Management of patellofemoral instability in the setting of multiligament knee injury
Introduction
The term multiligament knee injury (MLKI) is used to describe combination injuries to the major knee ligament groups [anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), lateral collateral ligament (LCL) with possible involvement of the posterolateral corner (PLC), and medial collateral ligament (MCL) with possible involvement of the posteromedial corner (PMC)] (1,2). Multiligament knee injuries are relatively rare, accounting for only 0.02% to 0.2% of all orthopaedic injuries (3,4). These injuries most often present in the setting of a traumatic knee dislocation and can be associated with potentially limb threatening sequelae (e.g., neurovascular injury). In addition to the above mentioned ligamentous and neurovascular injuries, there is also possibility for injury to the soft tissue envelope stabilizing the patellofemoral joint (PFJ) (5,6).
In contrast, acute dislocations of the patella are relatively common and account for 2% to 3% of all knee injuries. They are the second most common cause of a traumatic hemarthrosis of the knee behind ACL disruption (7). The overwhelming majority of patellar dislocations are lateral (8). The vast majority of patellar dislocations most often occur in females 10 to 17 years old who participate in sporting activities (9). These injuries typically occur via a low-velocity, indirect mechanism in patients with underlying bony and soft tissue risk factors for patella instability (10,11).
There is a paucity of literature documenting the evaluation and treatment of patella instability in the setting of MLKI. In stark contrast to patella dislocation in the athletic population, the mechanism of injury is typically high velocity trauma, often in patients with normal underlying bony and soft tissue patellofemoral (PF) anatomy. A high index of suspicion is required to efficiently diagnose and effectively treat patella instability in the setting of a significant distracting ligamentous complex and/or neurovascular injury.
The purpose of this review is to provide a clinically relevant guide to the evaluation and management of patella instability in the setting of the MLKI. As will be shown, there are key differences in patient demographics, injury mechanism, presence of concomitant pathology as compared to isolated PF instability that influence prognosis, and treatment strategy. These differences must be appreciated during patient evaluation to appropriately formulate a rational management plan. Our goal is to highlight the aspects of patella instability unique to the knee dislocation population in order to help surgeons develop a framework for treating these complex and rare combination injury patterns.
Relevant PF joint anatomy and biomechanics
Related structures pertaining to MLKI
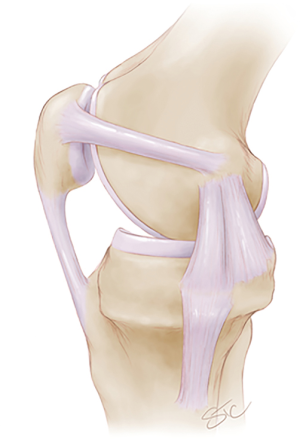
The PF joint consists of the patella, femoral trochlear groove, and surrounding soft tissue envelope. The major dynamic stabilizers of this joint include the quadriceps mechanism, core musculature, hip external rotators, and posterior chain (i.e., hamstrings) (12). The patella is a sesamoid bone that has the thickest articular cartilage in the body and increases the lever arm of the extensor mechanism (13). The trochlear groove is largely responsible for providing the inherent bony stability of the PFJ when the knee is in greater than 20 to 30 degrees of flexion (14). With respect to medial soft tissue PF restraints, the medial patellofemoral ligament (MPFL) is the strongest contributor to patellar stability from approximately 0 to 30 degrees of knee flexion (12,13,15). The MPFL is a thin transverse band of retinacular tissue that provides 50% to 60% of the restraining force against lateral patellar displacement (10,15). The MPFL origin on the femur is located in the saddle region between the adductor tubercle and the medial epicondyle; this is nearby to the origin of the MCL on the femur (Figure 1). It inserts onto the medial aspect of the proximal two-thirds of the patella (15,16). The MPFL is torn in nearly all cases of acute patellar dislocations (8,17). The medial patellomeniscal ligament (MPML), medial patellotibial ligament (MPTL), and medial retinaculum also assist in stabilizing the patella against lateral displacement, although to a much lesser degree than the MPFL (12). The lateral retinaculum is a primary stabilizer against medial patella translation and patella eversion, as well as a secondary stabilizer to excessive lateral translation.
Bony alignment parameters are important contributors to PF joint stability. Aberrant bony anatomy predisposes to instability at lower energy and is a risk factor for recurrence. Commonly encountered abnormalities include trochlear dysplasia, patella alta, lateralized force vector [i.e., elevated tibial tubercle-trochlear groove (TT-TG) distance], knee valgus, femoral anteversion, and external tibial torsion.
Clinical evaluation of PF instability in a MLKI setting
Multiligament knee injuries can be classified according to the mechanism of injury. High-velocity injuries occur as a result of direct trauma to the knee and are typically associated with motor vehicle and motorcycle accidents or falls from height (4,18). Low-velocity injuries typically occur during sporting events. These injuries are due to either a direct blow or twisting injury to the knee (19). Ultra-low-velocity injuries occur almost exclusively in obese patients. These injuries tend to occur as the result of seemingly innocuous rotational forces associated with relatively low-energy activities that exceed the knee ligaments’ inherent capacity to maintain normal joint integrity (20,21). Recognition of a MLKI is often challenging given that more than two-thirds of all knee dislocations spontaneously reduce prior to presentation (22). As a result, a high index of suspicion must be maintained when evaluating patients with traumatic knee injuries. Similarly, it is rare for the patella to be frankly dislocated on index presentation with combined MLKI. Clinical acumen combined with astute physical examination, examination under anesthesia, stress radiography, and other imaging modalities (i.e., MRI) are critical in recognizing this specific injury pattern.
Multiligament knee injuries can also be classified according to the number and laterality of the ligaments involved using the Schenck Knee Dislocation Classification system (2,23). This classification system has five tiers that progress in severity:
- Knee dislocation I (KD I) signifies injury to either the ACL or PCL.
- KD II indicates injury to both the ACL and PCL.
- KD III is subclassified based on whether the MCL (KD III-M) or LCL (KD III-L) is involved.
- KD IV means injury to the ACL, PCL, MCL, and LCL.
KD V is a knee fracture-dislocation (24).
Interestingly, there is no additional classification system for combined injuries to the extensor mechanism. These additional injuries may include rupture of the quadriceps and/or patella tendon or patella dislocation, with or without chondral or osteochondral injury.
All MLKI patients should be initially evaluated according to Advanced Trauma and Life Support (ATLS) principles. Vascular injury is relatively uncommon (1.6% to 12% incidence) but remains a significant concern in these patients; therefore, pedal pulses and ankle brachial indices (ABI) should be assessed, documented, and compared to the contralateral limb (25-28). Several studies suggest that physical exam alone may not be adequate to detect vascular injuries and thus recommend having a low threshold for further workup with arteriography (22,29). Nerve injury is a less severe but more common associated injury seen in 10% to 40% of patients presenting with a MLKI; the vast majority of these injuries involve the peroneal nerve (18,30).
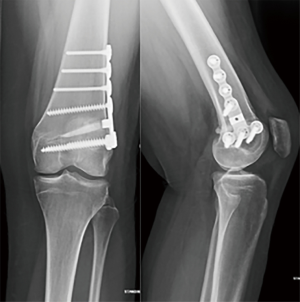
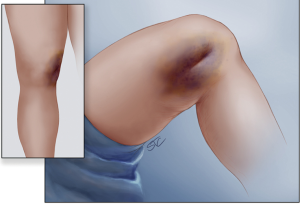
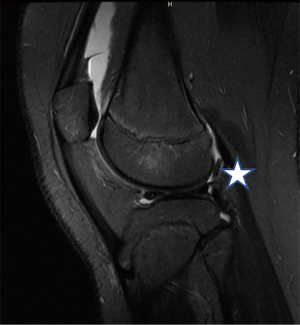
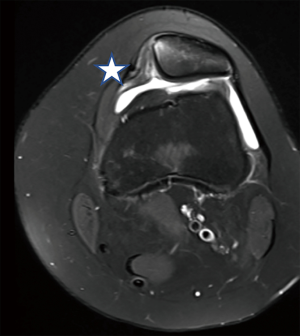
Clinical examination includes careful attention to asymmetric laxity compared to the opposite uninvolved extremity. In addition to specific laxity testing of the major ligament groups (i.e., ACL, PCL, PLC, PMC), specific laxity testing of the medial and lateral stabilizers of the PF joint should be performed. In the awake patient, competency of the extensor mechanism can be determined by the ability of the patient to perform a straight leg raise. Extensor lag or palpable defects in the extensor mechanism suggest fracture of the patella, rupture of the quadriceps tendon, patella tendon, or medial/lateral retinaculum. In the obtunded or multiply injured patient, clinical examination is best supplemented by careful review of advanced imaging studies to ensure intact extensor mechanism. PF laxity should be evaluated in full extension and throughout the range of motion (ROM) arc if at all possible. Patellar laxity and stability should be correlated with the degree of knee flexion at which both occur. Side-to-side differences in medial or lateral PF laxity should be noted, along with palpable defects or open injuries. Obstruction to normal PF mobility or skin puckering should also be noted as it may indicate a buttonholed medial retinaculum blocking reduction of a knee dislocation (31) (Figure 2). Excessive medial-to-lateral translation may indicate soft tissue injury to the medial PF restraints. Lateral sided patella eversion 20 degrees past horizontal or excessive medial-to-lateral patella translation is also pathologic and may indicate injury to the lateral retinaculum. Crepitus throughout a ROM arc or firm block to extension may indicate osteochondral injury or a loose body locked within the joint (Figure 3). Similar to the work-up of any MLKI, a standard trauma knee X-ray series should be obtained. MRI is helpful to evaluate for damage to the soft tissue structures, to rule out chondral or osteochondral injury and/or loose body, and to identify and quantify the presence of anatomic risk factors for recurrent PF instability (i.e., trochlear dysplasia, patella alta) (Figure 4).
Key differences
Between isolated PF instability and combined instability in the MLKI setting
It is critical to distinguish key features of patella dislocation combined with knee dislocation versus isolated PF instability. These differences are reviewed here and summarized in Table 1.

Full table
The patient demographics and injury mechanism of each group differs significantly. Acute, isolated patellar dislocations most commonly occur in young females aged 10 to 17 years who participate in sports (9,17). They tend to occur as the result of a low-velocity twisting injury in which the knee as a whole sustains relatively minor trauma (10,11). This is in sharp contrast to those who sustain MLKIs: males with an average age of 35 years who are involved in motor vehicle or motorcycle accidents. Multiligament knee injuries are most commonly the result of a high-energy mechanism in which the knee sustains a significant amount of trauma (32,33). Similarly, the vast majority of isolated PF instability cases are closed injuries in neurovascular intact patients; whereas open injuries to the PF soft tissue stabilizers are more commonly encountered in the MLKI population, with inherent increased risk to adjacent neurovascular structures.
As previously discussed, many patients with recurrent isolated patellar instability have underlying bony or soft abnormalities that predispose them to this condition (34). Common abnormalities include trochlear dysplasia, patella alta, a lateralized force vector, knee valgus, hyperlaxity, and/or vastus medialis obliquus (VMO) hypoplasia (12,15,34). In patients sustaining MLKIs, however, the majority of patients lack these predisposing factors for patellar instability (6). Most MLKI patients have normal underlying bony alignment in the PFJ, specifically regarding trochlear morphology and patella height. The energy required to dislocate with normal underlying anatomy is much greater than in patients with aberrant bony anatomy. Additionally, in patients with normal underlying anatomy, the risk of concurrent chondral shear injury or osteochondral fracture with loose body is higher as the energy of the injury increases. This is due to the fact that it takes more force to dislocate a normal joint than an abnormal joint with anatomic risk factors for PF instability. Consequently, MLKI patients have a higher risk of chondral or osteochondral injury with acute patella dislocation than their counterparts with isolated dislocation events.
As discussed, the MPFL is torn in greater than 94% of instability events regardless of underlying etiology. In isolated PF instability patients, the location of MPFL tear varies between the patella, mid-substance, and femoral origin. In contrast, the vast majority of MPFL tears in MLKI occur on the femoral side. In addition, the superficial MCL is torn in all cases of documented MPFL injury in MLKI patients, a finding that is rarely encountered in patients with isolated patella instability (6). This suggests more of a valgus moment causing the medial-sided injury in MLKI versus a predominant rotational-type injury in isolated patella dislocation. Interestingly, the most common bone bruise pattern following isolated dislocation seen on MRI involving the medial patella and lateral trochlea has not been appreciated with patella instability in patients with concomitant MLKI. Lastly, combined PF instability and MLKI patients typically have no antecedent history of patella instability whereas patients with isolated PF instability often suffer recurrent instability on the index or contralateral limb.
Treatment of patellar instability in the MLKI
To date, there is a paucity of literature to guide the treatment of patellar instability in the setting of a MLKI. Allen et al. retrospectively reviewed the records of all patients who underwent surgery for a MLKI over a 3-year period (6). There were a total of 51 patients treated with surgery for a MLKI, with pre-operative MRI showing an MPFL tear in 30 (59%) of these patients. Nine patients were lost to follow-up, leaving 21 patients available for comparison to a control group. The control group all had a surgically treated MLKI but with an intact MPFL. The majority of patients were male with an average age of 35.1 years. Based on the Schenck Knee Dislocation Classification, there were 6 KD I, 6 KD III-M, 2 KD III-L, 4 KD IV, and 3 KD V injuries. Thirteen patients had complete MPFL tears, 5 had high-grade partial tears, and 3 had partial tears. The majority of MPFL tears (76%) occurred in the proximal third of the ligament. The superficial MCL was torn in all of the patients with MPFL tears; however, the patellar or lateral femoral condyle bone bruising typically seen on MRI after a patellar dislocation was not identified in any of the patients. The average Caton-Deschamps ratio was the same in both groups, there were two patients in each group with trochlear dysplasia (grade A), and none of the patients reported patellar instability prior to their injury. Ten patients in the MPFL tear group underwent MCL repair (n=2) or reconstruction (n=8) at the time of MLKI reconstruction. None of the patients underwent MPFL repair or reconstruction. At final follow-up (mean 3.6 years), the average IKDC score was 79.4±16.1 in the isolated MLKI group vs. 65.5±22.9 in the MLKI group with MPFL tear (P=0.07). Only 1 (5%) patient complained of PF instability post-operatively. This patient had a KD III-L injury and a high-grade partial MPFL tear but did not undergo repair or reconstruction of the MCL. The authors concluded that MPFL injuries are commonly associated with MLKIs; however, their presence rarely leads to recurrent or symptomatic patellar instability. The authors acknowledge the limitations of their study due to the retrospective nature and small sample size; nonetheless, they should be applauded for investigating this under-researched topic and their study serves as a great starting point for further discussion and future research.
This study by Allen et al. (6) is, to our knowledge, the only one in the literature reporting on MPFL tears in the setting of a MLKI. As such, attempting to generalize a treatment strategy for patella instability in the setting of MLKI remains a difficult task due to the lack of substantial supporting evidence. It is useful to briefly summarize the evolving treatment algorithm for acute first-time dislocation in isolated PF instability in order to compare and contrast with the proposed algorithm for managing combined injury in the MLKI.
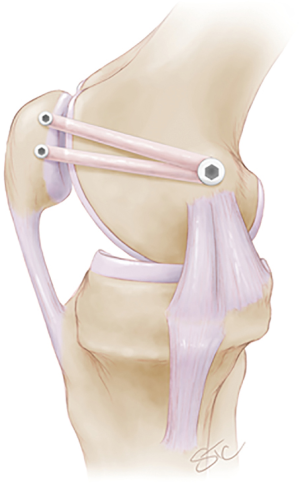
In the isolated PF dislocation cohort, most authors recommend non-operative treatment for first-time dislocators without osteochondral fracture or loose body. Several studies have demonstrated positive results following conservative management, with recurrent dislocation rates ranging from 13% to 52% (8,35), and 47% to 85% of patients reporting good or excellent subjective outcomes (36-38). However, there is a recognized subset of high-risk patients that may benefit from consideration for early surgical stabilization following a first dislocation without osteochondral injury. These patients are typically younger, participate in sports, and have high risk anatomy including trochlear dysplasia, patella alta, patella tilt, a lateralized force vector, and/or history of contralateral patella instability. Less controversial indications for early surgery include patients with a large loose body and/or osteochondral fracture for loose body removal and/or operative fixation of the osteochondral fragment. In this scenario, soft tissue stabilization is recommended to protect the fixation of the chondral surface. MPFL repair may be performed if the zone of injury is clearly demarcated with good tissue quality and normal underlying anatomy. If the injury to the medial restraints are diffuse with poor tissue quality, or if there is underlying high risk anatomy, MPFL reconstruction with autograft or allograft is preferred (Figure 5).
As discussed previously, the vast majority of MLKI patients with PF instability will have normal underlying anatomy and a clear zone of injury to the medial soft tissue restraints. In the case of open medial sided injury, buttonholing of the retinaculum blocking anatomic reduction, or osteochondral fracture/loose body, surgery is clearly indicated to address these abnormalities (Table 2). Open injury should undergo irrigation and debridement with provisional joint stabilization (i.e., external fixation) as indicated by other injury patterns. Operative repair of the torn medial soft tissue structures with absorbable monofilament suture is reasonable to consider at the time of surgery. Similarly, arthrotomy to remove buttonholed medial retinaculum in order to reduce a knee dislocation should include soft tissue repair of the medial PF stabilizers and remainder of medial soft tissue envelope. If an osteochondral injury requires arthrotomy and fixation, medial sided repair is also preferred to protect the fixation from further instability and recurrent injury.
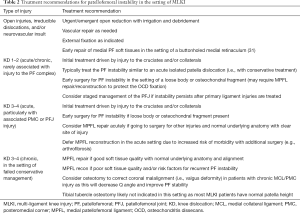
Full table
In the acute or subacute setting, if there is no bony block to motion, no open injury, and no osteochondral fracture, specific surgery for the MPFL may be avoided. This is particularly true in the setting of normal underlying anatomy (i.e., trochlear morphology and patella height), as the ligaments will likely heal at an acceptable resting length. In these cases, decision to operate should be dictated by other ligament groups (i.e., ACL/PCL/PMC/PLC) and not the PF joint. Concomitant injury to the MCL may also explain the very low rate of patellar instability following MLKI reconstruction (5%) vs. the relatively high rate of recurrent patellar instability following conservative treatment of isolated patellar dislocations (36%) (6,39). In the aforementioned study by Allen et al. (6), 10 of the 21 patients underwent concurrent MCL repair or reconstruction at the time of MLKI reconstruction and none of these patients experienced post-operative patellar instability. This certainly could have impacted the ultimate healing and stability of the MPFL; however, of the remaining 11 patients who did not undergo MCL repair or reconstruction, only one patient had patellar instability post-operatively. Therefore, it seems unlikely that surgically treating the torn MCL at the time of MLKI reconstruction has a significant impact on post-operative MPFL stability. Rather, concomitant injury to another structure (i.e., the MCL) in the area of the MPFL may further enhance the healing response and thus increase the chance of a stable patella post-operatively.
It is important to point out that more surgery in the face of high energy injury is not always desirable. It is well documented in the orthopedic literature that the more extensive the surgery around a joint, the greater the risk of post-operative arthrofibrosis. The incidence of knee stiffness is less than 5% of patients following an MPFL repair (40). In patients undergoing MLKI reconstruction without PF instability, the rate of knee stiffness already approaches 22% (41). The addition of an MPFL repair or reconstruction to an already substantially traumatized knee undergoing a multiligament reconstruction may dramatically increase the risk of post-operative arthrofibrosis (42). As noted by Allen et al. (6), the multiligament-injured knee undergoing reconstruction will experience a rather robust healing response (i.e., scar formation) due to both the nature of the injury itself as well as the surgery, which likely accounts for the lack of PF instability seen in these patients. Overall, caution must be exercised before offering an additional and potentially unnecessary procedure to an acute MLKI patient in order to avoid the increased risk of arthrofibrosis associated with extra surgery.
In the chronic setting, treatment of combined MLKI and PF instability should be based on the subjective sense of PF instability combined with objective evidence of symptomatic laxity on physical examination, and confirmed by imaging studies. If the MLKI has been previously stabilized, treatment of the PF joint may follow classic paradigms for management of isolated instability. If the MLKI needs to be addressed concomitantly, consideration for stabilizing the soft tissue envelope about the patella is important. With normal underlying anatomy and good tissue quality, MPFL imbrication may be performed to remove slack and restore the resting length of the medial PF complex (i.e., MPFL repair). In the setting of aberrant anatomy and/or poor tissue quality, MPFL reconstruction with allograft can be considered. Technical consideration must be taken regarding tunnel crowding about the medial epicondyle, particularly alongside concomitant MCL or PMC reconstruction. In the setting of chronic injury to PF restraints and PMC, coronal plane osteotomy may be considered prior to reconstruction to correct valgus and improve the Q-angle. Otherwise, there are few indications for other bony procedures in the management of chronic patella instability in MLKI (Figure 6).
Regarding patient reported outcomes, Allen et al. (6) shows that patients with MPFL tears did not have statistically worse IKDC scores than patients without MPFL tears. The magnitude of difference, however, was clinically significant, favoring those without MPFL tears. Given that all but one patient did not suffer patellar instability after surgery, injury to the MPFL is not the only contributing factor to the difference in IKDC scores. As previously noted, knees with MPFL injury likely sustained a higher level of trauma which could negatively impact outcomes.
Regarding rehabilitation of patella instability in the MLKI patient, specific precautions and restrictions are driven by the nature of the other ligament and/or chondral/meniscal injuries and not the status of the PF joint. Initial non-operative management of PF dislocation should focus on edema control and gentle ROM, followed by progressive strengthening of the quadriceps, core, hip rotators, and posterior chain musculature. For isolated MPFL repair or reconstruction, patients may begin weight bearing and ROM as tolerated immediately following surgery. Limitations in weight bearing or ROM may be given for fixation of osteochondral lesions at the surgeon’s discretion. In the MLKI patient, specific post-operative weight bearing and ROM restrictions are dictated by the multiligamentous nature of the injury as opposed to the PF joint. In the chronic setting, valgus correcting osteotomy typically requires early limitations in weightbearing prior to bony healing. There are no studies investigating the long-term return to activity in PF instability patients with concomitant MLKI. It is likely that return to normal activities of daily living, light physical activity, and full return to sport are delayed in MLKI patients compared to those with isolated PF instability (43).
Conclusions
PF instability in the setting of MLKI is relatively rare. There is a paucity of literature on the evaluation and management of this complex condition. It is critical to recognize that the patient population, mechanism of injury, and injury patterns in these MLKI patients differ from those with isolated PF instability. These patients are predominantly males in their mid-30s who sustain a high-velocity trauma to an otherwise normal PF joint. The majority of MPFL injuries occur on the femoral side along with concomitant MCL injury. Non-operative treatment of the PF injury in MLKI has led to good overall outcomes with minimal risk of recurrent PF instability. In the MLKI patient, medial PF soft tissue stabilization should be reserved for an open injury, a buttonholed medial retinaculum blocking reduction, an osteochondral fracture from patella dislocation, or chronic refractory PF instability symptoms. This strategy aims to minimize complications (e.g., arthrofibrosis) caused by early additional surgery, with the goal of improving outcomes for this challenging problem.
Acknowledgments
The authors would like to thank Steve C. Friedman, senior editor, and Stacy T. Cheavens, medical illustrator, University of Missouri Department of Orthopaedic Surgery, for assistance with the preparation of this article.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Camilo Partezani Helito and Jorge Chahla) for the series “The Multiligament Injured Knee” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.11.10). The series “The Multiligament Injured Knee” was commissioned by the editorial office without any funding or sponsorship. SLS reports personal fees from Joint Restoration Foundation, personal fees from Olympus, personal fees from Smith and Nephew, personal fees from Vericel, personal fees from Arthrex, personal fees from ConMed, personal fees from Flexion Therapeutics, personal fees from Vivorte, personal fees from Zimmer, personal fees from Bioventus, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Burrus MT, Werner BC, Griffin JW, et al. Diagnostic and Management Strategies for Multiligament Knee Injuries: A Critical Analysis Review. JBJS Rev 2016;4: [Crossref] [PubMed]
- Dwyer T, Marx RG, Whelan D. Outcomes of treatment of multiple ligament knee injuries. J Knee Surg 2012;25:317-26. [Crossref] [PubMed]
- Darcy G, Edwards E, Hau R. Epidemiology and outcomes of traumatic knee dislocations: Isolated vs multi-trauma injuries. Injury 2018;49:1183-7. [Crossref] [PubMed]
- Cook S, Ridley TJ, McCarthy MA, et al. Surgical treatment of multiligament knee injuries. Knee Surg Sports Traumatol Arthrosc 2015;23:2983-91. [Crossref] [PubMed]
- Krych AJ, Sousa PL, King AH, et al. Meniscal tears and articular cartilage damage in the dislocated knee. Knee Surg Sports Traumatol Arthrosc 2015;23:3019-25. [Crossref] [PubMed]
- Allen BJ, Krych AJ, Engasser W, et al. Medial patellofemoral ligament tears in the setting of multiligament knee injuries rarely cause patellar instability. Am J Sports Med 2015;43:1386-90. [Crossref] [PubMed]
- Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res 2007;93-101. [Crossref] [PubMed]
- Kang HJ, Wang F, Chen BC, et al. Non-surgical treatment for acute patellar dislocation with special emphasis on the MPFL injury patterns. Knee Surg Sports Traumatol Arthrosc 2013;21:325-31. [Crossref] [PubMed]
- Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114-21. [Crossref] [PubMed]
- Sillanpaa PJ, Maenpaa HM. First-time patellar dislocation: surgery or conservative treatment? Sports Med Arthrosc Rev 2012;20:128-35. [Crossref] [PubMed]
- Nikku R, Nietosvaara Y, Aalto K, et al. The mechanism of primary patellar dislocation: trauma history of 126 patients. Acta Orthop 2009;80:432-4. [Crossref] [PubMed]
- Sherman SL, Plackis AC, Nuelle CW. Patellofemoral anatomy and biomechanics. Clin Sports Med 2014;33:389-401. [Crossref] [PubMed]
- Koh JL, Stewart C. Patellar instability. Orthop Clin North Am 2015;46:147-57. [Crossref] [PubMed]
- Amis AA, Oguz C, Bull AM, et al. The effect of trochleoplasty on patellar stability and kinematics: a biomechanical study in vitro. J Bone Joint Surg Br 2008;90:864-9. [Crossref] [PubMed]
- Panni AS, Vasso M, Cerciello S. Acute patellar dislocation. What to do? Knee Surg Sports Traumatol Arthrosc 2013;21:275-8. [Crossref] [PubMed]
- Amis AA, Firer P, Mountney J, et al. Anatomy and biomechanics of the medial patellofemoral ligament. Knee 2003;10:215-20. [Crossref] [PubMed]
- Sherman SL, Deasis DP, Garrone AJ, et al. Return to Play after Patellar Stabilization. Curr Rev Musculoskelet Med 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Johnson ME, Foster L, DeLee JC. Neurologic and vascular injuries associated with knee ligament injuries. Am J Sports Med 2008;36:2448-62. [Crossref] [PubMed]
- Shelbourne KD, Klootwyk TE. Low-velocity knee dislocation with sports injuries. Treatment principles. Clin Sports Med 2000;19:443-56. [Crossref] [PubMed]
- Werner BC, Gwathmey FW Jr, Higgins ST, et al. Ultra-low velocity knee dislocations: patient characteristics, complications, and outcomes. Am J Sports Med 2014;42:358-63. [Crossref] [PubMed]
- Azar FM, Brandt JC, Miller RH 3rd, et al. Ultra-low-velocity knee dislocations. Am J Sports Med 2011;39:2170-4. [Crossref] [PubMed]
- Stannard JP, Bauer KL. Current concepts in knee dislocations: PCL, ACL, and medial sided injuries. J Knee Surg 2012;25:287-94. [Crossref] [PubMed]
- Ferrari MB, Chahla J, Mitchell JJ, et al. Multiligament Reconstruction of the Knee in the Setting of Knee Dislocation With a Medial-Sided Injury. Arthrosc Tech 2017;6:e341-50. [Crossref] [PubMed]
- Schenck RC Jr, Richter DL, Wascher DC. Knee Dislocations: Lessons Learned From 20-Year Follow-up. Orthop J Sports Med 2014;2:2325967114534387 [Crossref] [PubMed]
- Sillanpaa PJ, Kannus P, Niemi ST, et al. Incidence of knee dislocation and concomitant vascular injury requiring surgery: a nationwide study. J Trauma Acute Care Surg 2014;76:715-9. [Crossref] [PubMed]
- Natsuhara KM, Yeranosian MG, Cohen JR, et al. What is the frequency of vascular injury after knee dislocation? Clin Orthop Relat Res 2014;472:2615-20. [Crossref] [PubMed]
- Stannard JP, Sheils TM, Lopez-Ben RR, et al. Vascular injuries in knee dislocations: the role of physical examination in determining the need for arteriography. J Bone Joint Surg Am 2004;86-A:910-5. [Crossref] [PubMed]
- Boisrenoult P, Lustig S, Bonneviale P, et al. Vascular lesions associated with bicruciate and knee dislocation ligamentous injury. Orthop Traumatol Surg Res 2009;95:621-6. [Crossref] [PubMed]
- Mills WJ, Barei DP, McNair P. The value of the ankle-brachial index for diagnosing arterial injury after knee dislocation: a prospective study. J Trauma 2004;56:1261-5. [Crossref] [PubMed]
- Cho D, Saetia K, Lee S, et al. Peroneal nerve injury associated with sports-related knee injury. Neurosurg Focus 2011;31:E11 [Crossref] [PubMed]
- Capito N, Gregory MH, Volgas D, et al. Evaluation and management of an irreducible posterolateral knee dislocation. J Knee Surg 2013;26:S136-41. [Crossref] [PubMed]
- Moatshe G, Dornan GJ, Loken S, et al. Demographics and Injuries Associated With Knee Dislocation: A Prospective Review of 303 Patients. Orthop J Sports Med 2017;5:2325967117706521 [Crossref] [PubMed]
- Kupczik F, Schiavon ME, Vieira LA, et al. Knee Dislocation: Descriptive Study of Injuries. Revista Brasileira de Ortopedia 2013;48:145-51. [Crossref]
- Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med 2002;21:499-519. [Crossref] [PubMed]
- Buchner M, Baudendistel B, Sabo D, et al. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med 2005;15:62-6. [Crossref] [PubMed]
- Nikku R, Nietosvaara Y, Aalto K, et al. Operative treatment of primary patellar dislocation does not improve medium-term outcome: A 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop 2005;76:699-704. [Crossref] [PubMed]
- Christiansen SE, Jakobsen BW, Lund B, et al. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy 2008;24:881-7. [Crossref] [PubMed]
- Palmu S, Kallio PE, Donell ST, et al. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am 2008;90:463-70. [Crossref] [PubMed]
- Christensen TC, Sanders TL, Pareek A, et al. Risk Factors and Time to Recurrent Ipsilateral and Contralateral Patellar Dislocations. Am J Sports Med 2017;45:2105-10. [Crossref] [PubMed]
- Arshi A, Cohen JR, Wang JC, et al. Operative Management of Patellar Instability in the United States: An Evaluation of National Practice Patterns, Surgical Trends, and Complications. Orthop J Sports Med 2016;4:2325967116662873 [Crossref] [PubMed]
- Hanley J, Westermann R, Cook S, et al. Factors Associated with Knee Stiffness following Surgical Management of Multiligament Knee Injuries. J Knee Surg 2017;30:549-54. [Crossref] [PubMed]
- Marom N, Ruzbarsky JJ, Roselaar N, et al. Knee MLI Injuries: Common Problems and Solutions. Clin Sports Med 2018;37:281-91. [Crossref] [PubMed]
- Harner CD, Waltrip RL, Bennett CH, et al. Surgical management of knee dislocations. J Bone Joint Surg Am 2004;86-A:262-73. [Crossref] [PubMed]
Cite this article as: Sherman SL, Oladeji LO, Welsh J, DiPaolo ZJ. Management of patellofemoral instability in the setting of multiligament knee injury. Ann Joint 2018;3:100.