
Posterolateral corner repair and reconstruction: overview of current techniques
Introduction
The posterolateral corner (PLC) of the knee is the primary stabilizer to varus and external rotation, and it also acts as a secondary stabilizer to posterior tibial translation. The three main structures of this complex are: the lateral (fibular) collateral ligament (LCL), the popliteofibular ligament (PFL) and the popliteus tendon (PT). PLC knee injuries may lead to chronic pain, instability, and surgical failure of cruciate ligament reconstructions, when not properly addressed, by biomechanical overloading (1-10).
The treatment of PLC knee injuries has always been a challenging topic (4,6,11-15). Due to the low healing capacity of PLC injuries, surgery is usually indicated in most cases, while the non-operative treatment is reserved for isolated PLC injuries involving minor abnormal varus (up to 5 mm) and/or external rotation laxity (up to 5°).
Repair versus reconstruction
Repair of the injured structures was historically applied to acute cases; however, due to the higher failure rate in comparison to reconstructions (40% versus 6% in one cohort and 37% versus 9% in another cohort), the end-to-end isolated midsubstance repair is not currently recommended (16,17). Although this type of repair can still be used, it must be augmented by a reconstruction of the injured structures.
Presently, the recommended repairs are the ones involving avulsions, especially of structures torn off the fibular head (like the LCL, the PFL and the biceps tendon) or PT, that shall be reattached to the bone, and the ones involving the capsule and the lateral meniscocapsular ligaments that are anchored and sutured to the underlying bone (18). Repair of bone avulsions have a better healing potential than soft tissue avulsions and must be reattached to its insertion site.
Acute cases surgical treatment
Acute treated cases should have a mean time to surgery of <4 weeks. Acute treated cases tend to obtain better results than chronic ones, so the surgical treatment, ideally, should not be delayed more than 10 days to allow some soft tissue and capsule healing, lowering the risk of fluid extravasation during arthroscopy to address concomitant cruciate injuries. In such cases, some arthroscopy steps should be performed “dry” (without saline, just using the camera visualization). These cautions are intended to avoid compartment syndrome (4,13,14).
It is easier to identify the remnants of the torn structures in the acute setting in comparison to the chronic one because there is no important scar tissue formation. This identification is important, as the treatment of choice for acute PLC lesions involves the repair of avulsions of the PLC structures (fibular head, PT, lateral capsule, lateral meniscocapsular ligaments) reattaching them to its anatomical site (Figure 1) combined with the reconstruction of midsubstance tears of these injured structures. This hybrid approach, involving repair and reconstruction, is related to improve subjective outcomes and objective stability (14,18).

Chronic cases surgical treatment
Chronic PLC injured patients must first be evaluated for lower limb alignment with a full-length lower limb radiography. A proximal tibial opening-wedge corrective osteotomy must be considered if the lower limb mechanical axis (a line from the center of the femoral head to the center of the ankle mortise) passes medial to the apex of the medial tibial eminence and is mandatory if the patient presents double or triple varus (19,20). The weigh-bearing axis must be corrected to neutral. If the patient continues to have symptoms of instability at a minimum of three months after the osteotomy site had healed, it is performed a PLC reconstruction combined with anterior cruciate ligament (ACL) reconstruction or posterior cruciate ligament (PCL) reconstruction or both (14,20,21). Interestingly, 38% of the patients do not have symptoms of instability after the realignment osteotomy and do not require ligament reconstructions (20).
In the chronic setting, PLC injuries in patients with neutral or valgus alignment are addressed by reconstruction (4,6,14,15,21,22).
Types of reconstruction
After some studies demonstrated a high failure rate with primary repair, a trend toward reconstruction of the PLC has occurred (16,17). Early reconstruction techniques for PLC injuries applied a single femoral fixation site and a fibular sling (23). This technique evolved to two femoral tunnels with a fibular sling attempting to better reproduce the anatomy of the PLC (24). Both reconstructions reproduce just two of the three main structures of the PLC, the LCL and the PFL. Biomechanical studies comparing them showed improved results favoring the more anatomic two femoral tunnels reconstruction (25,26). An interesting technique, derived from the single femoral fixation site technique, despite being non-anatomic, is worth mentioning as it allows the combined reconstruction of the ACL and PLC with a single femoral tunnel (27,28).
LaPrade et al., in 2004, introduced the term anatomical reconstruction of the PLC of the knee, based on previous anatomic and biomechanical testing, surgically reproducing the three main structures of this complex: the LCL, the PFL and the PT (2). Based on this biomechanical validated data, the authors believe the term anatomical PLC reconstruction should be reserved for the techniques reproducing the three main structures of the PLC and its anatomic footprints (2,5,6,29). In addition, it has been demonstrated that an anatomic PLC reconstruction requires a PFL reconstruction through a tibial tunnel (30). Consequently, the term non-anatomical, should be applied to the techniques that do not reproduce the aforementioned three main structures and also for the techniques that try to reproduce them non-anatomically by single femoral fixation site or other non-anatomic attachments (23,24,27,31-35) (Tables 1,2).

Full table

Full table
Despite a majority of studies presenting similar results comparing non-anatomic to anatomic PLC reconstructions, it is important to note that some biomechanical and clinical studies present superior results favoring anatomical PLC reconstructions (3,30,31,36-38). Also, certain conditions, such as concurrent proximal tibiofibular instability or an asymmetric knee hyperextension are relative contraindications to non-anatomic fibular based PLC reconstructions requiring a more anatomic tibial based two tailed PLC reconstruction that is a technique which relies both on a fibular head and a tibial tunnel (1,6).
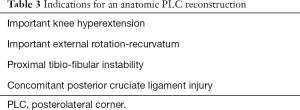
Regarding the biomechanical superiority and rational, the authors believe some conditions are indicative of an anatomic reconstruction over a non-anatomic one (6) (Table 3).
Full table
PLC
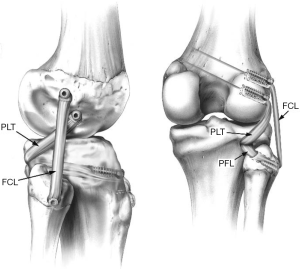
Most of the validated PLC reconstructions that intend to reproduce its three main structures rely on allografts or have to harvest the semitendinosus from both knees due to graft length issues (2,5,27,29,33,35). The authors, when allografts are available, prefer to use the LaPrade et al., 2004 technique as it is biomechanically validated and has improved clinical outcomes reported (21,30) (Figure 2).
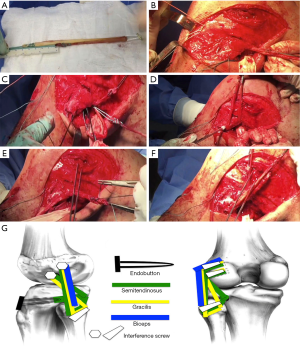
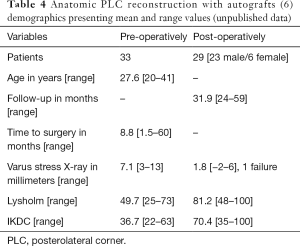
In the setting of unavailable allografts, the first author has preference to use the Franciozi et al., 2018 technique as it anatomically reproduces the three main structures of the posterolateral aspect of the knee using autografts. This technique provides anatomical PLC reconstruction using autografts as the semitendinosus graft is artificially lengthened by the loop of the suspensory fixation device, surpassing the need of longer allografts to do so (6). It relies just on a semitendinosus and a gracilis autografts, augmented by the posterior half of the biceps, when necessary, avoiding the need of contra-lateral side knee autografts. This technique is an important new resource because Tissue Banks are not available in some countries and regions, in addition to allograft cost issues. Also, this technique had successful improved subjective outcomes and restored objective stability in varus, external rotation and recurvatum in knees with a chronic PLC injury (unpublished data) (Figure 3, Table 4).
Full table
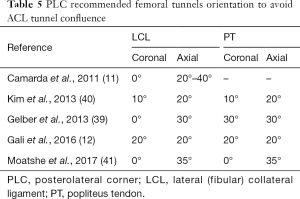
The presented modified LaPrade technique, despite the similarities with the original, has some important issues to be addressed. The first one is related to the femoral tunnels. Because they are not blind holes, the chances of tunnel confluence are higher, mainly with combined ACL procedures and a 0–20° anterior and 20–35° proximal orientation of the LCL femoral insertion tunnel, in addition to a 20–35° anterior and 0–30° proximal orientation of the PT femoral insertion must be respected (11,12,39-41) (Table 5). The next issue is the biceps augmentation in the scenario of a fibular tip avulsion where the reinsertion must be resistant and reliable in order to use this augmentation, being recommended strong fixation in full extension with anchors or through a bone tunnel, similar to a cerclage, distal to the fibular tunnel intended for graft passage.
Full table
Tips to improve plc surgical treatment outcomes
The authors recommend that an anatomic PLC knee reconstruction shall be performed in patients with PLC injury to best improve clinical and functional outcomes, especially in the setting of grade III PLC injuries (6,14,15,21).
Since identification and graduation of PLC injuries can be tricky, especially at the multiple ligament injured knee, stress X-rays are an objective and reliable method to help objectively assess these injuries (42,43).
PLC injuries are frequently associated with PCL injuries. The treatment of one influences over another as both structures act as secondary stabilizers to each other. In order to optimize surgical results, the surgeon should perform a double bundle PCL reconstruction due to its biomechanical advantage over PCL single bundle reconstruction (44). To do so, access to sufficient and adequate grafts to address all the ligament injuries is necessary as well as proficiency in multi-ligament knee surgeries, as this technique is more demanding than single bundle PCL reconstruction.
If the surgeon intends to perform a concomitant single bundle PCL reconstruction, a lateral tibial tunnel entry point can be utilized instead the medial tibial tunnel entry point as it is more effective to resist posterior translation and safer to avoid popliteal artery injury (45,46).
Graft tensioning and fixation sequence
Restoring the native tibiofemoral orientation and associated knee kinematics in the setting of a multiple knee ligaments reconstruction is a current hot topic involving knee dislocations. In a one-stage ACL and PCL reconstruction, applying tension to one graft changes the tension of the other and displaces the tibia relative to the femur before and after graft fixation as both graft tensions are interrelated. Mal-positioning of the tibia at the final graft fixation may lead to non-anatomic tibiofemoral orientation and badly influence knee kinematics (47,48).
A recent study evaluating multiple ligament reconstruction in an ACL, PCL and PLC deficient knee, applying manual reduction to obtain the normal step-off position of the tibiofemoral articulation, showed that tensioning the PLC first in a bicruciate knee ligament reconstruction with concurrent PLC reconstruction should be avoided because it significantly increased tibial internal rotation. It recommends that the PCL should be tensioned and fixed first (at 90° for the anterolateral bundle, reducing the knee manually to the normal step-off position of the tibiofemoral articulation, and at full extension for the posteromedial bundle), followed by the ACL near full extension, and that the PLC should be tensioned last (fixation of the FCL at 30° of knee flexion applying a valgus force, followed by the remaining PLC structures at 60° of flexion and neutral rotation) (48).
Another recent study also evaluated bicruciate ligament reconstruction graft tensioning sequence using a simultaneous tensioning protocol. The simultaneous tensioning protocol was used for graft fixation, in the bicruciate reconstruction, maintaining simultaneous tension to both grafts. Two distinctive graft fixation orders were evaluated: PCL fixation first was compared to ACL fixation first. PCL graft fixation was always accomplished at 90° of flexion and ACL graft fixation at full extension. Applying the simultaneous tensioning protocol, the results were different from the study of Moatshe et al., 2018. The study favored ACL fixation prior to PCL fixation using a simultaneous tensioning protocol (47). Tensioning the ACL first on Moatshe et al., 2018 study increased the risk of tibial posterior subluxation in extension (48). However, this might be avoided if both grafts were tensioned simultaneously due to the checkrein effect of the simultaneously tensioned PCL. The study indicates that graft fixation sequence in a bicruciate lesion, using a simultaneous tensioning protocol, should start with the ACL, in extension, to take advantage of the inherent stability of this position and the checkrein effect of the simultaneously tensioned PCL graft. The tibiofemoral articulation is close to the intact knee tibiofemoral orientation while in extension. Using the simultaneous tensioned PCL graft to avoid posterior subluxation of the tibia will lock the articulation into place by the ACL graft fixation. After that, PCL graft fixation will take place at 90° of knee flexion. The ACL fixed graft will act as a checkrein to avoid overcorrection of the tibial step-off caused by the manually applied anterior drawer, in accordance to the study of Kim et al., 2015 (47,49). This finding is supported by another study showing that full-extension is the most stable position after a complete bicruciate injury (47,50). In the setting of a simultaneous tensioning protocol involving a multiple ligament knee lesion, if the one intends to apply the simultaneous tensioning protocol for PLC multiple ligament lesions, the ACL should be fixed first, followed by the PCL and finally the PLC while maintaining simultaneous tension to all non-fixed grafts.
The best graft tensioning and fixation sequence comparing manual step-off reduction to simultaneous tensioning has yet to be determined.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Camilo Partezani Helito and Jorge Chahla) for the series “The Multiligament Injured Knee” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.11.04). The series “The Multiligament Injured Knee” was commissioned by the editorial office without any funding or sponsorship. CEF reports personal fees from Smith & Nephew, outside the submitted work. MSK reports personal fees from Smith & Nephew, personal fees from DePuy, outside the submitted work. RJA reports other from Smith & Nephew, outside the submitted work. MC reports grants, personal fees and other from Arthrex, outside the submitted work. MVML reports personal fees from DePuy, outside the submitted work. RFL reports personal fees and other from Arthrex, grants, personal fees and other from Ossur, grants, personal fees and other from Smith & Nephew, personal fees from Linvatec, outside the submitted work. RFL is on the editorial boards of AJSM, JEO and KSSTA, also serving on committees for AOSSM, ISAKOS and AANA. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Blackman AJ, Engasser WM, Krych AJ, et al. Fibular head and tibial-based (2-Tailed) posterolateral corner reconstruction. Sports Med Arthrosc 2015;23:44-50. [Crossref] [PubMed]
- LaPrade RF, Johansen S, Wentorf FA, et al. An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med 2004;32:1405-14. [Crossref] [PubMed]
- Miyatake S, Kondo E, Tsai TY, et al. Biomechanical comparisons between 4-strand and modified Larson 2-strand procedures for reconstruction of the posterolateral corner of the knee. Am J Sports Med 2011;39:1462-9. [Crossref] [PubMed]
- Moulton SG, Geeslin AG, LaPrade RF. A Systematic Review of the Outcomes of Posterolateral Corner Knee Injuries, Part 2: Surgical Treatment of Chronic Injuries. Am J Sports Med 2016;44:1616-23. [Crossref] [PubMed]
- Yoon KH, Bae DK, Ha JH, et al. Anatomic reconstructive surgery for posterolateral instability of the knee. Arthroscopy 2006;22:159-65. [Crossref] [PubMed]
- Franciozi CE, Albertoni LJB, Gracitelli GC, et al. Anatomic Posterolateral Corner Reconstruction With Autografts. Arthrosc Tech 2018;7:e89-95. [Crossref] [PubMed]
- Noyes FR, Barber-Westin SD, Albright JC. An analysis of the causes of failure in 57 consecutive posterolateral operative procedures. Am J Sports Med 2006;34:1419-30. [Crossref] [PubMed]
- Dhillon M, Akkina N, Prabhakar S, et al. Evaluation of outcomes in conservatively managed concomitant Type A and B posterolateral corner injuries in ACL deficient patients undergoing ACL reconstruction. Knee 2012;19:769-72. [Crossref] [PubMed]
- Kim SJ, Choi DH, Hwang BY. The influence of posterolateral rotatory instability on ACL reconstruction: comparison between isolated ACL reconstruction and ACL reconstruction combined with posterolateral corner reconstruction. J Bone Joint Surg Am 2012;94:253-9. [Crossref] [PubMed]
- Rochecongar G, Plaweski S, Azar M, et al. Management of combined anterior or posterior cruciate ligament and posterolateral corner injuries: a systematic review. Orthop Traumatol Surg Res 2014;100:S371-8. [Crossref] [PubMed]
- Camarda L, D'Arienzo M, Patera GP, et al. Avoiding tunnel collisions between fibular collateral ligament and ACL posterolateral bundle reconstruction. Knee Surg Sports Traumatol Arthrosc 2011;19:598-603. [Crossref] [PubMed]
- Gali JC, Bernardes Ade P, dos Santos LC, et al. Tunnel collision during simultaneous anterior cruciate ligament and posterolateral corner reconstruction. Knee Surg Sports Traumatol Arthrosc 2016;24:195-200. [Crossref] [PubMed]
- Geeslin AG, Moulton SG, LaPrade RF. A Systematic Review of the Outcomes of Posterolateral Corner Knee Injuries, Part 1: Surgical Treatment of Acute Injuries. Am J Sports Med 2016;44:1336-42. [Crossref] [PubMed]
- Chahla J, Moatshe G, Dean CS, et al. Posterolateral Corner of the Knee: Current Concepts. Arch Bone Jt Surg 2016;4:97-103. [PubMed]
- Shon OJ, Park JW, Kim BJ. Current Concepts of Posterolateral Corner Injuries of the Knee. Knee Surg Relat Res 2017;29:256-68. [Crossref] [PubMed]
- Levy BA, Dajani KA, Morgan JA, et al. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med 2010;38:804-9. [Crossref] [PubMed]
- Stannard JP, Brown SL, Farris RC, et al. The posterolateral corner of the knee: repair versus reconstruction. Am J Sports Med 2005;33:881-8. [Crossref] [PubMed]
- Geeslin AG, LaPrade RF. Outcomes of treatment of acute grade-III isolated and combined posterolateral knee injuries: a prospective case series and surgical technique. J Bone Joint Surg Am 2011;93:1672-83. [Crossref] [PubMed]
- Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 2000;28:282-96. [Crossref] [PubMed]
- Arthur A, LaPrade RF, Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med 2007;35:1844-50. [Crossref] [PubMed]
- LaPrade RF, Johansen S, Agel J, et al. Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am 2010;92:16-22. [Crossref] [PubMed]
- Laprade RF, Griffith CJ, Coobs BR, et al. Improving outcomes for posterolateral knee injuries. J Orthop Res 2014;32:485-91. [Crossref] [PubMed]
- Fanelli GC, Larson RV. Practical management of posterolateral instability of the knee. Arthroscopy 2002;18:1-8. [Crossref] [PubMed]
- Bicos J, Arciero RA. Novel approach for reconstruction of the posterolateral corner using a free tendon graft technique. Sports Med Arthrosc 2006;14:28-36. [Crossref] [PubMed]
- Feeley BT, Muller MS, Sherman S, et al. Comparison of posterolateral corner reconstructions using computer-assisted navigation. Arthroscopy 2010;26:1088-95. [Crossref] [PubMed]
- Ho EP, Lam MH, Chung MM, et al. Comparison of 2 surgical techniques for reconstructing posterolateral corner of the knee: a cadaveric study evaluated by navigation system. Arthroscopy 2011;27:89-96. [Crossref] [PubMed]
- Angelini FJ, Helito CP, Tozi MR, et al. Combined reconstruction of the anterior cruciate ligament and posterolateral corner with a single femoral tunnel. Arthrosc Tech 2013;2:e285-8. [Crossref] [PubMed]
- Helito CP, Bonadio MB, Demange MK, et al. Functional assessment of combined reconstruction of the anterior cruciate ligament and posterolateral corner with a single femoral tunnel: a two-year minimum follow-up. Int Orthop 2015;39:543-8. [Crossref] [PubMed]
- Stannard JP, Stannard JT, Cook JL. Repair or Reconstruction in Acute Posterolateral Instability of the Knee: Decision Making and Surgical Technique Introduction. J Knee Surg 2015;28:450-4. [Crossref] [PubMed]
- McCarthy M, Camarda L, Wijdicks CA, et al. Anatomic posterolateral knee reconstructions require a popliteofibular ligament reconstruction through a tibial tunnel. Am J Sports Med 2010;38:1674-81. [Crossref] [PubMed]
- Kim SJ, Kim TW, Kim SG, et al. Clinical comparisons of the anatomical reconstruction and modified biceps rerouting technique for chronic posterolateral instability combined with posterior cruciate ligament reconstruction. J Bone Joint Surg Am 2011;93:809-18. [Crossref] [PubMed]
- Sanders TL, Johnson NR, Pareek A, et al. Satisfactory knee function after single-stage posterolateral corner reconstruction in the multi-ligament injured/dislocated knee using the anatomic single-graft technique. Knee Surg Sports Traumatol Arthrosc 2018;26:1258-65. [PubMed]
- Stannard JP, Brown SL, Robinson JT, et al. Reconstruction of the posterolateral corner of the knee. Arthroscopy 2005;21:1051-9. [Crossref] [PubMed]
- Niki Y, Matsumoto H, Otani T, et al. A modified Larson's method of posterolateral corner reconstruction of the knee reproducing the physiological tensioning pattern of the lateral collateral and popliteofibular ligaments. Sports Med Arthrosc Rehabil Ther Technol 2012;4:21. [Crossref] [PubMed]
- Kim SJ, Park IS, Cheon YM, et al. New technique for chronic posterolateral instability of the knee: posterolateral reconstruction using the tibialis posterior tendon allograft. Arthroscopy 2004;20:195-200. [Crossref] [PubMed]
- Kang KT, Koh YG, Son J, et al. Finite Element Analysis of the Biomechanical Effects of 3 Posterolateral Corner Reconstruction Techniques for the Knee Joint. Arthroscopy 2017;33:1537-50. [Crossref] [PubMed]
- Suda Y, Seedhom BB, Matsumoto H, et al. Reconstructive treatment of posterolateral rotatory instability of the knee: a biomechanical study. Am J Knee Surg 2000;13:110-6. [PubMed]
- Yoon KH, Lee SH, Park SY, et al. Comparison of Anatomic Posterolateral Knee Reconstruction Using 2 Different Popliteofibular Ligament Techniques. Am J Sports Med 2016;44:916-21. [Crossref] [PubMed]
- Gelber PE, Erquicia JI, Sosa G, et al. Femoral tunnel drilling angles for the posterolateral corner in multiligamentary knee reconstructions: computed tomography evaluation in a cadaveric model. Arthroscopy 2013;29:257-65. [Crossref] [PubMed]
- Kim SJ, Chang CB, Choi CH, et al. Intertunnel relationships in combined anterior cruciate ligament and posterolateral corner reconstruction: an in vivo 3-dimensional anatomic study. Am J Sports Med 2013;41:849-57. [Crossref] [PubMed]
- Moatshe G, Brady AW, Slette EL, et al. Multiple Ligament Reconstruction Femoral Tunnels: Intertunnel Relationships and Guidelines to Avoid Convergence. Am J Sports Med 2017;45:563-9. [Crossref] [PubMed]
- LaPrade RF, Heikes C, Bakker AJ, et al. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am 2008;90:2069-76. [Crossref] [PubMed]
- Jackman T, LaPrade RF, Pontinen T, et al. Intraobserver and interobserver reliability of the kneeling technique of stress radiography for the evaluation of posterior knee laxity. Am J Sports Med 2008;36:1571-6. [Crossref] [PubMed]
- Wijdicks CA, Kennedy NI, Goldsmith MT, et al. Kinematic analysis of the posterior cruciate ligament, part 2: a comparison of anatomic single- versus double-bundle reconstruction. Am J Sports Med 2013;41:2839-48. [Crossref] [PubMed]
- Franciozi CE, Albertoni LJ, Ribeiro FN, et al. A simple method to minimize vascular lesion of the popliteal artery by guidewire during transtibial posterior cruciate ligament reconstruction: a cadaveric study. Arthroscopy 2014;30:1124-30. [Crossref] [PubMed]
- Kim SJ, Chang JH, Kang YH, et al. Clinical comparison of anteromedial versus anterolateral tibial tunnel direction for transtibial posterior cruciate ligament reconstruction: 2 to 8 years' follow-up. Am J Sports Med 2009;37:693-8. [Crossref] [PubMed]
- Franciozi CE, de Carvalho RT, Itami Y, et al. Bicruciate lesion biomechanics, Part 2-treatment using a simultaneous tensioning protocol: ACL fixation first is better than PCL fixation first to restore tibiofemoral orientation. Knee Surg Sports Traumatol Arthrosc 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Moatshe G, Chahla J, Brady AW, et al. The Influence of Graft Tensioning Sequence on Tibiofemoral Orientation During Bicruciate and Posterolateral Corner Knee Ligament Reconstruction: A Biomechanical Study. Am J Sports Med 2018;46:1863-9. [Crossref] [PubMed]
- Kim SJ, Kim SH, Jung M, et al. Does sequence of graft tensioning affect outcomes in combined anterior and posterior cruciate ligament reconstructions? Clin Orthop Relat Res 2015;473:235-43. [Crossref] [PubMed]
- de Carvalho RT, Franciozi CE, Itami Y, et al. Bicruciate lesion biomechanics, Part 1-Diagnosis: translations over 15 mm at 90 degrees of knee flexion are indicative of a complete tear. Knee Surg Sports Traumatol Arthrosc 2018; [Epub ahead of print]. [Crossref] [PubMed]
Cite this article as: Franciozi CE, Kubota MS, Abdalla RJ, Cohen M, Luzo MVM, LaPrade RF. Posterolateral corner repair and reconstruction: overview of current techniques. Ann Joint 2018;3:89.


