Management of peri-prosthetic fractures around total hip arthroplasty: a contemporary review of surgical options
Introduction
There is a risk of intraoperative periprosthetic fracture during primary hip arthroplasty (1); however, more commonly this complication is seen post-operatively (2). It is anticipated that the incidence of periprosthetic fractures will increase with increasing numbers of total hip or knee arthroplasty performed and as the numbers of uncemented femoral stems increase (3). These injuries often occur in older patients with more significant co-morbidity and osteopenia (4). Management of these injuries is often resource intensive and can present significant socioeconomic challenges (1).
Periprosthetic fractures are challenging for the surgeon and medical team. Surgical management can be technically demanding (5). Historically non-operative management of the injuries such as long leg casting or traction has demonstrated unacceptably high rates of morbidity and mortality (6). Multiple techniques have been described to manage these complex injuries and may include internal fixation and/or revision of the in situ prosthesis. Whilst internal fixation may include locking plate, cable plating, orthogonal plating and the use of allograft or autograft, no consensus exists on the ideal approach. Furthermore, controversy exists over plate type, length and distance spanning the prosthesis or the bone. Potential complications following surgery include blood loss, loosening, failure or bony union, further fracture and infection (7). Boylan et al. recently described a similar mortality rate in patients following periprosthetic fracture when compared to neck of femur fracture up to 6 months post injury and a 1-year mortality rate of 9.7% (8) highlighting the importance of prioritising management of these patients.
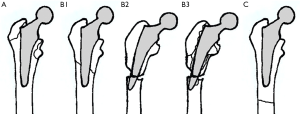
The Vancouver classification system (9) is commonly used to guide management decisions. This includes assessment of fracture location, stability and bone quality (10) (Figure 1). Type A fractures involve the greater or lesser trochanter, type B are diaphyseal starting around the stem and may extend distally whereas type C are distal to the stem in the femoral shaft. The Vancouver system remains the most commonly used due to its simplicity and its application to surgical management (11).
In general, in the context of a well fixed femoral stem (Vancouver B1 or C) it is possible to retain the prosthesis and treat with internal fixation methods (1,12). When there is concern of loosening or instability around the stem (Vancouver B2, B3) then the literature supports revision arthroplasty surgery with or without internal fixation (10). Despite this there remains some controversies surrounding the optimal management of peri-prosthetic fractures such as which internal fixation method is optimal in Vancouver B1 fracture (10) and identification of stable or unstable stems when considering retention of the prosthesis (7). The aim of this article is to present a contemporary evidence-based review of the surgical fixation options for management of periprosthetic fractures in the presence of well-fixed components.
Methods of internal fixation around stable stems
Fixation options in the context of a Vancouver B1 or C fractures are limited by restricted bony fixation proximally given the presence of a femoral stem and often in compromised bone stock. Complications following operative intervention for periprosthetic fractures can include blood loss, non-union, re-fracture or metalwork failure and implant loosening (13). These issues are compounded by the predisposition for these injuries to occur in patients of older age with more significant co-morbidity and reduced physiological reserve (4). Previous studies have been published describing the outcomes of operative intervention of these fractures, but the treatment methods have been heterogenous (14,15).
Plates
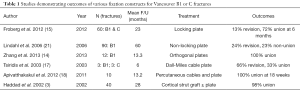
High failure rates and need for reoperation have previously been described by Lindahl et al. (13) with the use of single plate fixation for treatment of Vancouver B and C type fractures with an overall failure rate of 33.9%. Froberg et al. (15) described a 13% failure rate and need for revision in cases treated exclusively with locking plate fixation. Zhang et al. described orthogonal plating of 12 patients with Vancouver B fractures around cemented or uncemented femoral stems and reported that all cases had united at a mean of 12.5 weeks with no complications of infection or deep vein thrombosis (DVT) (14). These failures demonstrate that no single options for plate fixation of periprosthetic fractures is without risk. In addition, some of these failures may at least in part be due to a failure to recognise the original injury as involving a loose stem (13).
The potential benefits of using locking plates is the option for unicortical screw fixation and theoretical increased pull out strength when used in osteoporotic bone. Furthermore, there is in vitro evidence of increased resistance to axial load and torsion compared to non-locking plates (16). Despite this, evidence suggests that locking plates are associated with a higher rate of non-union and implant failure when used to treat Vancouver B1 fracture compared to non-locking plates (10) which may be a result of changing the strain at the fracture site and reducing healing potential while not achieving optimal compression at the fracture site.
Cables
Cerclage wire or cable fixation is commonly employed in the management of intra-operative periprosthetic fracture at time of primary surgery however this technique may also be applied to management of post-operative periprosthetic fractures. Authors have reported the use of both open cable fixation or percutaneous cable fixation but the majority of studies describe combined plate and cable techniques rather than cable fixation in isolation. Previous reports of “cable-only” plate fixation (i.e., no screws used) showed that this construct had high rates of failure and need for revision surgery. In a 16-patient series which included 3 Vancouver B1 fractures, 2 went on to non-union and metalwork failure at 6 months post-surgery with the use of plates and cables alone (17). A recent study demonstrated better outcomes using the hybrid technique of percutaneous cable fixation around the stem combined with distal locking plate fixation. In 10 cases of Vancouver B1 fracture fixed with the above construct with the mean time to union was 18 weeks and no implant failures were observed at an average of 13 months follow up (18).
Strut allograft
Strut allograft fixation has been described by Haddad et al. (3). The use of cortical strut grafts is based on their similar Young’s modulus of elasticity to the host bone therefore theoretically reducing the impact of stress shielding and bone resorption (19). Whilst the cortical bone graft provides an additional biological bone stock and structural support in the early phase of treatment some concern remains that as the graft incorporates its loses its mechanical strength (3). Cortical strut allografts are rarely used in isolation. They are more often applied and used in combination with plate fixation (10). The combination of plate and strut allograft in combination has been demonstrated to provide a very stable construct during in vitro biomechanical studies when used in orthogonal planes e.g., lateral plate fixation and anterior cortical struct graft fixation (20). In vivo results don’t appear to confer any added benefit over plate cable or compression plate fixation despite the additional procedure burden and economic impact of cortical strut graft use however (10) (Table 1).
Full table
The need to fix and revise—Vancouver B2 & B3
The presence of a loose stem associated with a periprosthetic fracture requires revision arthroplasty and fixation with the aim of achieving both a stable implant and a healed fracture (22). Revision arthroplasty for peri-prosthetic fractures has been described using both uncemented and cemented implants.
When uncemented prostheses are used, tapered fluted titanium stems can be used to achieve diaphyseal fixation while enabling the surgeon to bypass the fracture site and achieve fixation distal to the fracture (11). Modular implants have previously been popular allowing more freedom to reconstruct the anatomy; however, there is an increasing trend towards non-modular implants which avoid complications associated with corrosion and fatigue failure particularly when bone stock support may be limited (23).
Controversy surrounds periprosthetic fractures in the presence of a cemented hip replacement and whether the stem should be considered loose given that inherent lack of bonding between cement and stem. Some authors have suggested that the presence of fracture around a cemented stem is as an absolute indication for revision arthroplasty (22). In contrast, Goudie et al. achieved a 91% union rate in 79 periprosthetic fractures around cemented polished tapered stems using open reduction internal fixation (ORIF) with a broad dynamic compression plate (DCP) plate only suggesting that simultaneous revision arthroplasty is not required (24). Furthermore, the authors advocate, and had no complication from the use of biocritical locking screws proximally, avoiding the stem but accepting the cement mantle may be breeched. This has also been the experience of the senior authors.
Regardless of the stem fixation there has been concern raised that increased failure of fixation in some fracture patterns may be due to the incorrect diagnosis of a B2 fractures (13) i.e., failure to recognise at the time of presentation that the stem is loose. Certainly, evidence from the Swedish Hip Arthroplasty registry suggests poor outcomes with fixation of B1 fracture compared to fixation and revision of B2 fractures and it has been proposed that this may be an indication of mis-diagnosis of a B2 fracture at initial presentation and failure to recognise that the loose stem (13).
Encouraging outcomes have been reported following treatment of Vancouver B2 and B3 fractures with revision of the stem and reduction and cable fixation of the fractured proximal femur. The rate of union reported with this technique has been reported to be 98% union and 11% revision rates at a mean follow up for 4.5 years (11).
Vancouver B3 fractures present unique surgical challenges as there is a loose prosthesis in the presence of poor bone quality and often poor bone stock. While a fix and revise approach may be effective we would recommend having other options available such as impaction bone grafting (25) or reconstruction using megaprosthesis (26). These patients often have significant co morbidities therefore techniques which facilitate expedient reconstruction and with minimal anaesthetic time and surgical burden should be considered and a single surgical episode is preferable to need for revision surgery.
Discussion
In a recent systematic review of internal fixation methods for Vancouver B1 fractures (10), four groups were separated based on the type of construct used including ORIF with cortical strut allograft, ORIF with cable or compression plate, ORIF with plate and strut graft and ORIF with locking plates. The final analysis included 333 patients of which 46% were fixed with cable or compression plate, 36% with locking plates, 13% with plating and cortical strut graft and 6% with cortical strut graft only. The union rate was 95% for all types of fixation and when grouped complications included non-union (5%), metal work failure (4%), infection (5%) and need for reoperation (9%). In particular locking plate fixation demonstrated a more significant complication rate for non-union 9% vs. 3% and metalwork failure 7% vs. 2% therefore supporting the use of cable plate or compression plating techniques. In addition, the authors highlight the fact that in this complex highly comorbid population the reoperation rate of 9% represents a significant burden with high risk for the patients involved. In this often-challenging group of patients we suggest that the main surgical priorities should focus on achieving a stable reduction with a solid fixation, a stable implant and allowing early mobilisation and full weight bearing.
We retrospectively reviewed the outcomes of total femoral plating of periprosthetic fractures around stable hip or knee replacements to consider whether a spanning plate from trochanter to distal femur may reduce the risk of further periprosthetic fracture or metalwork failure whilst allowing our patients to fully weight bear immediately following surgery. We followed up 17 patients at a mean duration of 24 months post-op who had undergone total femoral plating for a periprosthetic fracture of the femur (unpublished data). Nine cases involved only a total hip replacement (THR), 6 cases only a total knee replacement (TKR) and 2 cases were interprosthetic. Average age was 72.5 years (range, 42–88 years), 88% were female, 12% female. Median ASA grade was 3.
Three patients were excluded from outcome scores as they were unable to complete the questionnaires due to dementia. Of the remaining 14 patients the mean Oxford Hip or Knee score was 50.25 (range, 23–60), EQ-5D scores were 4.0, 4.3, 4.1, 4.3 and 4.1 out of 5 for mobility, self-care, activity, pain and anxiety respectively. Visual Analogue Scale for general health was 64.4/100. At 6 months follow up 76% had achieved clinical and radiographic union. There were no other implant or patient related complications observed when using total femoral plating suggesting that this is a safe option. Moloney et al. 2014 also describe a similar technique by ensuring their plating technique extended from trochanter down to the femoral condyles around well-fixed stems. In 21 patients treated using this fixation method mean time to union was 19 weeks and there were no cases of non-union and metalwork failure unlike a comparable shorter plate fixation cohort (27). Therefore, we propose that the technique of plate application may be as important as the choice of internal fixation construct and future studies should also aim to compare “spanning” or “total femoral plating” outcomes.
Conclusions
In the presence of a well-fixed stem there are various options for retaining the implant and reduction and fixation of the fracture, but loose implants require revision arthroplasty and internal fixation. We have described some of the potential pitfalls of internal fixation of periprosthetic fractures including non-union, metalwork failure and discussed the important relationship to the physiologic health of the patient. Future large-scale randomised trials are needed to determine the optimum fixation option with an aim to reduce these complications.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.07.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chakravarthy J, Bansal R, Cooper J. Locking plate osteosynthesis for Vancouver Type B1 and Type C periprosthetic fractures of femur: a report on 12 patients. Injury 2007;38:725-33. [Crossref] [PubMed]
- Katz JN, Wright EA, Polaris JJ, et al. Prevalence and risk factors for periprosthetic fracture in older recipients of total hip replacement: a cohort study. BMC Musculoskelet Disord 2014;15:168. [Crossref] [PubMed]
- Haddad FS, Duncan CP, Berry DJ, et al. Periprosthetic femoral fractures around well-fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg Am 2002;84-A:945-50. [Crossref] [PubMed]
- Bhattacharyya T, Chang D, Meigs JB, et al. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am 2007;89:2658-62. [Crossref] [PubMed]
- Birch CE, Blankstein M, Chlebeck JD, et al. Orthogonal plating of Vancouver B1 and C-type periprosthetic femur fracture nonunions. Hip Int 2017;27:578-83. [Crossref] [PubMed]
- Mont MA, Maar DC. Fractures of the ipsilateral femur after hip arthroplasty. A statistical analysis of outcome based on 487 patients. J Arthroplasty 1994;9:511-9. [Crossref] [PubMed]
- Giannoudis PV, Kanakaris NK, Tsiridis E. Principles of internal fixation and selection of implants for periprosthetic femoral fractures. Injury 2007;38:669-87. [Crossref] [PubMed]
- Boylan MR, Riesgo AM, Paulino CB, et al. Mortality Following Periprosthetic Proximal Femoral Fractures Versus Native Hip Fractures. J Bone Joint Surg Am 2018;100:578-85. [Crossref] [PubMed]
- Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect 1995;44:293-304. [PubMed]
- Dehghan N, McKee MD, Nauth A, et al. Surgical fixation of Vancouver type B1 periprosthetic femur fractures: a systematic review. J Orthop Trauma 2014;28:721-7. [Crossref] [PubMed]
- Abdel MP, Cottino U, Mabry TM. Management of periprosthetic femoral fractures following total hip arthroplasty: a review. International Orthopaedics 2015;39:2005-10. (SICOT). [Crossref] [PubMed]
- Bryant GK, Morshed S, Agel J, et al. Isolated locked compression plating for Vancouver Type B1 periprosthetic femoral fractures. Injury 2009;40:1180-6. [Crossref] [PubMed]
- Lindahl H, Malchau H, Odén A, et al. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Br 2006;88:26-30. [Crossref] [PubMed]
- Zhang Y, Fan X, Liu Y, et al. Limited open reduction and double plates internal fixation for treatment of Vancouver type B1 periprosthetic femoral fracture after hip arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2013;27:1428-31. [PubMed]
- Froberg L, Troelsen A, Brix M. Periprosthetic Vancouver type B1 and C fractures treated by locking-plate osteosynthesis: fracture union and reoperations in 60 consecutive fractures. Acta Orthop 2012;83:648-52. [Crossref] [PubMed]
- Fulkerson E, Egol KA, Kubiak EN, et al. Fixation of diaphyseal fractures with a segmental defect: a biomechanical comparison of locked and conventional plating techniques. J Trauma 2006;60:830-35. [Crossref] [PubMed]
- Tsiridis E, Haddad FS, Gie GA. Dall-Miles plates for periprosthetic femoral fractures. A critical review of 16 cases. Injury 2003;34:107-10. [Crossref] [PubMed]
- Apivatthakakul T, Phornphutkul C, Bunmaprasert T, et al. Percutaneous cerclage wiring and minimally invasive plate osteosynthesis (MIPO): a percutaneous reduction technique in the treatment of Vancouver type B1 periprosthetic femoral shaft fractures. Arch Orthop Trauma Surg 2012;132:813-22. [Crossref] [PubMed]
- Mihalko WM, Beaudoin AJ, Cardea JA, et al. Finite-element modelling of femoral shaft fracture fixation techniques post total hip arthroplasty. J Biomech 1992;25:469-76. [Crossref] [PubMed]
- Zdero R, Walker R, Waddell JP, et al. Biomechanical evaluation of periprosthetic femoral fracture fixation. J Bone Joint Surg Am 2008;90:1068-77. [Crossref] [PubMed]
- Lindahl H, Garellick G, Regnér H, et al. Three Hundred and twenty-one periprosthetic femoral fractures. J Bone Joint Surg Am 2006;88:1215-22. [Crossref] [PubMed]
- Grammatopoulos G, Pandit H, Kambouroglou G, et al. A unique peri-prosthetic fracture pattern in well fixed femoral stems with polished, tapered, collarless design of total hip replacement. Injury 2011;42:1271-6. [Crossref] [PubMed]
- Sandiford NA, Garbuz DA, Masri BA, et al. Nonmodular Tapered Fluted Titanium Stems Osseointegrate Reliably at Short Term in Revision THA’s. Clin Orthop Relat Res 2017;475:186-92. [Crossref] [PubMed]
- Goudie ST, Patil S, Patton JT, et al. Outcomes following osteosynthesis of periprosthetic hip fractures around cemented tapered polished stems. Injury 2017;48:2194-200. [Crossref] [PubMed]
- Wimmer MD, Randau TM, Deml MC, et al. Impaction grafting in the femur in cementless modular revision total hip arthroplasty: a descriptive outcome analysis of 243 cases with the MRP-TITAN revision implant. BMC Musculoskelet Disord 2013;14:19. [Crossref] [PubMed]
- Parvizi J, Sim FH. Proximal femoral replacements with megaprostheses. Clin Orthop Relat Res 2004;169-75. [Crossref] [PubMed]
- Moloney GB, Westrick ER, Siska PA, et al. Treatment of periprosthetic femur fractures around a well-fixed hip arthroplasty implant: span the whole bone. Arch Orthop Trauma Surg 2014;134:9-14. [Crossref] [PubMed]
Cite this article as: Davenport D, Hutt JR, Mitchell PA, Trompeter A, Kendoff D, Sandiford NA. Management of peri-prosthetic fractures around total hip arthroplasty: a contemporary review of surgical options. Ann Joint 2018;3:65.