
Use of external fixator pre- and post-reconstruction in the multiligament injured knee
Introduction
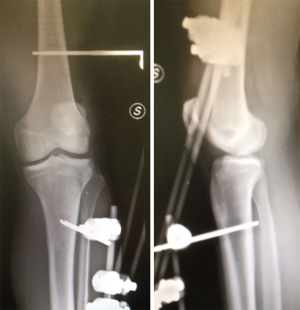
Multiligament knee injury (MLKIs) is a rare condition, making up the 0.02% of the orthopedic injuries, but are potentially devastating to patients. The management of such lesions mandates a clear knowledge of the anatomy on all sides of the joint. In addition to the ligamentous injury, the surgeon must also be vigilant for vascular or neurological damage that can often complicate MLKIs (Figures 1,2). There are several strategies for the management of knee dislocation which in many cases are controversial (1,2). The nonoperative treatment has historically represented the standard of care for decades, however, the results in term of range of motion and clinical outcomes were reported to be poor (3,4). Therefore, surgery is recommended with the aim to repair or reconstruct all the structures involved by the injury (5,6). However, even after surgery, MLKIs are burdened with high rates of knee stiffness and recurrent instability (5-7). Hanley et al. in a recent study reported a postoperative stiffness rate up to 20%. This complication occurs particularly if the injury involves three or more ligaments, because extensive hemarthrosis and surrounding soft tissue damage often can lead to secondary adhesion and capsulitis (8). Numerous authors advocate the use of aggressive rehabilitation protocols to reduce the rate of arthrofibrosis despite the risk of increasing the stress on immature grafts (9). Therefore, articulated external fixator (EF) has been proposed for protecting the grafts during intensive postoperative physical therapy. EF has also been advocated in the pre-operative period, in case of chronic knee dislocations (7,10,11) and periarticular fracture (12) (Figures 3,4).


External fixator biomechanics
The original surgically emplaced hinge was developed for the use on elbow (Compass Elbow Hinge, Smith and Nephew). Since that time different prototypes have been developed and used in the clinical setting. In the first cadaveric study performed by Simonian et al. in 1998, compression-distraction and anteroposterior translation of the knee during flexion-extension were evaluated using fluoroscopy in two settings: first with intact ligaments and then with multiligament disruption. In both settings the knee was immobilized using a hinged EF. The results were then compared with the contralateral healthy knee in order to identify if this type of immobilization was able to reproduce the native knee kinematics. The authors did not report differences regarding the compression-distraction part of the test, while there was a statistically significant posterior tibial translation in the multiligament injured setting when the knee reached 60° of flexion (13).
Since that time, the biomechanics of the hinged EF has substantially improved aiming to reproduce the four-bar linkage model of the knee and guide the posterior rollback of the femoral condyle during knee flexion. Recently, Marcacci et al. performed an in vitro kinematic evaluation of the tibial movement respect to the femur with and without a hinged EF. This device allows only flexion-extension of the knee (between 0–100°) and the posterior rollback of the knee while internal-external rotation is fixed. Their results show that, if the pins are placed correctly and the EF is positioned according to the transepicondylar axis, the device is able to reproduce the natural knee motion throughout the flexion-extension movement. Therefore, correct alignment of the knee flexion-extension axis with the fixator axis is crucial to avoid abnormal forces on the grafts (14).
Recently Mercer et al. evaluated the stiffness of knee-spanning EF in a different configuration. Their results show that a hinged fixator provides as much stiffness as the unhinged configuration, hence it should not be avoided based on concern for instability (15). Similarly, Fitzpatrick et al. investigated on a cadaveric model the ability of an articulated fixator to reduce stresses on the setting of a multiligament injured knee. Their results showed a reduced tibiofemoral translation by 49% for Lachman test, by 70% for anterior drawer test and 46% for posterior drawer test. The authors did not notice differences, in terms of joint displacement and ligament protection between mono- and bilateral fixator configuration (16).
Knee immobilization in the pre-operative period
Bracing versus external fixation: indications
Once the knee has been satisfactory reduced, vascular injury has been ruled out and physical examination and imaging studies have been performed, the surgeon must plan a surgical reconstruction. There are two potential approaches reported in the literature. Some surgeons prefer to address all the torn ligaments in the acute setting (defined as less than 2–3 weeks) while others perform surgery after this period (17). This delay allows the inflammatory phase to subside and to restore range of motion, reducing the risk of arthrofibrosis. In this setting, if arthroscopy is performed, there is no risk of a damaged capsule can that lead to fluid extravasation and compartment syndrome. Other authors advocate an early reconstruction, and their choice is supported by a systematic review conducted by Levy et al. where higher functional outcome, International Knee Documentation Comitee (IKDC), and sports activity score have been reported in patients treated within 3 weeks.
Regardless of the surgical timing, in the pre-operative period immobilization of the knee can be achieved with a knee brace locked in extension or with an EF. Casting or splinting are not indicated due to the risk of circumferential compression of the limb and the reduced possibility to identify vasospasm or vascular intimal flap lesion that can cause ischemia even after several hours from the injury. If a knee brace is applied, several X-rays should be performed in the pre-operative period to confirm that the reduction is maintained. If the brace is not able to avoid subluxation of the knee, then the application of an EF should be considered.
Indications
The indications for the use of spanning EF are controversial. In the literature some authors advocate its use in a subgroup of patient:
- severe polytrauma;
- open dislocation;
- patients with an unstable knee even after a successful reduction, particularly if the instability is in the anteroposterior plane;
- vascular surgery, in order to avoid stress forces on the vascular graft;
- morbidly obese patients [body mass index (BMI) >35];
- inability to tolerate immobilization in a knee brace alone.
It is important to underline that the pins should be placed at a certain distance from the future surgical incision following AO guidelines and that a spanning EF should not be applied for more than 6 weeks, otherwise the risk of arthrofibrosis is higher (18).
Knee immobilization in the post-operative period
Bracing versus external fixation: failure, range of motion, clinical score
In the last years, several publications have advocated the use of hinged EF in the context of MLKIs reconstruction when surgery needs to be delayed. Stannard et al. reported a lower incidence of ligament failure in the group treated with a hinged EF. Their results show a 7% of overall ligament failure in the EF group versus 29% in the group treated with a knee brace at 24 months of follow-up. Specifically, the failure rate of the Posterolateral corner repair was only 13% in the EF group versus the 54% in the control group (9).
A similar statistically significant (P<0.001) lower rate of ligament failure was reported in a prospective randomized trial at a follow up of 3.3 years. The failure rate was 21% in the knee bracing group (22 of 105), while the percentage in the group with external stabilization was 7% (11 of 157). Similarly, when the patients experienced a ligament failure, they were less likely to have multiple ligament failure if they were immobilized with the EF (failure per patient was 1.57 versus 2.44) (19).
These data are in contrast with the results of Angelini et al. In their prospective study, 33 patients were allocated to two groups for immobilization after reconstruction (cast vs. EF). At the final follow-up of 26 months, there were no difference in ligament stability between groups (20).
The range of motion in flexion-extension was documented in two different studies by Stannard et al. after acute MLKI surgery and aggressive rehabilitation. In both studies there were no statistical differences between the two types of immobilization (9,19).
Conversely, Angelini et al. reported better knee flexion in patients treated with EF: the flexion deficit was only 5° compared with 18° measured in the group immobilized with the knee brace. No difference in extension loss was reported (20). If we focus on the clinical results, other authors did not notice any difference at the final examination (9,19). While, in a randomized controlled trial, at 14 months of mean follow-up, patients treated with an EF showed better Lysholm scores, with the 73% of patients with excellent or good clinical score, compared with 35% of the patients immobilized with rigid knee bracing (20).
There are several disadvantages to use the articulated EF that must be balanced against the improvement in terms of stability. The application of this device provides additional surgical cost and prolong the surgical time of approximately 30 minutes. Moreover, superficial infection on the site of the fixator pins has been reported (18,19). Furthermore, it is difficult to tolerate it, since the femoral pins cause often pain when the knee is flexed beyond 60°.
Conclusions
There is still no consensus in many aspects of the management of MLKI. Among these it is still unclear which type of immobilization is the most appropriate. A postoperative brace appears to be appropriate for most knee dislocation but, in some cases, may not be sufficient. A hinged EF should be considered as an alternative option in patients with highly unstable knee, vascular damage, morbidly obese or severe polytrauma. Additional studies at a longer follow-up could help the surgeon to identify the right candidate for a skeletal fixation and help to clarify if the disadvantages of such procedure are compensated by better clinical outcome.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Camilo Partezani Helito and Jorge Chahla) for the series “The Multiligament Injured Knee” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.09.04). The series “The Multiligament Injured Knee” was commissioned by the editorial office without any funding or sponsorship. SZ serves as an unpaid editorial board member of Annals of Joint from Mar 2017 to Feb 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mariani PP, Santoriello P, Iannone S, et al. Comparison of surgical treatments for knee dislocation. Am J Knee Surg 1999;12:214-21. [PubMed]
- Martinek V, Steinbacher G, Friederich NF, et al. Operative treatment of combined anterior and posterior cruciate ligament injuries in complex knee trauma: can the cruciate ligaments be preserved? Am J Knee Surg 2000;13:74-82. [PubMed]
- Fanelli GC, Stannard JP, Stuart MJ, et al. Management of complex knee ligament injuries. J Bone Joint Surg Am 2010;92:2235-46. [PubMed]
- Taylor AR, Arden GP, Rainey HA. Traumatic dislocation of the knee. A report of forty-three cases with special reference to conservative treatment. J Bone Joint Surg Br 1972;54:96-102. [Crossref] [PubMed]
- Harner CD, Waltrip RL, Bennet CH, et al. Surgical management of knee dislocations. J Bone Joint Surg Am 2004;86:262-73. [Crossref] [PubMed]
- Ibrahim SA, Ahmad FH, Salah M, et al. Surgical management of traumatic knee dislocation. Arthroscopy 2008;24:178-87. [Crossref] [PubMed]
- Noyes FR, Barber-Westin SD. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Use of early protected postoperative motion to decrease arthrofibrosis. Am J Sports Med 1997;25:769-78. [Crossref] [PubMed]
- Hanley J, Westermann R, Cook S, et al. Factors Associated with Knee Stiffness following Surgical Management of Multiligament Knee Injuries. J Knee Surg 2017;30:549-54. [Crossref] [PubMed]
- Stannard JP, Sheils TM, McGwin G, et al. Use of a hinged external knee fixator after surgery for knee dislocation. Arthroscopy 2003;19:626-31. [Crossref] [PubMed]
- Simonian PT, Wickiewicz TL, Hotchkiss RN, et al. Chronic knee dislocation: reduction, reconstruction, and application of a skeletally fixed knee hinge. A report of two cases. Am J Sports Med 1998;26:591-6. [Crossref] [PubMed]
- Angelini FJ, Helito CP, Bonadio MB, et al. Surgical management of knee dislocations with ligament reconstruction associated with a hinged external fixator. Orthop Traumatol Surg Res 2015;101:77-81. [Crossref] [PubMed]
- Pavolini B, Maritato M, Turelli L, et al. The Ilizarov fixator in trauma: a 10-year experience. J Orthop Sci 2000;5:108-13. [Crossref] [PubMed]
- Simonian PT, Sussmann PS, Wickiewicz TL, et al. The skeletally fixed knee hinge for the grossly unstable knee. Am J Knee Surg 1998;11:181-7. [PubMed]
- Marcacci M, Zaffagnini S, Bonanzinga T, et al. Surgical technique: articulated external fixator for treatment of complex knee dislocation. Clin Orthop Relat Res 2012;470:869-76. [Crossref] [PubMed]
- Mercer D, Firoozbakhsh K, Prevost M, et al. Stiffness of knee-spanning external fixation systems for traumatic knee dislocations: a biomechanical study. J Orthop Trauma 2010;24:693-6. [Crossref] [PubMed]
- Fitzpatrick DC, Sommers MB, Kam BC, et al. Knee stability after articulated external fixation. Am J Sports Med 2005;33:1735-41. [Crossref] [PubMed]
- Magnussen RA, Riboh JC, Taylor DC, et al. How We Manage the Multiple Ligament Injured (Dislocated) Knee. Oper Tech Sports Med 2010;18:211-8. [Crossref]
- Moatshe G, Chahla J, La Prade RF, et al. Diagnosis and treatment of multiligament knee injury: state of the art. J ISAKOS 2017; [Crossref]
- Stannard JP, Nuelle CW, McGwin G, et al. Hinged external fixation in the treatment of knee dislocations: a prospective randomized study. J Bone Joint Surg Am 2014;96:184-91. [Crossref] [PubMed]
- Angelini FJ, Helito CP, Bonadio MB, et al. External fixator for treatment of the sub-acute and chronic multi-ligament-injured knee. Knee Surg Sports Traumatol Arthrosc 2015;23:3012-8. [Crossref] [PubMed]
Cite this article as: Lucidi GA, Grassi A, Cucurnia I, Macchiarola L, Zaffagnini S. Use of external fixator pre- and post-reconstruction in the multiligament injured knee. Ann Joint 2018;3:76.



