Wrist arthroscopy in the management of distal radius fractures
Introduction
Wrist arthroscopy has emerged as a potentially useful adjunct procedure in the surgical management of distal radius fractures (1). Although not required for every fracture, it may be beneficial in certain cases (2). Compared to more traditional techniques where the articular surface is reduced using an image intensifier, arthroscopy has the advantage of allowing direct visualization of the articular surface to assess and guide fracture reduction (1,3-8). It also has the advantage of allowing assessment and management of concomitant soft tissue injuries such as intercarpal ligament injuries, triangular fibrocartilage complex (TFCC) injuries and chondral pathology (9-12). Wrist arthroscopy however, is not without its problems. It can be technically challenging and is associated with additional surgical time and costs (13,14) (Table 1). While it is still unclear if chasing the perfect arthroscopic reduction or addressing soft tissue injuries leads to better outcomes, it should be considered in select cases where the difficulty of obtaining anatomical reduction is anticipated or soft tissue injuries are suspected. The aim of this review is to outline the indications for wrist arthroscopy in the setting of fractures and discuss the advantages and disadvantages of this adjunctive procedure. In doing so, the authors examine important technical considerations and review the outcome of surgery.
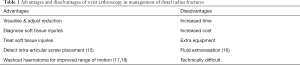
Full table
Indications
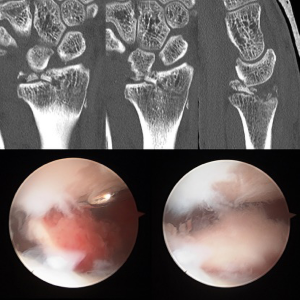
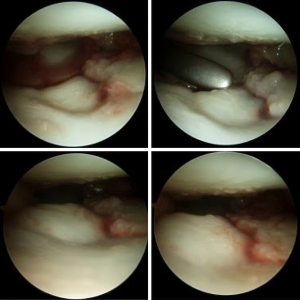
Wrist arthroscopy should be considered in young high demand patients when the difficulty of achieving a good reduction is anticipated or associated soft tissue injuries are suspected. Fractures with a die punch fragment, central comminution, lunate facet involvement, depressed fragments with residual step off >1 mm after fluoroscopic reduction, floating or flipped upside down osteochondral fragments will possibly benefit from arthroscopically assisted reduction of the articular surface (9,12,19-21) (Figures 1,2).
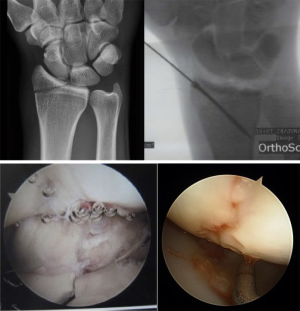
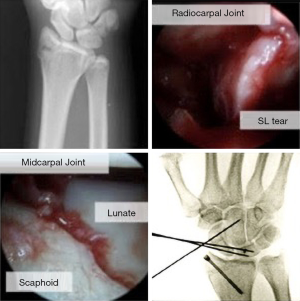
Although there is often no direct correlation, the authors feel the presence of radiographic signs suggestive of soft tissue injuries such as widening of the scapholunate gap and/or abnormal scapholunate angles, disruption of Gilula’s lines, widening of the distal radioulnar joint require further evaluation with wrist arthroscopy to more accurately categorise and treat where appropriate (9,20,22) (Figure 3).

Radial styloid fractures are a particular subgroup that should be considered for arthroscopically assisted surgery. Fluoroscopic reduction alone may be misleading, as the fragment may be mal-rotated. In addition, these fractures are well known to be associated with scapholunate ligament injury as part of a greater arc injury. It has also been suggested that this fracture is ideal for percutaneous arthroscopically assisted reduction and fixation (21) (Figures 4-6).

Fracture reduction
Anatomical reduction of the articular surface in addition to restoration of extra-articular alignment is the goal in the management of intra-articular fractures to optimize the chance of a good outcome and potentially prevent early onset post-traumatic arthritis (23). It is particularly important for young, high demand patients who often sustain high energy complex distal radius fractures compared to the low energy “Colles” type fractures in elderly patients (23,24). Knirk and Jupiter reported that residual incongruity of the radiocarpal joint (articular step off >2 mm) was associated with early radiographic arthritis in young patients (23) with some authors advocating a step off <1 mm being required for a better result (25-27). Combined incongruity that is a combination of a step off and a gap also seems important (27,28). Although there is a lack of correlation between radiographic signs of arthritis and patient symptoms (29,30), it is reasonable to strive for anatomical reduction, particularly in younger patients with higher functional demands. In this regard, reduction is better appreciated during arthroscopy compared to a fluoroscopic assessment (3-6).
Associated soft tissue injury evaluation
There is emerging evidence to show that distal radius fractures can be associated with soft tissue injuries including scapholunate & lunotriquetral ligament tears, TFCC and chondral injuries. The incidence identified arthroscopically in association with distal radius fractures is high and has been reported to range from 68% to 81% in a number of studies (9-11,31).
In these studies, TFCC injuries and scapholunate tears were the most commonly observed, while lunotriquetral ligaments injuries were rare. Swart and Tang analysed 13 studies, the average reported rate being 44% for all grades of scapholunate ligament tears, 43% for TFCCs, 32% for cartilage damage and 13% for lunotriquetral ligament tears (10). Radiographs are commonly used to diagnose scapholunate and TFCC injury. In the setting of distal radius fracture this has been shown to be unreliable and often have no direct correlation with the significance of the injury (9,12,15,32).
Without arthroscopy, many of these injuries would go undiagnosed and therefore untreated where applicable.
It is not surprising that arthroscopy detects soft tissue injuries more accurately than plain radiographs, the question remains, what proportion of them if any are clinically significant.
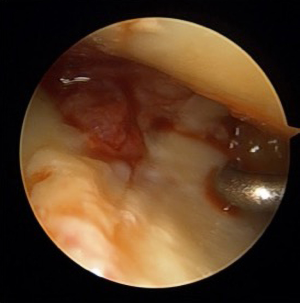
Triangular fibrocartilaginous complex
TFCC injury is a common cause of ulnar sided wrist pain and distal radioulnar joint instability. TFCC tears have been observed in intra and extra articular fractures without a correlation with ulna styloid fractures identified (17). An association with the degree of radial shortening (4 mm) and dorsal angulation (10 degrees) however has been shown (12) and is supported by a cadaver study that found similar displacement is required for the disruption of the ulnar TFCC attachment (18). In their case series Lindau et al. found distal radioulnar joint instability in one third of patients with non-osteoporotic fractures at one year follow up. It was associated with complete peripheral TFCC tears diagnosed by wrist arthroscopy at the time of the injury. Patients with instability had worse functional scores (17) (Table 2). Acute TFCC tear management depends on location of the tear and its severity. Central tears are usually stable and treated with debridement, while peripheral tears could be associated with instability and may need to be repaired arthroscopically or via an open technique (16).
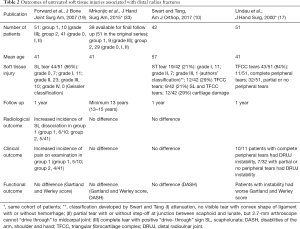
Full table
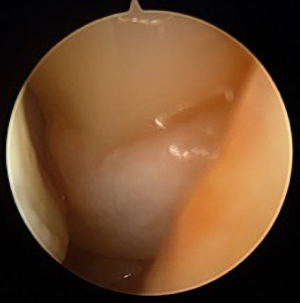
Scapholunate ligament tears
Scapholunate ligament injury can lead to dissociative carpal instability with complete disruption of the ligament complex and secondary stabilisers. In the longer term a predictable pattern of degenerative change is seen known as scapholunate advanced collapse (SLAC wrist). Traditionally diagnosis is made radiographically. Tang et al. used a combination of four radiographic parameters - widening of scapholunate space 3 mm, foreshortened appearance of scaphoid, cortical ring sign and scapholunate angle >70 degrees. They speculated that only tears causing all above changes were significant enough to affect the biomechanics of the wrist and therefore the outcome. In their study they only identified 4.6% patients with radiographic evidence of scapholunate dissociation (SLD) and those patients had worse function (32). Gunal et al. based their diagnosis on widening of the scapholunate gap >2 mm and noted that most of the patients with detected abnormalities were symptomatic and had poorer outcomes (34).
Scapholunate ligament injuries can occur in extra and intra-articular distal radius fractures, although seen more commonly in intra-articular fractures, particularly those that are comminuted and involving the lunate facet (9,12,19-21). Forward et al. noted that fractures with a relative increase in ulna variance >2 mm compared to the uninjured side at the time of injury had a fourfold increase in risk of sustaining a grade III scapholunate ligament tear (19).
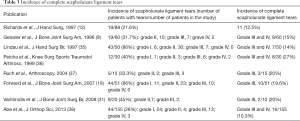
To summarise the published data, complete grade III and grade IV tears are identified by arthroscopy in 10–20% of intra-articular non-osteoporotic distal radius fractures (9,12,19,31,35-38) (Table 3).
Full table
The diagnosis and grading of these injuries is greatly enhanced with arthroscopy (Table 4), however the treatment once diagnosed is more controversial. It is controversial if arthroscopically detected untreated complete tears associated with distal radius fractures will lead to worse outcomes. While some argue that most of the tears probably heal following immobilization as part of the fracture management, others are concerned that even partial tears may progress to complete tears if left untreated, especially with early movement following volar locking plate fixation (19). There is, however, a paucity of evidence to support this stance.

Full table
Grade I & II injuries can be treated by immobilisation (16,19,33). Grade III injuries are usually treated by immobilisation or reduction and percutaneous pinning whereas grade IV injuries are treated by repair and pinning +/− a reinforcement procedure (2,16,19-21).
Age is also important as older patients may have pre-existing degenerative tears. A cadaver study by Wright et al. found scapholunate lesions in 18 out of 62 wrists in the elderly (39) whilst Akahane et al. found that the incidence of asymptomatic static SLD in wrists without distal radius fracture increases with age. They also found that in younger patients SLD was significantly higher in wrists with distal radius fractures and concluded this was more likely due to acute injury (40). This leads to the possibility of overtreatment in older individuals with pre-existing pathology.
Lunotriquetral ligament tears
Lunotriquetral ligament injuries are much less common than other intercarpal soft tissue injuries. Currently there is no evidence for long term disability or instability attributable to lunotriquetral ligament injury associated with distal radius fractures (19,33). There is also no consensus as to what treatment is optimal for diagnosed ligament injuries. Anecdotal and case series evidence for treatment suggests that “stable incomplete”, grade I-III injuries can be treated by immobilization as part of the fracture management. Despite a lack of high level evidence, it is suggested more significant Grade IV injuries be treated with debridement +/− K-wire pinning of the joint (41,42). The exact parameters to determine those, which need debridement only and those, which also need pinning is unclear.
Outcomes
In a systematic review, Smeraglia et al. evaluated 28 studies as part of their analysis (43). The common problem was short follow up, average 19.5 months (range: 4.3–36 months). The majority of the studies were case series, with only three randomised controlled trials and one retrospective case matched study. Of those four studies, an external fixator was used in three (31,37,44), and volar locking plate in one randomised controlled trial (45) (Table 5). Three studies with external fixator found better outcomes with arthroscopically assisted surgery, while the study by Yamazaki et al. on the volar locking plate identified no difference. The average patient age in the study published by Yamazaki et al. however was older than in other studies—62 years (range: 24–92 years) (45).

Full table
Nine papers described their experience combining volar locking plate with wrist arthroscopy (Table 6). Abe et al. (7) in the largest prospective case series of 205 fractures reported a good outcome at an average of 15 months follow up with the DASH score being 3.9 and modified Mayo wrist score being 156 excellent, 47 good, and 2 fair. They felt that with arthroscopy they could achieve a better reduction compared to fluoroscopy alone and could diagnose and manage soft tissue injuries appropriately. In their series 22.7% of the fractures had residual displacement with a gap or step off >2 mm following fluoroscopic reduction as identified by arthroscopy. Lutsky et al. (6) and Ono et al. (5,8) in their case series focused on the accuracy of fluoroscopic reduction assessed by wrist arthroscopy. They confirmed that fluoroscopy often underestimates step off and gap following reduction. Ono et al. also attempted to develop radiological criteria to recommend arthroscopically assisted reduction. They found that combined pre-operative step off and gap on plain radiographs and computer tomography (CT) that is 7.85 mm or more predicts residual incongruity >1 mm following fluoroscopic reduction (5). A minimally invasive technique of volar locked plating (incision 15 mm) that was combined with arthroscopy in 20 patients was described by Zemirline et al. (46). They found arthroscopy useful in the management of osteochondral lesions and soft tissue injuries. Del Pinal et al. (47) described arthroscopically assisted surgery in four patients with severely comminuted diaphyseal-metaphyseal intra-articular fractures with excellent outcomes at 3 years. By applying a long plate and creating a stable reference fragment first, they could continue arthroscopic reduction without losing extra-articular alignment due to diaphyseal-metaphyseal comminution. Kamano et al. (22) reported on the management of complete, multifragmentary articular fractures (AO/ASIF C3.1) with arthroscopically assisted volar locked plating and found arthroscopy useful in the management of this type of fracture. In contrast, Yamazaki et al. (45) in their RCT did not find a difference in outcomes between arthroscopically assisted and conventional surgery with volar locking plates; however, as discussed, they included elderly patients in their study.

Full table
Only a small number of studies have investigated outcomes of non-treated soft tissue injuries (Table 2). The prospective study by Forward et al. identified the difference in outcomes at one year between patients with complete tears and patients without or with only partial injuries (19). At one year follow up they noted a higher incidence of subjective pain on examination and radiographic changes in patients with grade III scapholunate injuries (no grade IV injuries were present in their patients), but no difference in functional outcome, grip strength or tip pinch strength. However, at long-term follow up of the same cohort (minimum of 13 years) no difference in any of the outcomes was identified (33). Swart and Tang did not detect a difference between patients with soft tissue injuries and patients without at one year review. They used their own classification to grade scapholunate injuries and only one patient according to the classification had complete tear. The authors also did not differentiate between outcomes for different grades of tears (10).
Currently, there is not enough evidence to recommend arthroscopy for every patient with a distal radius fracture to assess for intracarpal injury. A decision is made on a case-by-case basis. Younger patients with high energy trauma and evidence of static scapholunate injury on X-ray or widening of the distal radioulnar joint would be likely to have an acute injury and probably will benefit from further evaluation and additional management of soft tissue injuries if present. In addition, younger patients with fractures that are more likely to be associated with soft tissue injuries may also benefit from arthroscopic evaluation for intra-carpal injuries. However, more research into this area is still required.
Technical tips
Imaging
Plain X-ray
CT to more accurately categorise fracture patterns and to plan fixation.
Timing
As dictated by soft tissues, swelling and availability, there is no absolute consensus as to optimal timing (21,43,48).
Equipment
- Traction system with finger traps, preferable leaving 360 degrees working area;
- 2.5 mm arthroscope (1.9 mm can be used);
- Saline for intermittent irrigation;
- Shaver with suction;
- Arthroscopic probes and instruments;
- Fixation system of choice.
Technique
- Approach determined by fracture pattern;
- Fluoroscopy guided fracture reduction and locking plate provisional fixation (7,48);
- Wrist arthroscopy (dry technique) and assessment of fracture reduction and soft tissue injuries;
- Arthroscopically guided fracture reduction;
- Volar locking plate final fixation;
- Soft tissue injuries management.
Fixation
- Commonly volar locking plate;
- Fixation technique comfortable with.
Traction
Standard vertical traction, although the technique of longitudinal traction has been described (41). With vertical traction the arm generally has to be removed from traction to complete volar fixation. With longitudinal traction this does not have to be done but most surgeons are more familiar with vertical traction for arthroscopy (Figure 8).
Dry vs. wet
The technique of dry arthroscopy has been described in detail by Del Pinal (48). He emphasises that to succeed in dry arthroscopy the valve of the scope should be left open to air all the time, while suction to be opened only when needed. If required, the joint could be irrigated with 5–10 mL of fluid via a syringe attached to the side valve of the scope; the fluid then aspirated by the shaver. Fluid is required if a radiofrequency device is used.
Portals
Initially a 3–4 radial portal is established. Prior to proceeding ensure that the arthroscope is in the joint, not in the fracture site. The second, ulna sided portal, is a 4–5 or 6R portal depending on the fracture configuration as a 4–5 portal may interfere with the reduction of the dorsoulnar fragment (21,48).
The joint is irrigated repeatedly to wash out haematoma. Once vision is adequate we find it useful to use the ulna side portal as the viewing portal and to rest the arthroscope on top of the ulna head while doing work radially (48). This helps to keep the scope in a stable position and will not interfere with the fracture fragments reduction. Some authors also recommend using the volar portal to address the dorsal rim fragment (Figure 9) and to assess palmar portion of intercarpal ligaments (7). The volar portal could be safely established through the main incision. Intercarpal ligaments are evaluated further via midcarpal portals (Figure 7).
Reduction
Depressed fragments may be reduced by pushing up from the intramedullary canal via the main or separate dorsal incisions (7) or elevated with an arthroscopic probe or elevator from the inside of the joint and then secured with K-wires and screws (48) (Figure 10).
Bone grafting may be required to support depressed fragments. Conversely, over distracted fragments may be pushed down with a flat instrument. Free osteochondral fragments are re orientated with an arthroscopic probe or grasper, then, once positioned a raft of distal screws is created, the fragment then reduced and impacted with a flat instrument or using the carpus as a mold once traction released (48). Larger fragments could be reduced with a joystick maneuver (Figure 6) or tenaculum forceps. If there is metaphyseal comminution or multiple unreduced fragments then it is important to create a stable ulna or radial fragment first by reducing it and securing with screws and then complete the reduction by building on it (21,48). Small loose intra-articular fragments can be removed.
Postoperative management
Overnight stay for elevation, pain management +/− plaster slab.
Removable thermoplastic splint for comfort and active range of motion commenced. Vitamin C 500 mg is prescribed for 3 months (49) for all patients. X-rays are obtained at 6–8 weeks to evaluate for union.
This management is predicated on fracture stability. If there is any doubt about the stability of fixation or the fracture then the patient is immobilized for up to 6 weeks.
The management of patients with associated soft tissue injuries is determined by the nature of the soft tissue injury and its treatment (or not).
Conclusions
Wrist arthroscopy can be a valuable technique to utilize in the management of distal radius fractures. It is especially helpful with fractures that are difficult to reduce without visualizing the articular surface or that have a higher chance of simultaneous soft tissue injuries. It appears that arthroscopically assisted surgery is associated with better short and medium term results. Despite it being unclear whether wrist arthroscopy provides an advantage in the long term, in particular with volar locking plating, it should be considered in younger patients with higher functional demands. At what cost in time, money and risk this reduction should be achieved is yet to be elucidated.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.08.06). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Burnier M, Le Chatelier Riquier M, Herzberg G. Treatment of intra-articular fracture of distal radius fractures with fluoroscopic only or combined with arthroscopic control: A prospective tomodensitometric comparative study of 40 patients. Orthop Traumatol Surg Res 2018;104:89-93. [Crossref] [PubMed]
- Abe Y, Fujii K. Arthroscopic-Assisted Reduction of Intra-articular Distal Radius Fracture. Hand Clin 2017;33:659-68. [Crossref] [PubMed]
- Edwards CC 2nd, Haraszti CJ, McGillivary GR, et al. Intra-articular distal radius fractures: arthroscopic assessment of radiographically assisted reduction. J Hand Surg Am 2001;26:1036-41. [Crossref] [PubMed]
- Augé WK 2nd, Velazquez PA. The application of indirect reduction techniques in the distal radius: the role of adjuvant arthroscopy. Arthroscopy 2000;16:830-5. [Crossref] [PubMed]
- Ono H, Katayama T, Furuta K, et al. Distal radial fracture arthroscopic intraarticular gap and step-off measurement after open reduction and internal fixation with a volar locked plate. J Orthop Sci 2012;17:443-9. [Crossref] [PubMed]
- Lutsky K, Boyer MI, Steffen JA, et al. Arthroscopic assessment of intra-articular distal radius fractures after open reduction and internal fixation from a volar approach. J Hand Surg Am 2008;33:476-84. [Crossref] [PubMed]
- Abe Y. Plate presetting and arthroscopic reduction technique (PART) for treatment of distal radius fractures. Handchir Mikrochir Plast Chir 2014;46:278-85. [Crossref] [PubMed]
- Ono H, Furuta K, Fujitani R, et al. Distal radius fracture arthroscopic intraarticular displacement measurement after open reduction and internal fixation from a volar approach. J Orthop Sci 2010;15:502-8. [Crossref] [PubMed]
- Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am 1996;78:357-65. [Crossref] [PubMed]
- Swart E, Tang P. The Effect of Ligament Injuries on Outcomes of Operatively Treated Distal Radius Fractures. Am J Orthop (Belle Mead NJ) 2017;46:E41-6. [PubMed]
- Ogawa T, Tanaka T, Yanai T, et al. Analysis of soft tissue injuries associated with distal radius fractures. BMC Sports Sci Med Rehabil 2013;5:19. [Crossref] [PubMed]
- Richards RS, Bennett JD, Roth JH, et al. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am 1997;22:772-6. [Crossref] [PubMed]
- Herzberg G. Intra-articular fracture of the distal radius: arthroscopic-assisted reduction. J Hand Surg Am 2010;35:1517-9. [Crossref] [PubMed]
- Hardy P, Gomes N, Chebil M, et al. Wrist arthroscopy and intra-articular fractures of the distal radius in young adults. Knee Surg Sports Traumatol Arthrosc 2006;14:1225-30. [Crossref] [PubMed]
- Bunker DL, Pappas G, Moradi P, et al. Radiographic signs of static carpal instability with distal end radius fractures: is current treatment adequate? Hand Surg 2012;17:325-30. [Crossref] [PubMed]
- Lindau T. Arthroscopic Evaluation of Associated Soft Tissue Injuries in Distal Radius Fractures. Hand Clin 2017;33:651-8. [Crossref] [PubMed]
- Lindau T, Adlercreutz C, Aspenberg P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg Am 2000;25:464-8. [Crossref] [PubMed]
- Scheer JH, Adolfsson LE. Pathomechanisms of ulnar ligament lesions of the wrist in a cadaveric distal radius fracture model. Acta Orthop 2011;82:360-4. [Crossref] [PubMed]
- Forward DP, Lindau TR, Melsom DS. Intercarpal ligament injuries associated with fractures of the distal part of the radius. J Bone Joint Surg Am 2007;89:2334-40. [PubMed]
- Mudgal CS, Jones WA. Scapho-lunate diastasis: a component of fractures of the distal radius. J Hand Surg Br 1990;15:503-5. [Crossref] [PubMed]
- Geissler WB. Intra-articular distal radius fractures: the role of arthroscopy? Hand Clin 2005;21:407-16. [Crossref] [PubMed]
- Kamano M, Koshimune M, Kazuki K, et al. Palmar plating for AO/ASIF C3.2 fractures of the distal radius with arthroscopically assisted reduction. Hand Surg 2005;10:71-6. [Crossref] [PubMed]
- Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am 1986;68:647-59. [Crossref] [PubMed]
- Bradway JK, Amadio PC, Cooney WP. Open reduction and internal fixation of displaced, comminuted intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am 1989;71:839-47. [Crossref] [PubMed]
- Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg Am 1991;16:375-84. [Crossref] [PubMed]
- Mehta JA, Bain GI, Heptinstall RJ. Anatomical reduction of intra-articular fractures of the distal radius. An arthroscopically-assisted approach. J Bone Joint Surg Br 2000;82:79-86. [Crossref] [PubMed]
- Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am 1994;19:325-40. [Crossref] [PubMed]
- Rogachefsky RA, Lipson SR, Applegate B, et al. Treatment of severely comminuted intra-articular fractures of the distal end of the radius by open reduction and combined internal and external fixation. J Bone Joint Surg Am 2001;83-A:509-19. [Crossref] [PubMed]
- Catalano LW 3rd, Cole RJ, Gelberman RH, et al. Displaced intra-articular fractures of the distal aspect of the radius. Long-term results in young adults after open reduction and internal fixation. J Bone Joint Surg Am 1997;79:1290-302. [Crossref] [PubMed]
- Goldfarb CA, Rudzki JR, Catalano LW, et al. Fifteen-year outcome of displaced intra-articular fractures of the distal radius. J Hand Surg Am 2006;31:633-9. [Crossref] [PubMed]
- Varitimidis SE, Basdekis GK, Dailiana ZH, et al. Treatment of intra-articular fractures of the distal radius: fluoroscopic or arthroscopic reduction? J Bone Joint Surg Br 2008;90:778-85. [Crossref] [PubMed]
- Tang JB, Shi D, Gu YQ, et al. Can cast immobilization successfully treat scapholunate dissociation associated with distal radius fractures? J Hand Surg Am 1996;21:583-90. [Crossref] [PubMed]
- Mrkonjic A, Lindau T, Geijer M, et al. Arthroscopically diagnosed scapholunate ligament injuries associated with distal radial fractures: a 13- to 15-year follow-up. J Hand Surg Am 2015;40:1077-82. [Crossref] [PubMed]
- Gunal I, Ozaksoy D, Altay T, et al. Scapholunate dissociation associated with distal radius fractures. Eur J Orthop Surg Traumatol 2013;23:877-81. [Crossref] [PubMed]
- Lindau T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of the radius in young adults. A descriptive arthroscopic study in 50 patients. J Hand Surg Br 1997;22:638-43. [Crossref] [PubMed]
- Peicha G, Seibert F, Fellinger M, et al. Midterm results of arthroscopic treatment of scapholunate ligament lesions associated with intra-articular distal radius fractures. Knee Surg Sports Traumatol Arthrosc 1999;7:327-33. [Crossref] [PubMed]
- Ruch DS, Vallee J, Poehling GG, et al. Arthroscopic reduction versus fluoroscopic reduction in the management of intra-articular distal radius fractures. Arthroscopy 2004;20:225-30. [Crossref] [PubMed]
- Abe Y, Yoshida K, Tominaga Y. Less invasive surgery with wrist arthroscopy for distal radius fracture. J Orthop Sci 2013;18:398-404. [Crossref] [PubMed]
- Wright TW, Del Charco M, Wheeler D. Incidence of ligament lesions and associated degenerative changes in the elderly wrist. J Hand Surg Am 1994;19:313-8. [Crossref] [PubMed]
- Akahane M, Ono H, Nakamura T, et al. Static scapholunate dissociation diagnosed by scapholunate gap view in wrists with or without distal radius fractures. Hand Surg 2002;7:191-5. [Crossref] [PubMed]
- Lindau T. Wrist arthroscopy in distal radial fractures using a modified horizontal technique. Arthroscopy 2001;17:E5 [Crossref] [PubMed]
- Weiss AP, Sachar K, Glowacki KA. Arthroscopic debridement alone for intercarpal ligament tears. J Hand Surg Am 1997;22:344-9. [Crossref] [PubMed]
- Smeraglia F, Del Buono A, Maffulli N. Wrist arthroscopy in the management of articular distal radius fractures. Br Med Bull 2016;119:157-65. [Crossref] [PubMed]
- Doi K, Hattori Y, Otsuka K, et al. Intra-articular fractures of the distal aspect of the radius: arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am 1999;81:1093-110. [Crossref] [PubMed]
- Yamazaki H, Uchiyama S, Komatsu M, et al. Arthroscopic assistance does not improve the functional or radiographic outcome of unstable intra-articular distal radial fractures treated with a volar locking plate: a randomised controlled trial. Bone Joint J 2015;97-B:957-62. [Crossref] [PubMed]
- Zemirline A, Taleb C, Facca S, et al. Minimally invasive surgery of distal radius fractures: a series of 20 cases using a 15mm anterior approach and arthroscopy. Chir Main 2014;33:263-71. [Crossref] [PubMed]
- Del Piñal F, Klausmeyer M, Moraleda E, et al. Arthroscopic reduction of comminuted intra-articular distal radius fractures with diaphyseal-metaphyseal comminution. J Hand Surg Am 2014;39:835-43. [Crossref] [PubMed]
- Del Piñal F. Technical tips for (dry) arthroscopic reduction and internal fixation of distal radius fractures. J Hand Surg Am 2011;36:1694-705. [Crossref] [PubMed]
- Aïm F, Klouche S, Frison A, et al. Efficacy of vitamin C in preventing complex regional pain syndrome after wrist fracture: A systematic review and meta-analysis. Orthop Traumatol Surg Res 2017;103:465-70. [Crossref] [PubMed]
Cite this article as: Shkolnikova J, Harvey J. Wrist arthroscopy in the management of distal radius fractures. Ann Joint 2018;3:77.