
Combined anterior cruciate ligament and posterolateral corner injuries: diagnosis and treatment
Introduction
The treatment of isolated anterior cruciate ligament (ACL) injury has been well described in the literature, yet there still remain challenges to successful outcomes when injuries involve concomitant ligamentous injury. Historically, combined posterolateral corner (PLC) injuries have often gone undiagnosed and have been identified as a significant risk factor for ACL reconstruction (ACLR) graft failure (1). With further advancements in the objective diagnosis of multiligament knee injuries (2,3), recent studies have now reported that these injuries occur more often than once believed, as up to 11% of ACL-deficient knees present with combined PLC injury (1,4).
Biomechanical studies evaluating ACLRs in the setting of a deficient PLC has emphasized the need for an anatomic PLC reconstruction (PLCR) to restore native knee kinematics and protect the integrity of the ACLR graft (5-7). This is because untreated PLC deficiency has been reported to increase the loads experienced by the ACL graft due to rotary and varus instability (8). Clinically, PLC deficiency has further been reported to influence postoperative graft laxity, have poorer outcomes, and increased ACLR graft failure.
Proper recognition, diagnosis, and treatment of associated PLC injuries is essential to restore the native function of the knee joint and reduce the risk of ACLR failure. Improved knee stability and surgical outcomes can be achieved when all concurrent pathology is addressed, specifically when treated with combined anatomic ACL and PLC reconstructions. Therefore, the purpose of this article was to review the relevant literature on the diagnosis and treatment of concomitant ACL and posterolateral corner injuries.
History
Previous studies have reported high rates of undiagnosed concomitant PLC injury, highlighting a major underlying cause of failed ACLRs due to graft overload and emphasizing the need for a thorough patient assessment at the time of initial presentation (9-11). The bony anatomy of the lateral knee is inherently unstable and PLC injury can often be recognized in patients who report with feelings of varus instability in full knee extension (12). There should also be a high suspicion of combined ACL-PLC injury when the mechanism of injury occurs from either high-velocity motor vehicle accidents or low-velocity sports-related activities, most notably those involving falls onto a hyperextended and varus knee (1,13,14). A significant risk of concomitant neurovascular injury has further been reported with PLC tears (12,15,16). Therefore, initial clinical exams should include a thorough neurovascular evaluation to rule out potential injury to the popliteal artery in acute cases and possible damage to the common peroneal nerve (which sustain a traction injury in up to 15% of PLC-injured patients) (13). A comprehensive patient history is essential especially in chronic cases, because chronic PLC tears are often difficult to diagnose with magnetic resonance imaging alone (1,17).
Physical exam
Physical examination can be extremely useful in diagnosing ACL injuries. Patients who have a significant increase in anterior translation on the Lachman or anterolateral rotation of the pivot-shift examinations should be carefully assessed for any concurrent lack of secondary restraints such the posterior horn of the medial meniscus (18), root tear of the posterior horn of the medial meniscus and most importantly, the static structures of the PLC. If the patient has significant anterior tibial translation on the Lachman exam or an “explosive” pivot shift, the examiner should be suspicious for a possible combined PLC injury.
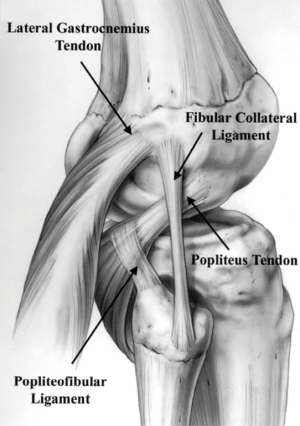
The PLC is responsible for providing stability in multiple planes of knee motion. The PLC acts as a restraint to varus translation, external rotation and posterolateral rotation. Furthermore, the PLC structures act as secondary stabilizers to anterior and posterior tibial translation (Figure 1). The role of the PLC as a secondary restraint to anterior and posterior translation is of particular importance when considering the increased force across an ACLR graft in the setting of an untreated PLC injury.
To determine the degree of varus laxity of the injured knee, the patient’s knee is flexed into 20 to 30 degrees of flexion with the patient’s thigh flat against the exam table. Correct position of the patient’s injured extremity cannot be understated, because it will allow for greater patient relaxation and in turn, a more reliable physical exam. Once the patient’s affected knee is properly positioned, a varus force is applied across the knee. This force should be applied to the knee through the foot and ankle to permit rotatory motion to occur through the knee, and not the distal leg. Examining the uninjured knee prior to the injured knee can allow the examiner to gain an understanding of the patient’s native ligamentous laxity and allow for better assessment of the degree of varus gapping on the injured side.
A second crucial physical examination maneuver is the dial test (also known as the external rotation test). This test assesses for the amount of increased external rotation of the knee at both 30 and 90 degrees of knee flexion and is compared with the contralateral side. The dial test is performed with the patient either prone or supine. The examining surgeon rotates both feet and ankles simultaneously and evaluates the degree of increased external rotation on the injured leg. If there is an increase of at least 15 degrees of external rotation between the injured and uninjured sides, a posterolateral injury should be suspected. When the dial test is positive at 30 degrees but negative at 90 degrees an isolated PLC injury is likely. However, when the dial test is positive at both 30 and 90 degrees a combined PLC and posterior cruciate ligament (PCL) injury merits further clinical and radiographic evaluation (19). It is also important to assess for a medial collateral ligament (MCL) tear with an increased dial test.
A third valuable physical exam maneuver to evaluate for lateral knee injuries is the heel height test. This test is performed with the examiner grasping the patient’s great toe on the injured extremity and lifting the foot vertically, while stabilizing the distal thigh to avoid knee elevation and rotation. The same maneuver is then performed on the uninjured side and a side-to-side difference (SSD) is calculated. An SSD of 3 cm has demonstrated greater than 80% sensitivity and specificity for the detection of combined ACL and fibular collateral ligament (FCL) injuries (3). With the leg in this position the examiner can also examine the degree of recurvatum and assess for peroneal nerve deficits. It is important to perform a well-developed set of physical exam maneuvers to detect these combined injuries because they occur together in approximately 11 of ACL tears (9).
Radiographic evaluation
In the setting of positive physical exam findings, radiographic evaluation of ligamentous and other soft tissue pathology is paramount. Varus stress radiographs are an essential tool to diagnose PLC injuries. Isolated FCL injuries have been demonstrated to produce 2.7 mm of increased lateral compartment gapping compared to the contralateral limb on varus stress radiographs, while complete PLC injuries have been shown to produce ≥4 mm when compared to the contralateral side (2,4,20). However, these SSD values are not absolute cut-offs because patient specific factors such as acute injuries and patient guarding can skew the degree of lateral compartment gapping seen on radiographs. However, varus stress radiographs are valuable in determining if a patient has increased lateral compartment gapping, medial compartment pseudolaxity, or if a medial compartment injury occurred concurrently with a PLC injury (12,21-23).
Effect of PLC injuries on ACLR
The PLC functions in resisting varus and external rotational movements of the knee. Untreated or unrecognized grade III PLC injuries may place a significant amount of force on an ACLR graft due to varus laxity created by the FCL tear, thus potentially increasing the risk of ACLR graft failure if the PLC is not reconstructed simultaneously (9). When performing concomitant anatomic PLC and ACLRs, the PLC structures should be reconstructed and fixed before ACL graft fixation to prevent a fixed external rotation deformity (24). Additionally, genu varus malalignment can cause significant unwanted varus stress on the ACLR graft. Therefore, in the chronic and revision settings, longstanding alignment radiographs should be obtained to rule out varus malalignment (25). This diagnostic approach is even more important to consider if there is a combined ACL and PLC injury—thus, a first-stage medial opening wedge proximal tibial osteotomy may be indicated for these patients to decrease the risk of ACL and PLC graft failure (26).
Anatomic PLCR
The corresponding author’s preferred anatomic reconstruction technique has been previously described (5). A two-graft technique is utilized to restore the FCL, PLT, and PFL. Following an open lateral hockey stick incision and subsequent dissection to locate the common peroneal nerve, the tibial and fibular attachment sites are identified. Through the FCL-biceps bursa, the fibular attachment of the FCL is found on the lateral aspect of the fibular head. The fibular tunnel is first drilled from the lateral aspect of the fibular head to the PFL attachment site on the posteromedial aspect of the fibular styloid. The fibular attachment of the PFL is located on the posteromedial aspect of the fibular styloid, and the musculotendinous junction attachment of the PFL and PLT is identified on the posterolateral aspect of the tibia, near the posterior tibial popliteal sulcus (5,27). Next, the tibial tunnel is drilled anterior-to-posterior from a point medial and distal to Gerdy’s tubercle, to the popliteus musculotendinous junction on the posterior aspect of the tibial sulcus.
A horizontal incision is then made through the iliotibial band, and the femoral attachment sites of the PLT and FCL are identified on the proximal fifth of the popliteal sulcus and proximal and posterior to the lateral epicondyle, respectively (12,28). The subsequent femoral tunnels for both the FCL and PLT are then reamed in the anteromedial direction from the attachment sites identified. When a complete PLCR is performed concurrently with ACLRs (Figures 2,3), the FCL and PLT femoral tunnels should be aimed approximately 35° anteriorly, as opposed to 0° in isolated PLCRs, to eliminate the potential for tunnel convergence with the femoral ACLR tunnel and ultimately graft failure (29).
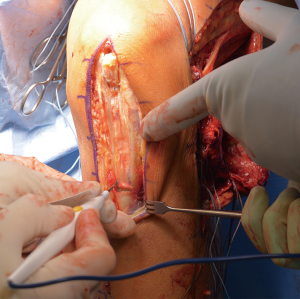
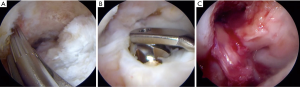
In order to prevent external rotation deformity, PLC structures should first be secured prior to the ACL (24). The first graft is used to restore the PLT, and is first fixed at its femoral attachment, followed by graft passage through the popliteal hiatus to the musculotendinous junction of the popliteus, and pulled through the tibial tunnel posterior to anterior. The second graft is utilized for restoration of both the FCL and PFL. The graft is initially fixed at the femoral attachment of the FCL, and is passed beneath the superficial layer of the iliotibial band and long head of the biceps femoris along its anatomic trajectory, and is passed through the fibular tunnel from lateral to posteromedial and fixed in the fibular head tunnel at 20 degrees of knee flexion, followed by the ensuing passage from posterior to anterior through the tibial tunnel (neighboring the PLT graft). Both grafts (PLT and PFL/FCL) are then tensioned and fixated on the anterior tibia (Figure 4).

Outcomes following anatomic PLCRs that include concurrent ACLRs have been shown to significantly improve in regards to varus stability through varus stress radiographs, external rotation stability on examination, and single leg hop scores postoperatively (30). Furthermore, patients report improved subjective outcome scores with significant increases from preoperative to postoperative. In addition, acutely injured patients (<3 weeks) report better improvements postoperatively than chronic patients (>3 weeks) which highlights the urgency for prompt diagnosis and proper surgical management.
Conclusions and future directions
Proper diagnosis and treatment of combined ACL and PLC injuries is essential to maximize patient outcome. Objective diagnosis of isolated FCL or complete PLC tears with varus stress radiographs is strongly recommended. Further investigation into eh safety of early weight bearing with anatomic-based FCL and PLCRs is ongoing.
Take home points
- Understanding the high prevalence of associated PLC injuries with ACL injuries is crucial for diagnosis, especially in the setting of knee hyperextension and varus force mechanisms of injury.
- Physical examination is key to properly diagnose and treat PLC injuries. Moreover, the use of varus stress radiographs provide an objective diagnosis for guiding treatment options.
- PLC injuries should raise concern for potential neurovascular injuries and a thorough neurovascular exam should be conducted. Additionally, the common peroneal nerve should be carefully monitored both preoperatively and postoperatively to ensure the patient does not develop a foot drop due to either the injury itself or post-surgical swelling/compression.
- Anatomic reconstruction of the ACL and PLC structures have demonstrated significant objective and subjective improvements in patient outcomes.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “The Multiligament Injured Knee”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.11.08). The series “The Multiligament Injured Knee” was commissioned by the editorial office without any funding or sponsorship. JC served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bonanzinga T, Zaffagnini S, Grassi A, et al. Management of Combined Anterior Cruciate Ligament–Posterolateral Corner Tears: A Systematic Review. Am J Sports Med 2014;42:1496-503. [Crossref] [PubMed]
- Jackman T, LaPrade RF, Pontinen T, et al. Intraobserver and interobserver reliability of the kneeling technique of stress radiography for the evaluation of posterior knee laxity. Am J Sports Med 2008;36:1571-6. [Crossref] [PubMed]
- Cinque ME, Geeslin AG, Chahla J, et al. The Heel Height Test: A Novel Tool for the Detection of Combined Anterior Cruciate Ligament and Fibular Collateral Ligament Tears. Arthroscopy 2017;33:2177-81. [Crossref] [PubMed]
- LaPrade RF, Wentorf FA, Fritts H, et al. A prospective magnetic resonance imaging study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthroscopy 2007;23:1341-7. [Crossref] [PubMed]
- LaPrade RF, Johansen S, Wentorf FA, et al. An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med 2004;32:1405-14. [Crossref] [PubMed]
- LaPrade RF, Tso A, Wentorf FA. Force measurements on the fibular collateral ligament, popliteofibular ligament, and popliteus tendon to applied loads. Am J Sports Med 2004;32:1695-701. [Crossref] [PubMed]
- LaPrade RF, Wentorf FA, Crum JA. Assessment of healing of grade III posterolateral corner injuries: an in vivo model. J Orthop Res 2004;22:970-5. [Crossref] [PubMed]
- Geeslin AG, Moulton SG, LaPrade RF. A Systematic Review of the Outcomes of Posterolateral Corner Knee Injuries, Part 1: Surgical Treatment of Acute Injuries. Am J Sports Med 2016;44:1336-42. [Crossref] [PubMed]
- LaPrade RF, Resig S, Wentorf F, et al. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med 1999;27:469-75. [Crossref] [PubMed]
- Pacheco RJ, Ayre CA, Bollen SR. Posterolateral corner injuries of the knee: a serious injury commonly missed. J Bone Joint Surg Br 2011;93:194-7. [Crossref] [PubMed]
- O'Brien SJ, Warren RF, Pavlov H, et al. Reconstruction of the chronically insufficient anterior cruciate ligament with the central third of the patellar ligament. J Bone Joint Surg Am 1991;73:278-86. [Crossref] [PubMed]
- LaPrade RF, Terry GC. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med 1997;25:433-8. [Crossref] [PubMed]
- Mitchell JJ, Cinque ME, Dornan GJ, et al. Primary Versus Revision Anterior Cruciate Ligament Reconstruction: Patient Demographics, Radiographic Findings, and Associated Lesions. Arthroscopy 2018;34:695-703. [Crossref] [PubMed]
- Moatshe G, Chahla J, LaPrade RF, et al. Diagnosis and treatment of multiligament knee injury: State of the art. J ISAKOS Jt Disord Orthop Sport Med 2017;2:152-61. [Crossref]
- Moatshe G, Dornan GJ, Løken S, et al. Demographics and injuries associated with knee dislocation: A prospective review of 303 patients. Orthop J Sports Med 2017;5:2325967117706521 [Crossref] [PubMed]
- Ridley TJ, McCarthy MA, Bollier MJ, et al. The incidence and clinical outcomes of peroneal nerve injuries associated with posterolateral corner injuries of the knee. Knee Surg Sports Traumatol Arthrosc 2018;26:806-11. [Crossref] [PubMed]
- Devitt BM, Whelan DB. Physical examination and imaging of the lateral collateral ligament and posterolateral corner of the knee. Sports Med Arthrosc Rev 2015;23:10-6. [Crossref] [PubMed]
- DePhillipo NN, Moatshe G, Brady A, et al. Effect of Meniscocapsular and Meniscotibial Lesions in ACL-Deficient and ACL-Reconstructed Knees: A Biomechanical Study. Am J Sports Med 2018;46:2422-31. [Crossref] [PubMed]
- LaPrade RF, Ly TV, Griffith C. The external rotation recurvatum test revisited: reevaluation of the sagittal plane tibiofemoral relationship. Am J Sports Med 2008;36:709-12. [Crossref] [PubMed]
- LaPrade RF, Heikes C, Bakker AJ, et al. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am 2008;90:2069-76. [Crossref] [PubMed]
- LaPrade RF, Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clin Orthop Relat Res 2002;110-21. [Crossref] [PubMed]
- Lunden JB, Bzdusek PJ, Monson JK, et al. Current concepts in the recognition and treatment of posterolateral corner injuries of the knee. J Orthop Sports Phys Ther 2010;40:502-16. [Crossref] [PubMed]
- Moulton SG, Geeslin AG, LaPrade RF. A Systematic Review of the Outcomes of Posterolateral Corner Knee Injuries, Part 2: Surgical Treatment of Chronic Injuries. Am J Sports Med 2016;44:1616-23. [Crossref] [PubMed]
- Wentorf FA, LaPrade RF, Lewis JL, et al. The influence of the integrity of posterolateral structures on tibiofemoral orientation when an anterior cruciate ligament graft is tensioned. Am J Sports Med 2002;30:796-9. [Crossref] [PubMed]
- Arthur A, LaPrade RF, Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med 2007;35:1844-50. [Crossref] [PubMed]
- Laprade RF, Engebretsen L, Johansen S, et al. The effect of a proximal tibial medial opening wedge osteotomy on posterolateral knee instability: a biomechanical study. Am J Sports Med 2008;36:956-60. [Crossref] [PubMed]
- LaPrade RF, Ly TV, Wentorf FA, et al. The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med 2003;31:854-60. [Crossref] [PubMed]
- Terry GC, LaPrade RF. The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med 1996;24:732-9. [Crossref] [PubMed]
- Moatshe G, Slette EL, Engebretsen L, et al. Intertunnel Relationships in the Tibia During Reconstruction of Multiple Knee Ligaments: How to Avoid Tunnel Convergence. Am J Sports Med 2016;44:2864-9. [Crossref] [PubMed]
- LaPrade RF, Johansen S, Agel J, et al. Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am 2010;92:16-22. [Crossref] [PubMed]
Cite this article as: Cinque ME, DePhillipo NN, Kennedy MI, Aman ZS, Chahla J, LaPrade RF. Combined anterior cruciate ligament and posterolateral corner injuries: diagnosis and treatment. Ann Joint 2018;3:95.


