [PubMed]
- Lee SC, Jung KA, Nam CH, et al. The short-term follow-up results of open wedge high tibial osteotomy with using an Aescula open wedge plate and an allogenic bone graft: the minimum 1-year follow-up results. Clin Orthop Surg 2010;2:47-54. [Crossref] [PubMed]
- Marti RK, Verhagen RA, Kerkhoffs GM, et al. Proximal tibial varus osteotomy. Indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am 2001;83-A:164-70. [Crossref] [PubMed]
- Koyonos L, Slenker N, Cohen S. Complications in brief: Osteotomy for lower extremity malalignment. Clin Orthop Relat Res 2012;470:3630-6. [Crossref] [PubMed]
- Hsu RW, Himeno S, Coventry MB, et al. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res 1990;215-27. [PubMed]
- Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 1987;69:745-9. [Crossref] [PubMed]
- Wang JW, Wang CJ. Total knee arthroplasty for arthritis of the knee with extra-articular deformity. J Bone Joint Surg Am 2002;84-A:1769-74. [Crossref] [PubMed]
- Hartford JM, Goodman SB, Schurman DJ, et al. Complex primary and revision total knee arthroplasty using the condylar constrained prosthesis: An average 5-year follow-up. J Arthroplasty 1998;13:380-7. [Crossref] [PubMed]
- Lachiewicz PF, Falatyn SP. Clinical and radiographic results of the Total Condylar III and Constrained Condylar total knee arthroplasty. J Arthroplasty 1996;11:916-22. [Crossref] [PubMed]
- Morgan H, Battista V, Leopold SS. Constraint in primary total knee arthroplasty. J Am Acad Orthop Surg 2005;13:515-24. [Crossref] [PubMed]
Cite this article as: Xu J, Zhang Y, Li D, Huang Y, Cai Z, Ma R. Different osteotomy solutions influence future total knee arthroplasty in patients with multiapical lower extremity deformities. Ann Joint 2018;3:30.


