
How to avoid tunnel convergence in a multiligament injured knee
Introduction
A multi-ligament knee injury is defined as a tear of at least two of the four major knee ligament structure complexes: the posterior cruciate ligament (PCL), the anterior cruciate ligament (ACL), the posterolateral corner (PLC) and the posteromedial corner (PMC) (Figure 1) (1,2). These injuries are less common than isolated knee ligament injuries; however, identifying and diagnosing these complex and challenging injuries is important. Knee dislocations result in multiligament knee injuries; however, multiligament knee injuries can occur in the absence of a knee dislocation. A high level of suspicion, and a thorough and systematic evaluation of the patient is mandatory to diagnose these injuries because a missed diagnosis can lead to persistent instability, pain and ligament reconstruction failure if all torn ligaments are not addressed concurrently.

Knee ligament injury patterns and epidemiology
Despite being less common than isolated knee ligament tears, multiligament knee injuries are not as rare as previously reported (3). Medial side structures are commonly injured in multiligament knee injuries occurring after knee dislocations (4). Grade III medial-sided injuries have a concomitant cruciate ligament injury in 78% of the cases (5). In a setting of bicruciate knee dislocations, medial sided injuries have been reported to occur in 17–52% of the cases (4,6). Injuries to the PLC and fibular collateral ligament (FCL) are typically associated with concomitant knee ligament injuries such as ACL and PCL tears (5-7). In a series of 102 patients with acute PLC injuries, isolated PLC injuries were found in only 28 patients. Thus, patients with high grade (grade III) medial or lateral collateral ligament tears should be evaluated for combined injuries.
Moatshe et al. evaluated 303 patients with bicruciate knee dislocations, and reported that 52% had medial-sided injuries (KD IIIM), 28% had lateral sided injuries (KD IIIL) and 13% had injuries to all four major knee stabilizers (KD IV) (4). These findings demonstrate that up to 83% of patients with multiligament knee injuries after a knee dislocation will require reconstruction of three or more ligaments. In all knee injuries, especially high energy injuries, it is important to evaluate the integrity of all ligaments. A thorough and systematic evaluation of the knee is imperative to identify all the injured structures, develop a management plan and to optimize functional outcomes. Furthermore, the use of imaging, including magnetic resonance imaging (MRI), to diagnose concomitant injuries (Figure 1), and stress radiographs to evaluate the extent of ligament injury is recommended. This is particularly important in chronic cases where MRI has been demonstrated to have lower sensitivity for PCL and FCL tears compared to stress radiographs (7,8).
Treatment of multiligament knee injuries
Non-operative treatment
Grade I and II ligament injuries whether isolated, or in multiligament injured knees, are usually treated non-operatively. Non-operative treatment of knee ligament injuries usually involves bracing for 5–7 weeks and physical rehabilitation programs that focus on restoring knee range of motion, proprioception and patella mobility, enhancing quadriceps function, and controlling edema (9). However, the type of brace, duration of bracing and the rehabilitation protocol depends on the concomitant knee ligament injuries.
Operative treatment
Surgical treatment of grade III ligament injuries in the setting of multiligament knee injuries has been demonstrated to result in superior clinical outcomes compared to non-surgical treatment (1,10-14). Reconstruction of the cruciate ligaments is widely accepted, and is regarded as the standard of treatment despite recent increasing interest in surgical repair of the torn cruciate ligaments (15). Studies have reported higher failure and reoperation rates after repair of the collateral ligaments compared to reconstructions (16,17). Thus, it is usually recommended to reconstruct both the cruciate (18-21) and collateral ligaments (16,17) when torn. Anatomic knee ligament reconstruction has been demonstrated to restore the native anatomy and biomechanics. Furthermore, it is recommended that all injured structures be reconstructed concurrently in order to minimize the risk of reconstruction graft failure and to allow for early knee motion (22-25). Biomechanical studies have demonstrated that untreated grade III PLC injuries increase the forces on both the ACL and PCL, which can increase the risk of graft failure (23,24).
The qualitative and quantitative anatomy of the native knee ligaments, which is the basis for optimal tunnel placement for anatomic reconstruction of knee ligament structures have previously been defined (26-33). In the setting of multiligament reconstruction in the knee, several tunnels are needed for the reconstruction grafts in both the distal femur and proximal tibia and the risk of tunnel convergence is high. When reconstruction tunnels converge, the reconstruction graft can be damaged and increase the risk of reconstruction failure. Additionally, damage to fixation devices and poor graft fixation can occur, leading to reconstruction failure. Furthermore, creating several tunnels may lead to bone loss and there may not be sufficient bone stock for graft fixation, incorporation and healing.
Avoiding tunnel convergence
Femoral tunnels
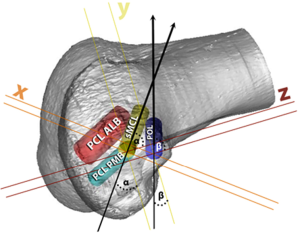
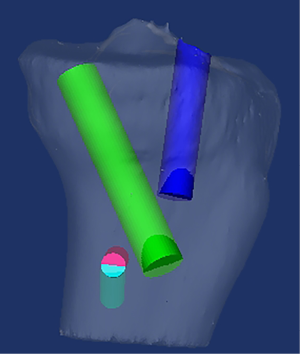
In the setting of global laxity where all four major knee ligament structures are torn, there will potentially be four tunnels or sockets [double bundle PCL, sMCL and posterior oblique ligament (POL)] in the medial femoral condyle and three on the lateral femoral condyle [ACL, FCL and popliteus tendon (PLT)]. Aiming the collateral ligament tunnels, POL and popliteus tunnel straight across the distal femur and parallel to the joint line increases the risk of convergence with cruciate ligament tunnels. On the medial femoral side, Moatshe et al. (34) reported that aiming the sMCL tunnel 40° in the axial and coronal planes and the POL tunnel 20° in the axial and coronal planes was safe to avoid convergence with the double bundle PCL tunnels (Figures 2,3). Gelber et al. evaluated tunnel convergence and optimal angulation of the tunnels on the medial femur condyle, and found that aiming the PMC tunnels (superficial MCL and POL) 30° in the axial plane and coronal plane reduced the risk of convergence with the PCL tunnels (35).
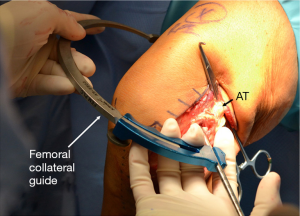
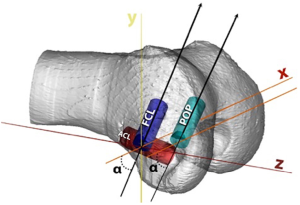
On the lateral femoral condyle, the FCL and popliteus tunnels should be parallel to each other. In a recent study evaluating the risk of tunnel convergence in the femur and the optimal angulation of the tunnels, Moatshe et al., found that aiming both the FCL (lateral collateral ligament) and the PLT tunnels 35–40° anteriorly reduced the risk of convergence with the ACL tunnel (Figure 4) (34). In addition, Shuler et al reported that angles over 40° should be avoided because they lead to elliptical tunnels (36), which can ultimately lead to poor fixation of the reconstruction grafts.
It is important to be aware of the risk of tunnel convergence when treating multiligament injuries and plan tunnel placement and orientation appropriately. Furthermore, the use of perioperative fluoroscopy may be beneficial.
Some authors argue that the MCL has a good intrinsic healing potential and hence can be treated non-operatively, even in multiligament injuries. With this approach, the knee is placed in a brace for 6–8 weeks until the MCL heals, and the other ligaments can be treated surgically at a later stage. This approach allows for early mobilization of the knee to reduce the risk of arthrofibrosis and reduce surgery time. Furthermore, if the MCL heals, the risk of tunnel convergence with the PCL is minimized (37). However, it is important to remember that a multiligament knee injury is more complex, with more soft tissue injury; therefore, the healing potential of the MCL may be compromised by both the large injury and the secondary instability of the knee. Thus, a medial side injury in a setting of a multiligament knee injury is different from an isolated MCL injury. High grade injuries (grade III) of the PMC, specifically tears with valgus gapping in extension and distal tears of the MCL, have a higher risk of not healing, with a resultant residual valgus and rotational instability (38,39). Persistent instability increases the forces acting on the ACL and PCL reconstruction grafts, increasing the risk of reconstruction graft failure. Therefore, in a setting of a multiligament knee injury involving the PMC, early concurrent reconstruction is recommended to facilitate early mobilization and rehabilitation (25).
Tibial tunnels
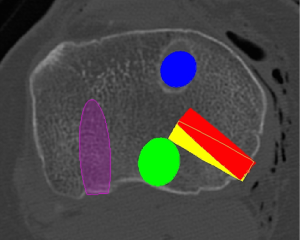
In a setting where all major knee ligaments are torn (KD IV), there will potentially be a total of 5 tunnels in the proximal tibia when using anatomic and biomechanically validated reconstruction techniques (29,30,40-42). The number of tunnels in the tibia can be increased in the setting of meniscal root repair with transtibial technique. Moatshe et al. (43). reported that the rate of tunnel convergence between the POL and the PCL tunnels in the tibia when the POL tunnel was aimed at Gerdy’s tubercle was 67%. This high convergence rate can lead to reconstruction graft failure. The risk of tunnel convergence between the POL and the PCL can be minimized by aiming the POL tunnel to a point 15 mm medial to Gerdy’s tubercle (Figure 5). There is an increased risk of tunnel convergence between the PCL tunnel and the superficial medial collateral ligament (sMCL) tunnel, both of which are created 6 cm from the joint line on the tibia. In a study using 3DCT and Mimics software to recreate anatomic reconstructions, Moatshe et al. recommended that the sMCL tunnel be aimed 30° distally to avoid convergence with the PCL (Figure 6) (43). In smaller knees, the PLC tunnel may be too close to the PCL tunnel posteriorly, it is imperative to use the anatomic landmarks to ensure correct placement of the tunnels to avoid convergence. Fluoroscopy can also be utilized preoperatively to verify pin placement prior to reaming.
Summary
Multiligament knee injuries are challenging to diagnose and treat. Surgical treatment of the torn ligaments has been demonstrated to be superior to non-operative management. Furthermore, reconstruction of the torn ligaments has been demonstrated to be superior to repair. In the setting of multiple knee ligament reconstructions, the risk of tunnel convergence is high because of the total number and size of the tunnels in a limited bone mass. It is recommended to perform anatomic ligament reconstructions to restore both the anatomy and the biomechanics of the knee. Thorough planning of tunnel placement and orientation is important.
On the medial femoral condyle, aiming the sMCL tunnel 40° proximally (towards the hip) and 20–40° anteriorly in the axial plane can reduce the risk of collision with the PCL tunnels. If there is a concurrent POL reconstruction, the sMCL tunnel should be aimed 40° proximally and 40° anteriorly, and the POL tunnel should be aimed 20° proximally and 20° anteriorly to minimize the risk of convergence with the PCL tunnels. On the lateral femoral condyle, it is recommended to aim both the FCL and the PLT tunnels 35–40° anteriorly to reduce the risk of convergence with the ACL tunnel.
On the proximal tibia, aiming the POL towards Gerdy’s tubercle increases the risk of convergence with the PCL tunnel; therefore, it is recommended to aim the POL tunnels to a point 15 mm medial to Gerdy’s tubercle to reduce risk of convergence with the PCL tunnel. If the sMCL is reconstructed concurrently with the PCL, convergence between the tunnels can be minimized by aiming the sMCL 30° distally. Good exposure to identify the anatomic landmarks and the use of intra-operative fluoroscopy can facilitate better tunnel placement and orientation.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Camilo Partezani Helito and Jorge Chahla) for the series “The Multiligament Injured Knee” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interests: The series “The Multiligament Injured Knee” was commissioned by the editorial office without any funding or sponsorship. RFL American Journal of Sports Medicine: Editorial or governing board; American Orthopaedic Society for Sports Medicine: Board or committee member; Arthrex, Inc: IP royalties; Paid consultant; Research support; International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine: Board or committee member; Journal of Experimental Orthopaedics: Editorial or governing board; Knee Surgery, Sports Traumatology, Arthroscopy: Editorial or governing board; Linvatec: Research support; Ossur: IP royalties; Paid consultant; Research support; Smith & Nephew: IP royalties; Paid consultant; Research support. Lars Engebretsen: Acta Orthopaedica: Editorial or governing board; American Orthopaedic Society for Sports Medicine: Board or committee member; Arthrex, Inc: IP royalties; Paid consultant; Research support; Biomet: Research support; BJSM: Publishing royalties, financial or material support; ESSKA: Board or committee member; iBalance: Stock or stock Options; International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine: Board or committee member. Journal of Bone and Joint Surgery - American: Editorial or governing board; Knee: Editorial or governing board; Knee Surgery, Sports Traumatology, Arthroscopy: Editorial or governing board; Smith & Nephew: Research support. Gilbert Moatshe: Research support from Arthrex Inc and South eastern Norway health Authorities; Journal of Arthroscopy: Editorial Board member. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Levy BA, Dajani KA, Whelan DB, et al. Decision Making in the Multiligament-Injured Knee: An Evidence-Based Systematic Review. Arthroscopy 2009;25:430-8. [Crossref] [PubMed]
- Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma 1997;11:525-9. [Crossref] [PubMed]
- Arom GA, Yeranosian MG, Petrigliano FA, et al. The changing demographics of knee dislocation: a retrospective database review. Clin Orthop Relat Res 2014;472:2609-14. [Crossref] [PubMed]
- Moatshe G, Dornan GJ, Loken S, et al. Demographics and Injuries Associated With Knee Dislocation: A Prospective Review of 303 Patients. Orthop J Sports Med 2017;5:2325967117706521 [Crossref] [PubMed]
- Halinen J, Lindahl J, Hirvensalo E, et al. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med 2006;34:1134-40. [Crossref] [PubMed]
- Becker EH, Watson JD, Dreese JC. Investigation of multiligamentous knee injury patterns with associated injuries presenting at a level I trauma center. J Orthop Trauma 2013;27:226-31. [Crossref] [PubMed]
- DePhillipo NN, Cinque ME, Godin JA, et al. Posterior Tibial Translation Measurements on Magnetic Resonance Imaging Improve Diagnostic Sensitivity for Chronic Posterior Cruciate Ligament Injuries and Graft Tears. Am J Sports Med 2018;46:341-7. [Crossref] [PubMed]
- Kane PW, DePhillipo NN, Cinque ME, et al. Increased Accuracy of Varus Stress Radiographs Versus Magnetic Resonance Imaging in Diagnosing Fibular Collateral Ligament Grade III Tears. Arthroscopy 2018;34:2230-5. [Crossref] [PubMed]
- Peterson L, Junge A, Chomiak J, et al. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med 2000;28:S51-7. [Crossref] [PubMed]
- Dwyer T, Marx RG, Whelan D. Outcomes of treatment of multiple ligament knee injuries. J Knee Surg 2012;25:317-26. [Crossref] [PubMed]
- Fanelli GC, Stannard JP, Stuart MJ, et al. Management of complex knee ligament injuries. J Bone Joint Surg Am 2010;92:2235-46. [PubMed]
- Peskun CJ, Whelan DB. Outcomes of operative and nonoperative treatment of multiligament knee injuries: an evidence-based review. Sports Med Arthrosc Rev 2011;19:167-73. [Crossref] [PubMed]
- Meyers MH, Moore TM, Harvey JP Jr. Traumatic dislocation of the knee joint. J Bone Joint Surg Am 1975;57:430-3. [Crossref] [PubMed]
- O'Donoghue DH. An analysis of end results of surgical treatment of major injuries to the ligaments of the knee. J Bone Joint Surg Am 1955;37-A:1-13. passim. [Crossref] [PubMed]
- Levy BA, Fanelli GC, Whelan DB, et al. Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg 2009;17:197-206. [Crossref] [PubMed]
- Stannard JP, Brown SL, Farris RC, et al. The posterolateral corner of the knee: repair versus reconstruction. Am J Sports Med 2005;33:881-8. [Crossref] [PubMed]
- Levy BA, Dajani KA, Morgan JA, et al. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med 2010;38:804-9. [Crossref] [PubMed]
- Feagin JA Jr, Curl WW. Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med 1976;4:95-100. [Crossref] [PubMed]
- Engebretsen L, Benum P, Sundalsvoll S. Primary suture of the anterior cruciate ligament. A 6-year follow-up of 74 cases. Acta Orthop Scand 1989;60:561-4. [Crossref] [PubMed]
- Grøntvedt T, Engebretsen L, Benum P, et al. A prospective, randomized study of three operations for acute rupture of the anterior cruciate ligament. Five-year follow-up of one hundred and thirty-one patients. J Bone Joint Surg Am 1996;78:159-68. [Crossref] [PubMed]
- Fu FH, Bennett CH, Ma CB, et al. Current trends in anterior cruciate ligament reconstruction. Part II. Operative procedures and clinical correlations. Am J Sports Med 2000;28:124-30. [Crossref] [PubMed]
- Harner CD, Vogrin TM, Hoher J, et al. Biomechanical analysis of a posterior cruciate ligament reconstruction. Deficiency of the posterolateral structures as a cause of graft failure. Am J Sports Med 2000;28:32-9. [Crossref] [PubMed]
- LaPrade RF, Resig S, Wentorf F, et al. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med 1999;27:469-75. [Crossref] [PubMed]
- LaPrade RF, Muench C, Wentorf F, et al. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: a biomechanical study. Am J Sports Med 2002;30:233-8. [Crossref] [PubMed]
- Geeslin AG, LaPrade RF. Outcomes of treatment of acute grade-III isolated and combined posterolateral knee injuries: a prospective case series and surgical technique. J Bone Joint Surg Am 2011;93:1672-83. [Crossref] [PubMed]
- LaPrade RF, Johansen S, Wentorf FA, et al. An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med 2004;32:1405-14. [Crossref] [PubMed]
- Lind M, Jakobsen BW, Lund B, et al. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med 2009;37:1116-22. [Crossref] [PubMed]
- Coobs BR, Wijdicks CA, Armitage BM, et al. An in vitro analysis of an anatomical medial knee reconstruction. Am J Sports Med 2010;38:339-47. [Crossref] [PubMed]
- Laprade RF, Wijdicks CA. Surgical technique: development of an anatomic medial knee reconstruction. Clin Orthop Relat Res 2012;470:806-14. [Crossref] [PubMed]
- Spiridonov SI, Slinkard NJ, LaPrade RF. Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Joint Surg Am 2011;93:1773-80. [Crossref] [PubMed]
- Ziegler CG, Pietrini SD, Westerhaus BD, et al. Arthroscopically pertinent landmarks for tunnel positioning in single-bundle and double-bundle anterior cruciate ligament reconstructions. Am J Sports Med 2011;39:743-52. [Crossref] [PubMed]
- Anderson CJ, Ziegler CG, Wijdicks CA, et al. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am 2012;94:1936-45. [Crossref] [PubMed]
- Johannsen AM, Anderson CJ, Wijdicks CA, et al. Radiographic landmarks for tunnel positioning in posterior cruciate ligament reconstructions. Am J Sports Med 2013;41:35-42. [Crossref] [PubMed]
- Moatshe G, Brady AW, Slette EL, et al. Multiple Ligament Reconstruction Femoral Tunnels: Intertunnel Relationships and Guidelines to Avoid Convergence. Am J Sports Med 2017;45:563-9. [Crossref] [PubMed]
- Gelber PE, Masferrer-Pino A, Erquicia JI, et al. Femoral Tunnel Drilling Angles for Posteromedial Corner Reconstructions of the Knee. Arthroscopy 2015;31:1764-71. [Crossref] [PubMed]
- Shuler MS, Jasper LE, Rauh PB, et al. Tunnel convergence in combined anterior cruciate ligament and posterolateral corner reconstruction. Arthroscopy 2006;22:193-8. [Crossref] [PubMed]
- Tibor LM, Marchant MH Jr, Taylor DC, et al. Management of medial-sided knee injuries, part 2: posteromedial corner. Am J Sports Med 2011;39:1332-40. [Crossref] [PubMed]
- Wijdicks CA, Griffith CJ, Johansen S, et al. Injuries to the Medial Collateral Ligament and Associated Medial Structures of the Knee. J Bone Joint Surg Am 2010;92:1266-80. [Crossref] [PubMed]
- Chahla J, Nitri M, Civitarese D, et al. Anatomic Double-Bundle Posterior Cruciate Ligament Reconstruction. Arthrosc Tech 2016;5:e149-56. [Crossref] [PubMed]
- Goldsmith MT, Jansson KS, Smith SD, et al. Biomechanical comparison of anatomic single- and double-bundle anterior cruciate ligament reconstructions: an in vitro study. Am J Sports Med 2013;41:1595-604. [Crossref] [PubMed]
- Serra Cruz R, Mitchell JJ, Dean CS, et al. Anatomic Posterolateral Corner Reconstruction. Arthrosc Tech 2016;5:e563-72. [Crossref] [PubMed]
- Wijdicks CA, Kennedy NI, Goldsmith MT, et al. Kinematic analysis of the posterior cruciate ligament, part 2: a comparison of anatomic single- versus double-bundle reconstruction. Am J Sports Med 2013;41:2839-48. [Crossref] [PubMed]
- Moatshe G, Slette EL, Engebretsen L, et al. Intertunnel Relationships in the Tibia During Reconstruction of Multiple Knee Ligaments: How to Avoid Tunnel Convergence. Am J Sports Med 2016;44:2864-9. [Crossref] [PubMed]
Cite this article as: Moatshe G, LaPrade RF, Engebretsen L. How to avoid tunnel convergence in a multiligament injured knee. Ann Joint 2018;3:93.


