
Managing acromial fractures: prevention and treatment, both nonoperative and operative
Introduction
The utilization of total shoulder arthroplasty (TSA) and specifically reverse shoulder arthroplasty (RSA) has increased steadily over the past decades (1-3). As the indications for RSA have continued to expand, so has the prevalence of this procedure. While traditionally RSA was reserved for patients with end stage rotator cuff arthropathy, indications have expanded to also include many other pathologies (4,5). As the number of RSAs being performed increases, inevitably so will the number of complications.
A number of intra-operative and post-operative complications have been described in RSA, with overall complication rates estimated at 19 percent for primary RSA and up to 69 percent for revision RSA procedures (6,7). Some of the more common complications include scapular notching, glenoid component loosening, infection, instability, and fracture (8). Periprosthetic fractures of the humeral shaft, greater tuberosity, coracoid, acromion, and scapular spine have all been described (9,10). Acromial and scapular spine fractures have been associated with significantly worse functional outcomes after RSA and are a major cause of post-operative dysfunction and/or pain in these patients (11-13).
Acromial and scapular spine fractures occur in 3.1% to 11.2% of all patients undergoing RSA (Table 1) (11-18,20). While a number of risk factors have been proposed, there is a relative paucity of quality evidence in the literature on the cause of this complication. The purpose of this article is to highlight the risk factors for scapular spine and acromial fractures in patients undergoing RSA and discuss treatment and prevention options based on current literature.
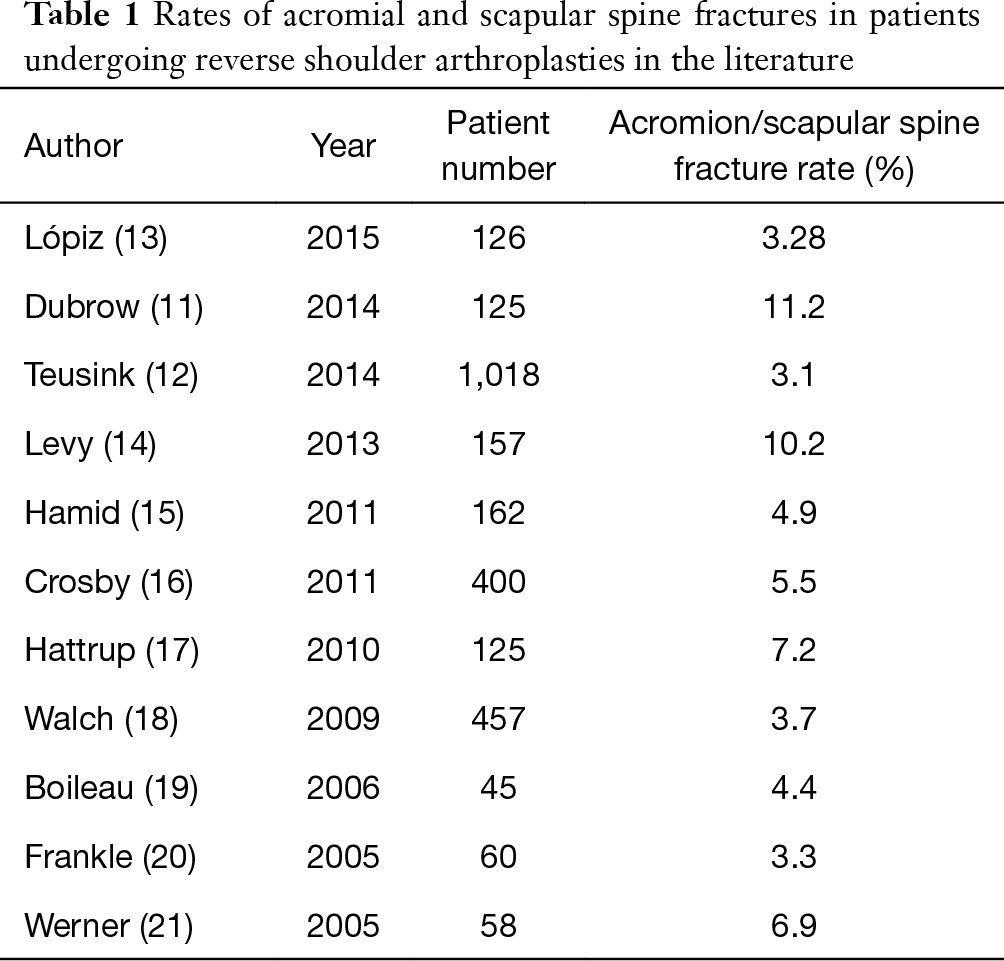
Full table
Clinical presentation, diagnosis, and classification
Acromial fractures and scapular spine fractures may occur intra-operatively or post-operatively in association with RSA. Intra-operative fractures are rare and may be treated conservatively or with acute fixation depending on location and displacement of the fracture as well as implant stability. Post-operative fractures present differently, and may be due to a direct trauma or a chronic fatigue type of mechanism (17). Patients with a traumatic mechanism often report a fall or an event requiring them to reach out and grab something to prevent a fall. This mechanism suggests that the mechanism for these types of fractures may be from rapid deltoid contraction.
Patients with acromial stress fractures often present with a period of initial pain relief post-operatively followed by an increase in pain and poor function (22). It is well established that RSA patients who sustain acromial or scapular spine fractures have worse outcomes compared to patients without fractures. Lópiz et al. showed a significant decreased in Constant scores, lower quality of life scores, and an average decrease of 39 degree of forward flexion and 34 degrees of abduction compared to control patients (13). Similarly, Teusink et al. showed a higher revision surgery rate, less overall improvement in American Shoulder and Elbow Surgeons (ASES) score (58.0 compared to 74.2), and worse range of motion improvement (26 degrees compared to 76 degrees) (12). The success of an RSA is reliant on a functional deltoid, and significant deltoid dysfunction and loss of tension may occur with displaced fractures of the deltoid origin on the acromion or scapular spine. The time period in which these fractures occur varies anywhere from 1 to 94 months post-operatively, with the average typically between 3 and 12 months (12-14). Many patients with acromion fractures are a diagnostic challenge as their clinical exam is ambiguous and radiographs are normal or have subtle findings.
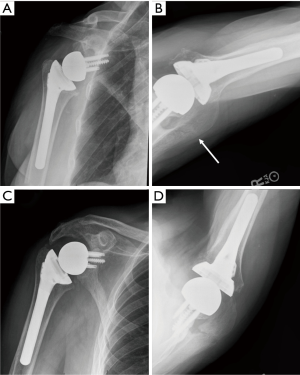
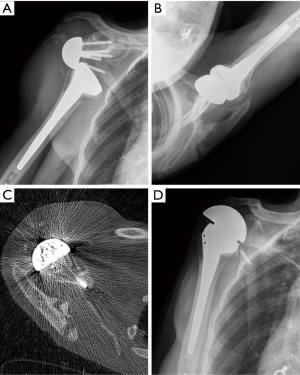
Routine shoulder plain radiographs are the initial diagnostic imaging tool but only have a sensitivity of 79% and poor interobserver reliability (14,23). Therefore, early advanced imaging is indicated in patients presenting with a high clinical suspicion for scapula fractures. Computed tomography is the advanced image study that best identifies fractures not apparent on plain radiographs, but magnetic resonance imaging (MRI) or bone scans can be helpful for stress fractures or stress reactions. Figures 1 and 2 demonstrate radiographs and advanced imaging in two case examples.
Crosby et al. proposed a classification for acromion fractures after RSA after retrospectively reviewing 400 patients, 22 of which sustained acromion or scapular spine fractures. Type I fractures are small anterior fractures at the level of the acromioclavicular (AC) joint and were hypothesized to be secondary to deltoid avulsion from a weakened acromion. Type II fractures are posterior to the AC joint and were thought to be due to fatigue failure of the acromion. Type III fractures are in the posterior acromion or scapular spine and were all related to a traumatic event in their series (16). Levy et al. has also proposed another classification system based on the amount of deltoid origin involvement that is depicted in Table 2 (14).
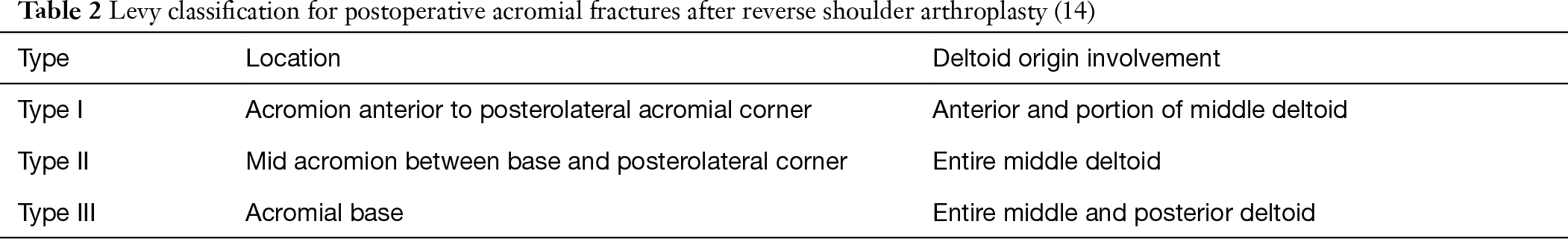
Full table
Risk factors
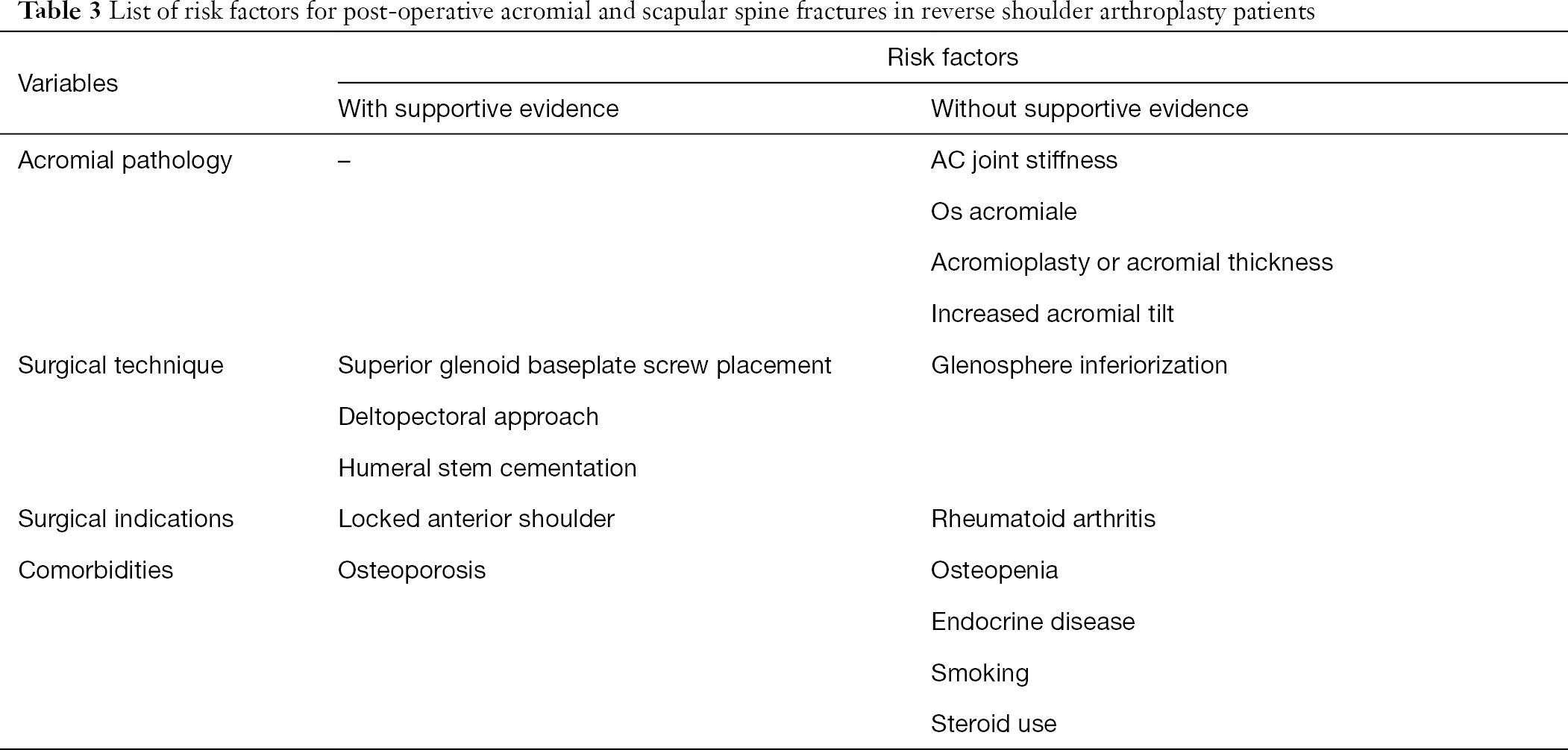
The first step in appropriately managing and preventing acromion fractures in RSA patients is to mitigate possible risk factors. Risk factors can be classified into surgical indication, patient comorbidities, acromial pathology, and surgical technique.
Surgical indication
The indications for RSA have been expanded over the past decades, and with this more complicated patients are getting reverse shoulder arthroplasties (4,5). One particular example is locked anterior shoulder with static instability and anterior glenoid bone loss. This group of patients develop soft tissue contractures that may place an increased load on the acromion, and have a higher fracture incidence at 21 percent (24). Rheumatoid arthritis patients have a higher risk of intra-operative fractures during RSA; however, post-operative acromial fracture rate appears to be similar to non-rheumatoid patients (10,25,26).
Comorbidities
Certain medical comorbidities may increase the risk of acromial fractures in RSA patients. One retrospective case-control study looked at comorbidities in relation to acromial fractures and found the osteoporosis significantly increased the risk; however, no increased risk of fracture existed in patient with osteopenia, endocrine disease, autoimmune disease, smoking, alcohol abuse, or steroid use (23). Definitive conclusions are difficult to make based on such a rare complication, and it is likely that all medical comorbidities that cause decreased bone strength or bone metabolic changes increase the risk of acromion fractures to some degree. Additionally, patients at an increased risk of falling are at higher risk of sustaining an acromial or scapular spine fracture after RSA.
Acromial pathology
Pre-operative pathology in the acromion such as os acromiale, acromial thickness, acromial tilt, or prior acromioplasty may weaken the bone, theoretically putting it at an increased risk of fracture (18,27). Several retrospective series have studied these particular risk factors. Walch et al. compared 23 patients with os acromiale and 17 patients with pre-operative acromion fracture or fragmentation to patients without these lesions and found no significant difference in outcomes nor an increased risk of post-operative fractures (18). Otto et al. studied 53 RSA patients that sustained post-operative scapular fractures and found no differences in acromial thickness or acromial tilt when compared to non-fractured RSA patients (23).
Crosby et al. proposed AC joint stiffness as a predisposing factor for acromial fractures, specifically in type II fractures (16). AC joint stiffness has only been evaluated critically in one study by Dubrow et al. The authors found no significant difference in radiographic presence of AC degenerative changes in patients with acromial fractures and those without (11). The applicability of these results is difficult to assess due to the low sample size and subjective nature of assessing AC stiffness radiographically. Therefore, it is uncertain if the presence of AC arthritis or stiffness is a risk factor for acromial fractures in RSA patients.
Surgical technique
Several intra-operative factors may also increase the risk of acromial fractures in RSA patients. Several studies have related displaced fractures of the base of the scapular spine to the superior glenoid baseplate screw. The screw being too long or exiting at the scapular spine base may cause increased stress in the scapular spine causing a fracture (16,22,23).
Another factor that may contribute is placing excessive tension on the deltoid by distalizing the center of rotation and lengthening the arm. Biomechanically this gives the deltoid a better lever arm for elevation and was one of the original goals in RSA (28). This effectively lengthens the arm and the deltoid, placing increased stress on the acromion and scapular spine. Studies have used objective radiographic measurements such as glenoid-to-tuberosity distance, acromion-to-tuberosity or acromiohumeral distance, and arm length to quantify and reproduce this. However, to date no study has shown that increased arm lengthening or increasing deltoid tension does put the acromion at an increased risk of fracture (11,23,29). Furthermore, inadequate deltoid tension is associated with increased risk of prosthetic instability (29).
Several other surgical factors have been reported as a risk for post-operative acromial fractures in RSA. Phadnis et al. compared results in cemented vs. uncemented humeral stems and found that cemented humeral stems were associated with more acromion fractures in a retrospective review (30). In another retrospective series, Molé et al. demonstrated a higher fracture rate in the deltopectoral approach compared to the anterosuperior approach (5.6% vs. 2.2%) (31). However, without randomized controlled trials, the true risk associated with cementation and approach is unknown.
Prevention
A number of risk factors have been identified as being associated with post-operative acromial spine fractures (Table 3). As this is a relatively infrequent complication in RSA, the evidence in support of each risk factor is generally poor, making prevention of acromion fractures difficult. Prevention strategies can be grouped into mitigation of patient factors and surgical technique.
Full table
Patient factors are difficult to control. As RSA is typically an end-stage treatment, other lower risk procedures have already been attempted or are not indicated. Surgeons should carry a high index of suspicion when offering RSA to patients presenting with a chronic locked anterior shoulder dislocation, as the incidence of acromial fractures is higher in this group. Optimization of bone health in osteoporotic individuals with appropriate medical management and bisphosphonate use may help mitigate risk in this patient population. Abnormal pre-operative acromial morphology such as decreased acromial thickness, acromial tilt, AC joint stiffness, or os acromiale has not been shown to increase risk of post-operative fractures and therefore should not preclude patients from getting surgery.
Surgical technique may play a role in preventing acromial and scapular spine fractures during and after RSA. The superior glenoid baseplate screw has been shown to be associated with scapular spine fractures, especially those occurring at the base of the scapular spine (16,22,23). This may be prevented by ensuring this screw is of appropriate length and trajectory with a maximum length of 24 mm and avoiding a posterior trajectory (22). It may also be prevented by not placing the superior screw at all as long as the remaining screws have adequate purchase (32). Regarding surgical approach, while one study demonstrated that the anterosuperior approach may have a lower rate of acromial fractures and post-operative instability, the rate of implant loosening and scapular notching was higher with this approach (31). It is recommended that the surgeon utilizes the approach that he or she is most comfortable with.
While deltoid lengthening has been shown to improve post-operative function in RSA patients, this may also predispose patients to acromial fractures or deltoid fatigue from overlengthening (33-35). While no definitive evidence has shown that increasing the deltoid tension may predispose RSA patients to acromial fractures, it is still recommended to limit arm lengthening to 2.5 centimeters to mitigate the risk of possible acromion fracture, neurologic injury, or deltoid weakening (29,33,36). This may be achieved by avoiding excessive inferior placement of the baseplate/glenosphere and choosing a humeral component design that does not excessively distalize the humerus (37).
Treatment
Treatment of scapular spine and acromial fractures in RSA patients can be generally grouped into conservative treatment and operative fixation. Conservative management is the standard treatment for acute, non-displaced fractures of the scapula, with a recent survey of ASES members demonstrating that 74 percent prefer conservative management (15). Nonsurgical treatment involves a period of immobilization for six weeks, followed by progressive range of motion (12-15,22). During this period, gentle pendulum exercises may be allowed, but no active motion due to high risk of fracture displacement (16). Conservative management has yielded nonunion rates as high as 50 to 75 percent, calling into question this treatment modality (12,13,15). Some surgeons advocate that patients may go on to a painless nonunion and have acceptable results (15).
Certain fracture patterns are better treated with operative management. Displaced fractures and fractures at the base of the scapular spine are prone to poor outcomes due to the larger amount of deltoid insertion involvement. A fracture at the base of the scapular spine will involve roughly two thirds of the deltoid origin. When a fracture in this region displaces, deltoid tension is lost and function of the RSA suffers significantly (23,38). A variety of surgical fixation methods have been described in the literature for acromial fractures in RSA patients. While tension band wiring is a described technique, the deltoid muscle is not a simple single plane tension force vector which may contribute to failure of this technique (18,22,39). Some fractures of the lateral acromion have little area for screw purchase, in which case a tension band construct may be the only feasible option. Most surgeons favor rigid plate fixation when treating these fractures operatively. Rouleau et al. described a technique of dual orthogonal plating of a scapular spine base fracture with excellent results (40). Hess et al. described a technique of bending a cruciform pilon plate over the acromion to place a retrograde lag screw across the fracture (41). Hill et al. described a series of 13 patients with acromion or scapular spine fractures in native scapulae that underwent fixation with a 2.7- or 3.5-mm lag screw and a neutralization reconstruction plate with 100 percent union rate and good overall outcomes (42).
A consensus treatment plan for acromial and scapular spine fractures in RSA patients does not exist as no studies have been published comparing fixation techniques or operative and nonoperative management. The majority of literature includes case series of less than five patients, from which little clinical judgement can be made. In the absence of any comparative trials, our institution recommends treating nondisplaced fractures of the acromion and scapular spine conservatively with six weeks of immobilization followed by progressive shoulder motion. In the setting of painful nonunion or displaced fractures, we recommend surgical fixation with dual orthogonal plating when possible.
Conclusions
Scapular spine and acromial fractures after RSA can be difficult to diagnose and are challenging to treat. We recommend early advanced imaging with a CT scan if the clinical suspicion for a fracture exists despite normal radiographs. It is important for the surgeon to be cognizant of potential risk factors and certain patient characteristics that may contribute to acromial and scapular spine fractures such as osteoporosis, locked anterior shoulder dislocations, inflammatory arthritis, and severe AC joint arthrosis and stiffness. Surgical techniques to prevent these fractures include avoiding aberrant placement of the superior glenoid baseplate screw and avoiding implant placement that may excessively distalize the humerus. Treatment of acromial and scapular spine fractures in RSA patients is typically conservative with shoulder immobilization except in cases of displaced fractures or painful nonunions. In these cases, rigid fixation offers the best chance of achieving union. Future comparative studies are needed to guide management in acromial and scapular spine fractures associated with RSA.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Joseph A. Abboud) for the series “Evolving Trends in Reverse Shoulder Arthroplasty” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.12.03). The series “Evolving Trends in Reverse Shoulder Arthroplasty” was commissioned by the editorial office without any funding or sponsorship. AJS reports personal fees from Medacta, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Day JS, Lau E, Ong KL, et al. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg 2010;19:1115-20. [Crossref] [PubMed]
- Westermann RW, Pugely AJ, Martin CT, et al. Reverse Shoulder Arthroplasty in the United States: A Comparison of National Volume, Patient Demographics, Complications, and Surgical Indications. Iowa Orthop J 2015;35:1-7. [PubMed]
- Schairer WW, Nwachukwu BU, Lyman S, et al. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 2015;24:91-7. [Crossref] [PubMed]
- Hyun YS, Huri G, Garbis NG, et al. Uncommon Indications for Reverse Total Shoulder Arthroplasty. Clin Orthop Surg 2013;5:243. [Crossref] [PubMed]
- Urch E, Dines JS, Dines DM. Emerging Indications for Reverse Shoulder Arthroplasty. Instr Course Lect 2016;65:157-69. [PubMed]
- Wall B, Nové-Josserand L, O’Connor DP, et al. Reverse Total Shoulder Arthroplasty: A Review of Results According to Etiology. J Bone Joint Surg Am 2007;89:1476. [PubMed]
- Saltzman BM, Chalmers PN, Gupta AK, et al. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2014;23:1647-54. [Crossref] [PubMed]
- Farshad M, Gerber C. Reverse total shoulder arthroplasty-from the most to the least common complication. Int Orthop 2010;34:1075-82. [Crossref] [PubMed]
- Cheung E, Willis M, Walker M, et al. Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg 2011;19:439-49. [Crossref] [PubMed]
- Young AA, Smith MM, Bacle G, et al. Early Results of Reverse Shoulder Arthroplasty in Patients with Rheumatoid Arthritis. J Bone Joint Surg Am 2011;93:1915-23. [Crossref] [PubMed]
- Dubrow S, Streit JJ, Muh S, et al. Acromial Stress Fractures: Correlation With Acromioclavicular Osteoarthritis and Acromiohumeral Distance. Orthopedics 2014;37:e1074-9. [Crossref] [PubMed]
- Teusink MJ, Otto RJ, Cottrell BJ, et al. What is the effect of postoperative scapular fracture on outcomes of reverse shoulder arthroplasty? J Shoulder Elbow Surg 2014;23:782-90. [Crossref] [PubMed]
- Lópiz Y, Rodríguez-González A, García-Fernández C, et al. Fracturas de estrés de la escápula tras artroplastia invertida en artropatía de manguito: ¿cuál es su repercusión funcional? Rev Esp Cir Ortop Traumatol 2015;59:318-25. [Crossref] [PubMed]
- Levy JC, Anderson C, Samson A. Classification of postoperative acromial fractures following reverse shoulder arthroplasty. J Bone Joint Surg Am 2013;95:e104 [Crossref] [PubMed]
- Hamid N, Connor PM, Fleischli JF, et al. Acromial fracture after reverse shoulder arthroplasty. Am J Orthop (Belle Mead NJ) 2011;40:E125-9. [PubMed]
- Crosby LA, Hamilton A, Twiss T. Scapula Fractures After Reverse Total Shoulder Arthroplasty: Classification and Treatment. Clin Orthop Relat Res 2011;469:2544-9. [Crossref] [PubMed]
- Hattrup SJ. The Influence of Postoperative Acromial and Scapular Spine Fractures on the Results of Reverse Shoulder Arthroplasty. Orthopedics 2010;33: [Crossref] [PubMed]
- Walch G, Mottier F, Wall B, et al. Acromial insufficiency in reverse shoulder arthroplasties. J Shoulder Elbow Surg 2009;18:495-502. [Crossref] [PubMed]
- Boileau P, Watkinson D, Hatzidakis AM, et al. Neer Award 2005: The Grammont reverse shoulder prosthesis: Results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 2006;15:527-40. [Crossref] [PubMed]
- Frankle M, Siegal S, Pupello D, et al. The Reverse Shoulder Prosthesis for Glenohumeral Arthritis Associated with Severe Rotator Cuff Deficiency: A Minimum Two-Year Follow-up Study of Sixty Patients. J Bone Joint Surg Am 2005;87:1697-705. [PubMed]
- Werner CM, Steinmann PA, Gilbart M, et al. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am 2005;87:1476-86. [PubMed]
- Mayne IP, Bell SN, Wright W, et al. Acromial and scapular spine fractures after reverse total shoulder arthroplasty. Shoulder Elbow 2016;8:90-100. [Crossref] [PubMed]
- Otto RJ, Virani NA, Levy JC, et al. Scapular fractures after reverse shoulder arthroplasty: evaluation of risk factors and the reliability of a proposed classification. J Shoulder Elbow Surg 2013;22:1514-21. [Crossref] [PubMed]
- Kurowicki J, Triplet JJ, Momoh E, et al. Reverse shoulder prosthesis in the treatment of locked anterior shoulders: a comparison with classic reverse shoulder indications. J Shoulder Elbow Surg 2016;25:1954-60. [Crossref] [PubMed]
- Jauregui JJ, Paul Hovis J, Ashfaq Hasan S. Characteristics of rheumatoid arthritis patients undergoing reverse shoulder arthroplasty. Clin Rheumatol 2018;37:339-43. [Crossref] [PubMed]
- Gee ECA, Hanson EK, Saithna A. Reverse Shoulder Arthroplasty in Rheumatoid Arthritis: A Systematic Review. Open Orthop J 2015;9:237-45. [Crossref] [PubMed]
- Mottier F, Wall B, Nové-Josserand L, et al. Reverse prosthesis and os acromiale or acromion stress fracture. Rev Chir Orthop Reparatrice Appar Mot 2007;93:133-41. [Crossref] [PubMed]
- Grammont P, Trouilloud P, Laffay J. Concept study and realization of a new total shoulder prosthesis. Rhumatologie 1987;39:407-18.
- Lädermann A, Williams MD, Melis B, et al. Objective evaluation of lengthening in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2009;18:588-95. [Crossref] [PubMed]
- Phadnis J, Huang T, Watts A, et al. Cemented or cementless humeral fixation in reverse total shoulder arthroplasty? Bone Joint J 2016;98-B:65-74. [Crossref] [PubMed]
- Molé D, Favard L. Excentered scapulohumeral osteoarthritis. Rev Chir Orthop Reparatrice Appar Mot 2007;93:37-94. [PubMed]
- James J, Allison MA, Werner FW, et al. Reverse shoulder arthroplasty glenoid fixation: is there a benefit in using four instead of two screws? J Shoulder Elbow Surg 2013;22:1030-6. [Crossref] [PubMed]
- Lädermann A, Walch G, Lubbeke A, et al. Influence of arm lengthening in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2012;21:336-41. [Crossref] [PubMed]
- Jobin CM, Brown GD, Bahu MJ, et al. Reverse total shoulder arthroplasty for cuff tear arthropathy: the clinical effect of deltoid lengthening and center of rotation medialization. J Shoulder Elbow Surg 2012;21:1269-77. [Crossref] [PubMed]
- Sabesan VJ, Lombardo D, Josserand D, et al. The effect of deltoid lengthening on functional outcome for reverse shoulder arthroplasty. Musculoskelet Surg 2016;100:127-32. [Crossref] [PubMed]
- Wright J, Potts C, Smyth MP, et al. A quantitative analysis of the effect of baseplate and glenosphere position on deltoid lengthening in reverse total shoulder arthroplasty. Int J Shoulder Surg 2015;9:33-7. [Crossref] [PubMed]
- Onstot BR, Jacofsky MC, Hansen ML. Muscle force and excursion requirements and moment arm analysis of a posterior-superior offset reverse total shoulder prosthesis. Bull Hosp Jt Dis 2013;2013:S25-30. [PubMed]
- Levy JC, Blum S. Postoperative acromion base fracture resulting in subsequent instability of reverse shoulder replacement. J Shoulder Elbow Surg 2012;21:e14-8. [Crossref] [PubMed]
- Wahlquist TC, Hunt AF, Braman JP. Acromial base fractures after reverse total shoulder arthroplasty: report of five cases. J Shoulder Elbow Surg 2011;20:1178-83. [Crossref] [PubMed]
- Rouleau DM, Gaudelli C. Successful treatment of fractures of the base of the acromion after reverse shoulder arthroplasty: Case report and review of the literature. Int J Shoulder Surg 2013;7:149-52. [Crossref] [PubMed]
- Hess F, Zettl R, Smolen D, et al. Anatomical reconstruction to treat acromion fractures following reverse shoulder arthroplasty. Int Orthop 2018;42:875-81. [Crossref] [PubMed]
- Hill BW, Anavian J, Jacobson AR, et al. Surgical Management of Isolated Acromion Fractures. J Orthop Trauma 2014;28:e107-13. [Crossref] [PubMed]
Cite this article as: Joyce CD, Seidl AJ. Managing acromial fractures: prevention and treatment, both nonoperative and operative. Ann Joint 2019;4:1.


