
Anatomic double-bundle anterior cruciate ligament reconstruction using soft tissue interference screw fixation
Introduction
Anterior cruciate ligament (ACL) has at least two bundles, an anteromedial (AM) bundle and a posterolateral (PL) bundle (1). These bundles act separately during the range of the motion of the knee, so that at extended knee, the PL bundle is tight and the AM bundle is lax, and at flexed knee it is opposite (2). An anatomic double-bundle ACL reconstruction can more closely mimic this phenomenon and restore normal kinematics to the knee when compared with a single-bundle technique in a cadaver model (3).
On the 27 prospective randomized trials comparing the clinical results of double-bundle versus single-bundle techniques, 8 trials (30%) did not find any significant differences in the clinical results between these two techniques (4-11). However, 19 trials (70%) reported significantly better results with double-bundle technique than with single-bundle technique (12-30). There were differences in favour of double-bundle technique both at objective and subjective findings of the patients, and no study reported the superiority of single-bundle technique.
Most of the above noted studies have used cortical fixation for the graft fixation, which may not be as anatomic as the aperture fixation (31). With interference screws, the anatomical aperture fixation can be easily achieved. The advantage of using bioabsorbable interference screws is that they do not interfere the magnetic resonance imaging (MRI) techniques afterwards. They have been shown to provide even stronger fixation than metal screws (32,33), although slow absorption of some materials are reported (34).
The purpose of this review is to introduce the technique and results of the anatomic double-bundle ACL reconstruction with bioabsorbable interference screw fixation comparing to the single-bundle ACL reconstruction with interference screw fixation during the past 15 years we have used these techniques. Our techniques have not changed during these years.
Surgical technique of the anatomic double-bundle ACL reconstruction
The surgical technique of the double-bundle method has been described earlier in detail by Järvelä (16). In brief, a complete diagnostic arthroscopy of the knee is performed first to ensure the ACL tear and other possible findings inside the injured knee. The standard anterolateral arthroscopic portal is established adjacent to the lateral patella tendon border at the level of inferior pole of the patella. Accordingly, the standard AM portal is placed adjacent to the medial patella tendon border, but about 1 cm below the anterolateral border. The ruptured ACL is examined with an arthroscopic probe, dissected, and debrided. The tibial footprint of the ACL is left intact. Also, the anatomical footprints of the AM and PL bundles of the ACL on the lateral wall of the intercondylar notch are identified. A bony notchplasty is not performed.
The AM femoral tunnel is drilled first using the AM portal and a free-hand technique without a guide. The AM femoral tunnel is placed as posterior as possible, without breaking the posterior wall of the femoral condyle, in the posterior part of the intercondylar notch on the lateral wall of the notch. The tunnel is first marked with a 30 degrees awl with the knee at 90 degrees of flexion, and then drilled with a guide pin through the femoral condyle at 120 degrees flexion of the knee. The cannulated drill is used for the final drilling of the tunnel (diameter of 4 mm). The final drilling of the tunnel is made after harvesting and measuring the diameter of the hamstring autografts. The diameter of the AM femoral tunnel is typically 7 mm, and the depth of the tunnel is 30 mm.
The PL femoral tunnel is drilled using also the AM portal and a free-hand technique. The anatomical femoral footprint of the PL bundle is identified arthroscopically and marked with a 30 degrees awl, as described above. If the PL femoral footprint is difficult to identify, as it sometimes can be in a chronic case, the PL femoral tunnel is placed as closed as possible to the AM femoral tunnel, without breaking the wall between these tunnels. The PL femoral tunnel is located anteriorly and inferiorly from the AM femoral tunnel in flexion position. The drilling of the PL femoral tunnel is performed the knee in 90 degrees of flexion. The diameter of the PL femoral tunnel is 6 mm, and the depth of the tunnel is 30 mm. The wall between these two tunnels (AM and PL) in femoral side has to be at least 1–2 mm. Otherwise, the inside-out fixation with bioabsorbable interference screws is not possible.
On the tibial side, tibial guide is used when creating the tibial tunnels. An ACL tibial drill guide is placed on the AM aspect of the ACL tibial footprint. The starting point of the AM tibial tunnel is the same as in standard ACL single bundle technique. Once acceptable placement of the AM tibial pin is obtained (no impingement in the knee extension), the PL tibial guide wire is placed on the PL aspect of the ACL tibial footprint. The PL tibial tunnel has a more medial starting point on the tibial cortex than standard ACL tibial tunnel. An osseous bridge of 1–2 cm remained on the tibial cortex between these tunnels. The AM tibial tunnel is drilled first followed by the PL tunnel. The diameter of the AM tibial tunnel is typically 7 mm, and that of PL tunnel 6 mm.
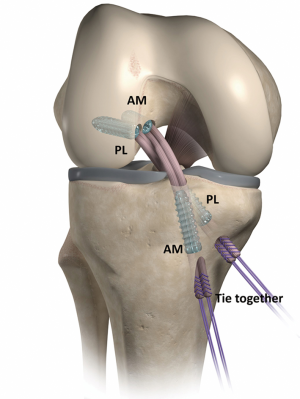
The hamstring grafts are harvested from the same leg and doubled or tripled depending of the diameters of the tendons. Grafts are inserted in a retrograde manner through the tibial tunnels and fixed with bioabsorbable interference screws (D-lactide, L-lactide, and trimethylene carbonate, Hexalon; Inion Company, Tampere, Finland) with an inside-out technique in the femur and an outside-in manner in the tibia. The PL graft (doubled or tripled gracilis tendon autograft) is passed first, and fixed with the above noted bioabsorbable screw. The diameter of the screw is 6 mm, and the length of the screw is 25 mm. Then the graft for AM bundle (doubled semitendinosus tendon autograft) is passed and fixed with a same technique as described above. The diameter of the screw is usually 7 mm at the AM bundle fixation, and the length of the screw is 25 mm. On the tibial side, the PL bundle is tensioned by pulling with a hand and fixed first the knee at full extension, followed by the AM bundle at 30 degrees of flexion of the knee with tensioning by pulling with a hand. Bioabsorbable interference screw are used for the fixation on the tibial side, too. The diameter of the screw is typically 7 mm in the PL tunnel, and 8 mm in the AM tunnel, and the length of the screw is 30 mm. An additional fixation is made with the nonabsorbable sutures coming from each graft to tie them together over the cortical bone bridge between the tibial tunnels (Figure 1). The above noted bioabsorbable screws were introduced already in 2002. Since that we have inserted more than 5,000 of these screws into the knees of the patients and only one screw breakage has been occurred during the screw insertion. With this particular patient, the screw driver broke first, and that was the reason for the screw breakage.
Surgical technique of the single-bundle ACL reconstruction
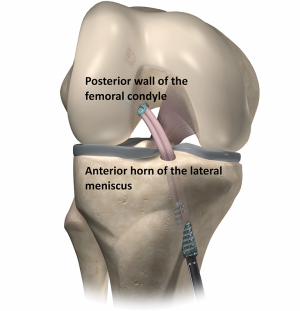
A diagnostic arthroscopic procedure and debridement are performed first as described above. The femoral tunnel is drilled through an AM portal as posterior as possible without breaking the posterior wall of the femur with a free-hand technique on the lateral wall of the notch in the same manner as described above when doing AM femoral tunnel. The tibial tunnel is made with a tibial guide in the middle of the ACL tibial footprint at the level of anterior horn of the lateral meniscus. The semitendinosus and gracilis tendons are harvested, doubled, and inserted through the tibial tunnel and into the femur and fixed with interference screws as described above when making the fixation for the AM bundle. The diameter of the 4-stranded hamstring autograft is typically 8 mm. Tunnel size is the same as the diameter of the graft (typically 8 mm). The diameter of the screw is 8 mm in the femoral side and 8–9 mm in the tibial side. The length of the screw is 25 mm in the femoral side, and 30 mm in the tibial side. No additional fixation is used with single-bundle technique (Figure 2).
Postoperative rehabilitation
Immediate full weightbearing and full range of motion is permitted. No brace is used. Crutches are used for 3 to 4 weeks. Closed kinetic chain exercises are started immediately postoperatively. Cycling with an ergometer bicycle is permitted at 2 to 3 weeks, running at 3 to 4 months, and pivoting sports at 6 to 8 months postoperatively, provided that the patient has regained full functional stability and muscle performance. If meniscal repair is performed during the same operative procedure, range of motion is recommended from 0 to 90 degrees for the first 4 to 6 weeks.
Results
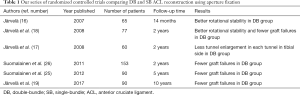
We started a prospective randomized clinical trial comparing anatomic double-bundle versus single-bundle ACL reconstruction already 15 years ago (Table 1). At the 14-month follow-up, the patients in the double-bundle group had significantly better rotational stability than the patients in the single-bundle group (16).
Full table
At the 2-year follow-up, the rotational stability was still the best among the patients with double-bundle ACL reconstruction. Also, the patients with the double-bundle ACL reconstruction had significantly fewer graft failures leading to revision ACL surgery than the patients with the single-bundle procedure (18). MRI evaluation at 2 years showed that there was less tunnel enlargement in each tunnel the tibial side in the patients with the double-bundle ACL reconstruction than in the patients with the single-bundle technique (17). In this study, bone tunnel enlargement was assessed digitally by measuring the widths of the bone tunnels perpendicular to the long axis of the tunnels on an oblique coronal and sagittal plane. The MRI were interpreted by consensus by two musculoskeletal radiologists who were unaware of the patients’ clinical data. The anteroposterior and mediolateral diameters of the femoral and tibial tunnels were measured 2 cm from the articular surface of the knee joint, and a mean of these two measurements was recorded. The measurements were repeated in 20 randomly chosen patients after 2 months, and the intraobserver differences were evaluated. The MRI data at follow-up were compared with the intraoperatively documented drill diameters. Changes in tunnel size were calculated in millimeters and as a percentage of the diameter of the drill size used at surgery. In another MRI study, tunnel communication was seen in the femur in 10% of patients and in the tibia in 27% of the patients, although no statistically significant association between the MRI findings of tunnel communication and knee laxity was found (35). In addition, MRI evaluation at 2 years showed that the patients with the single-bundle procedure had significantly more invisible grafts than the patients with the double-bundle procedure, although no revision ACL surgery was performed for them so far (26). Further analysis of the patients with the double-bundle ACL reconstruction showed that the graft disruption was seen only in 3% of AM grafts and 6% of PL grafts at 2 years. Both grafts were disrupted only in 3% of the patients (36). The locations of the grafts were determined with MRI at the 2-year follow-up by a musculoskeletal radiologist both in patients with the double-bundle ACL reconstruction and in patients with the single-bundle ACL reconstruction, and they were all at the anatomic zone of insertion sites of the ACL (37,38).
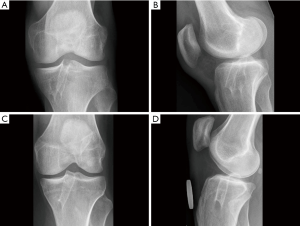
At the 5-year follow-up, there was no significant difference in the rotational stability of the knee anymore. However, the patients with the single-bundle ACL reconstruction had significantly more graft failures leading to the revision ACL surgery than the patients with the double-bundle technique. At 5 years, the x-rays showed no significant differences at osteoarthritic rates between the patients with the single-bundle and the double-bundle procedures (25). The MRI evaluation in the patients with the double-bundle ACL reconstruction showed that the tunnel enlargement seen at 2 years was followed by tunnel narrowing at 5-year follow-up. Tunnel ossification resulted in evenly narrowed tunnels in 44%, in conical tunnels in 48%, and fully ossified in 8%. At 5 years, none of the bioabsorbable screws was anymore completely visible, and 19% of them were already fully ossified (Figure 3) (39).
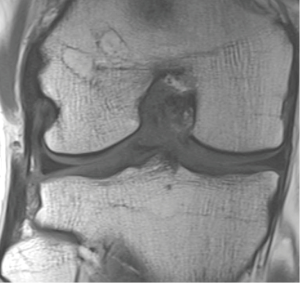
At the 10-year follow-up, the double-bundle technique resulted in significantly fewer graft failures than the single-bundle ACL reconstruction during the follow-up. Knee stability and osteoarthritic rates were similar at 10 years (Figure 4) (19).
Discussion
The main finding of our prospective randomized trial was that at the beginning the rotational stability was significantly better in patients with the anatomic double-bundle ACL reconstruction comparing to the patients with the single-bundle procedure (16,18). Also, the single-bundle ACL reconstruction resulted in significantly more graft failures during the 10-year follow-up than the double-bundle ACL surgery (18,19,25,26). At the 10-year follow-up, only one patient out of 30 patients had graft failure with the double-bundle technique leading up to revision ACL surgery, while with the single-bundle procedures ten patients out of 60 patients had revision ACL surgery because of the graft failure. In addition, the one patient with the double-bundle ACL failure had a severe trauma in causing the graft failure, because he fell from the roof while working and had bony fractures, too. The ten patients with an ACL failure with the single-bundle technique had only minor trauma in causing the graft failure.
The reason why the double-bundle ACL is stronger and more durable may be the fact that the double-bundle ACL is more anatomic than the single-bundle ACL. It mimics the normal anatomy of the ACL more closely than the single-bundle one. In the double-bundle technique, each bundle act separately during the range of motion of the knee creating the crossing pattern of these bundles, as they do in the original ACL, too (2). This is something we cannot create with a single-bundle technique. Also, the double-bundle graft is thicker than the single-bundle graft. In our study, usually the thickness of the AM-bundle was 7 mm, and that of the PL-bundle 6 mm. So, together the thickness of the double-bundle graft was about 13 mm, while the thickness of the single-bundle graft was usually only 7 to 8 mm. In addition, in the double-bundle technique, we used four interference screws for the fixation, while in the single-bundle technique only two interference screws were used. All these factors could explain the superiority of the double-bundle ACL comparing to the single-bundle ACL even at the 10-year follow-up.
In the past, the use of the bioabsorbable screws for the graft fixation had poor reputation, because they could break during insertion (40,41). Also, they could cause some tissue reactions during the absorption, and absorb either too fast or too slow (34,42-45). Each polymer has its material-specific properties. For example, polyglycolic acid is strong but very fast to absorb, poly-L-lactid acid is strong but brittle and slow to absorb, whereas trimethylene carbonate is rather weak but elastic like rubber. By blending these polymers, it is possible to create materials which are strong, unbreakable during the insertion, and will absorb without causing any tissue reactions.
The bioabsorbable screws made of bioabsorbable copolymers composed of L-lactic acid, D-lactid acid, and trimethylene carbonate (Hexalon, Inion Company, Tampere, Finland) and used in our trial was introduced already in 2002. Since that we have inserted more than 5,000 of these screws into the knees of the patients without any major problems. According to sheep study, this copolymer blend fully absorbs in 2 years in vivo without causing any clinically significant inflammatory, foreign body, or other tissue reactions (46). At our MRI evaluations with patients, it seems that these bioabsorbable screws are fully absorbed in 2 to 5 years, and even actually finally replaced by bone at 5 years in 19% of the cases (39). Tunnel cysts are frequent MRI findings at 5 years, but they are not associated with adverse clinical evaluation results. Tunnel cysts may be a natural course of the bioabsorbable screw absorption and ossifying process, because the screw cannot be replaced by bone before it has absorbed.
Conclusions
According to our prospective, randomized trial, the anatomic double-bundle ACL reconstruction with bioabsorbable interference screw fixation resulted in significantly better clinical results than the single-bundle ACL reconstruction during the 10-year follow-up. At the beginning, the rotational stability was better with the double-bundle technique, and during the years fewer graft failures leading to ACL revision surgery was found with the double-bundle procedure. The double-bundle ACL reconstruction is stronger and more durable than the single-bundle ACL reconstruction even at the 10-year follow-up. The bioabsorbable interference screws used for the graft fixation seem to absorb totally in 2 to 5 years, and finally replace by bone after the screws have absorbed. No adverse effects related to these screws were found during the 10-year follow-up.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Takeshi Muneta) for the series “Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.10.04). The series “Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop 1975;216-31. [Crossref] [PubMed]
- Amis AA, Dawkins GP. Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br 1991;73:260-7. [Crossref] [PubMed]
- Yagi M, Wong EK, Kanamori A, et al. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 2002;30:660-6. [Crossref] [PubMed]
- Adachi N, Ochi M, Uchio Y, et al. Reconstruction of the anterior cruciate ligament: single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br 2004;86:515-20. [Crossref] [PubMed]
- Araki D, Kuroda R, Kubo S, et al. A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop 2011;35:439-46. [Crossref] [PubMed]
- Fujita N, Kuroda R, Matsumoto T, et al. Comparison of the clinical outcome of double-bundle, anteromedial single-bundle, and posterolateral single-bundle anterior cruciate ligament reconstruction using hamstring tendon graft with minimum 2-year follow-up. Arthroscopy 2011;27:906-13. [Crossref] [PubMed]
- Kang HJ, Wang XJ, Wu CJ, et al. Single-bundle modified patellar tendon versus double-bundle tibialis anterior allograft ACL reconstruction: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 2015;23:2244-9. [Crossref] [PubMed]
- Núñez M, Sastre S, Núñez E, et al. Health-related quality of life and direct costs in patients with anterior cruciate ligament injury: single-bundle versus double-bundle reconstruction in a low-demand cohort. A randomized trial with 2 years of follow-up. Arthroscopy 2012;28:929-35. [Crossref] [PubMed]
- Sastre S, Popescu D, Nunez M, et al. Double-bundle versus single-bundle ACL reconstruction using thehorizontal femoral position: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 2010;18:32-6. [Crossref] [PubMed]
- Streich NA, Friedrich K, Gotterbarm T, et al. Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc 2008;16:232-8. [Crossref] [PubMed]
- Wang JQ, Ao YF, Yu CL, et al. Clinical evaluation of double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: a prospective, randomized and controlled study. Chin Med J (Engl) 2009;122:706-11. [PubMed]
- Aglietti P, Giron F, Cuomo P, et al. Single- and double-incision double-bundle ACL reconstruction. Clin Orthop Relat Res 2007;108-13. [Crossref] [PubMed]
- Aglietti P, Giron F, Losco M, et al. Comparison between single- and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized single-blinded clinical trial. Am J Sports Med 2010;38:25-34. [Crossref] [PubMed]
- Hussein M, van Eck CF, Cretnik A, et al. Prospective, randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med 2012;40:512-20. [Crossref] [PubMed]
- Ibrahim SA, Hamido F, Al Mister AK, et al. Anterior cruciate ligament reconstruction using autologous hamstring double bundle graft compared with single bundle procedures. J Bone Joint Surg Br 2009;91:1310-5. [Crossref] [PubMed]
- Järvelä T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 2007;15:500-7. [Crossref] [PubMed]
- Järvelä T, Moisala AS, Paakkala T, et al. Tunnel enlargement after double-bundle anterior cruciate ligament reconstruction: a prospective, randomized study. Arthroscopy 2008;24:1349-57. [Crossref] [PubMed]
- Järvelä T, Moisala AS, Sihvonen R, et al. Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: prospective, randomized clinical study with 2-year results. Am J Sports Med 2008;36:290-7. [Crossref] [PubMed]
- Järvelä S, Kiekara T, Suomalainen P, et al. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 10-year results. Am J Sports Med 2017;45:2578-85. [Crossref] [PubMed]
- Koga H, Muneta T, Yagishita K, et al. Mid-to long-term results of single-bundle versus double-bundle anterior cruciate ligament reconstruction: randomized controlled trial. Arthroscopy 2015;31:69-76. [Crossref] [PubMed]
- Lee S, Kim H, Jang J, et al. Comparison of anterior and rotatory laxity using navigation between single- and double-bundle ACL reconstruction: prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 2012;20:752-61. [Crossref] [PubMed]
- Mayr HO, Benecke B, Hoell A, et al. Single-bundle versus double-bundle anterior cruciate ligament reconstruction; a comparative2-year follow-up. Arthroscopy 2016;32:34-42. [Crossref] [PubMed]
- Muneta T, Koga H, Mochizuki T, et al. A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 2007;23:618-28. [Crossref] [PubMed]
- Siebold R, Dehler C, Ellert T. Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 2008;24:137-45. [Crossref] [PubMed]
- Suomalainen P, Järvelä T, Paakkala A, et al. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med 2012;40:1511-8. [Crossref] [PubMed]
- Suomalainen P, Moisala AS, Paakkala A, et al. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: randomized clinical and magnetic resonance imaging study with 2-year follow-up. Am J Sports Med 2011;39:1615-22. [Crossref] [PubMed]
- Yagi M, Kuroda R, Nagamune K, et al. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res 2007;100-7. [Crossref] [PubMed]
- Zaffagnini S, Bruni D, Marcheggiani Muccioli G, et al. Single-bundle patellar tendon versus non-anatomical double-bundle hamstring ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc 2011;19:390-7. [Crossref] [PubMed]
- Zaffagnini S, Bruni D, Russo A. ST/G ACL reconstruction: double strand plus extra-articular sling vs double bundle, randomized study at 3-year follow-up. Scand J Med Sci Sports 2008;18:573-81. [Crossref] [PubMed]
- Zhang Z, Gu B, Zhu W, et al. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomized study with 2-year follow-up. Eur J Orthop Surg Traumatol 2014;24:559-65. [Crossref] [PubMed]
- Fu FH, Bennett CH, Ma CB, et al. Current trends in anterior cruciate ligament reconstruction. Part II. Operative procedures and clinical correlations. Am J Sports Med 2000;28:124-30. [Crossref] [PubMed]
- Kousa P, Järvinen TL, Vihavainen M, et al. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part I: femoral site. Am J Sports Med 2003;31:174-81. [Crossref] [PubMed]
- Kousa P, Järvinen TL, Vihavainen M, et al. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part II: tibial site. Am J Sports Med 2003;31:182-88. [Crossref] [PubMed]
- Ma CB, Francis K, Towers J, et al. Hamstring anterior cruciate ligament reconstruction: a comparison of bioabsorbable interference screw and endobutton-post fixation. Arthroscopy 2004;20:122-8. [Crossref] [PubMed]
- Kiekara T, Järvelä T, Huhtala H, et al. Tunnel communication and increased graft signal intensity on magnetic resonance imaging of double-bundle anterior cruciate ligament reconstruction. Arthroscopy 2014;30:1595-601. [Crossref] [PubMed]
- Kiekara T, Järvelä T, Huhtala H, et al. MRI of double-bundle ACL reconstruction: evaluation of graft findings. Skeletal Radiol 2012;41:835-42. [Crossref] [PubMed]
- Suomalainen P, Moisala AS, Paakkala A, et al. Comparison of tunnel placements and clinical results of single-bundle anterior cruciate ligament reconstruction before and after starting the use of double-bundle technique. Knee Surg Sports Traumatol Arthrosc 2013;21:646-53. [Crossref] [PubMed]
- Kiekara T, Järvelä T, Huhtala H, et al. MRI evaluation of the four tunnels of double-bundle ACL reconstruction. Acta Radiol 2014;55:579-88. [Crossref] [PubMed]
- Kiekara T, Paakkala A, Suomalainen P, et al. Femoral and tibial tunnel diameter and bioabsorbable screw findings after double-bundle ACL reconstruction in 5-year clinical and MRI follow-up. Orth J Sports Med 2017:2:5:2325967116685525.
- Costi JJ, Kelly AJ, Hearn TC, et al. Comparison of torsional strengths of bioabsorbable screws for anterior cruciate ligament reconstruction. Am J Sports Med 2001;29:575-80. [Crossref] [PubMed]
- Smith CA, Tennent TD, Pearson SE, et al. Fracture of Bilok interference screws on insertion during anterior cruciate ligament reconstruction. Case report. Arthroscopy 2003;19:E115-17. [Crossref] [PubMed]
- Andriano KP, Pohjonen T, Tormala P. Processing and characterization of absorbable polylactide polymers for use in surgical implants. J Appl Biomater 1994;5:133-40. [Crossref] [PubMed]
- Böstman OM, Pihlajamäki HK. Adverse tissue reactions to bioabsorbable fixation devices. Clin Orthop 2000;216-27. [Crossref] [PubMed]
- Bergsma JE, de Bruijn WC, Rozema FR, et al. Late degradation tissue response to poly(L-lactide) bone plates and screws. Biomaterials 1995;16:25-31. [Crossref] [PubMed]
- Böstman O, Pihlajamäki H. Clinical biocompatibility of biodegradable orthopaedic implants for internal fixation: a review. Biomaterials 2000;21:2615-21. [Crossref] [PubMed]
- Nieminen T, Rantala I, Hiidenheimo I, et al. Degradative and mechanical properties of a novel resorbable plating system during a 3-year follow-up in vivo and in vitro. J Mater Sci Mater Med 2008;19:1155-63. [Crossref] [PubMed]
Cite this article as: Järvelä T, Nurmi JT, Järvelä S. Anatomic double-bundle anterior cruciate ligament reconstruction using soft tissue interference screw fixation. Ann Joint 2018;3:86.


