Acute proximal tibiofibular joint dislocation: a sports related injury?—two different cases
Introduction
Proximal tibiofibular joint (PTFJ) is a stable joint due to bony congruency and ligamentous and muscle support (1,2). Nonetheless, it has a wide morphological variability (3,4) as shown by Ogden, in his published study in cadavers (5,6), dividing it in two types of joints: horizontal and oblique. The horizontal configuration, defined as less than 20-degree of joint surface inclination in relation to the horizontal plane, is associated with increased rotational mobility being more resistant to rotational forces than the oblique configuration that has less rotational mobility resulting in smaller joint surface.
Acute PTFJ dislocation is a rare condition, accounting for less than 1% of all knee injuries (7), mostly seen in 17–30 years old males (8), during sports activity. It is thought that there is an underestimated prevalence of this condition due to misdiagnosis as radiographs are not always clear.
The mechanism of injury is often a twisting of the knee with inversion and plantar flexion of the foot with simultaneous knee flexion and external rotation of the leg (9,10). It occurs usually during sports activity, or more rarely, following direct high-energy trauma to the knee (6,9,11).
This condition was first described by Nelaton in 1874. Lyle proposed a classification in 1925, later modified by Ogden in 1974 (5,6) when he proposed four types of PTFJ injuries: type I—subluxation (atraumatic, excessive joint mobility with no dislocation); type II—antero-lateral (85% of all cases, usually during sports); type III—postero-medial [10% of all cases (11), usually related to direct trauma to the knee]; type IV—superior dislocation (rare, usually related with fibular head fractures or high-energy trauma).
Diagnosis is essentially clinical, supported by high suspicion when the mechanism of injury is known. Most common signs and symptoms are acute lateral pain exacerbated by manual pressure over the fibula head, associated with visual asymmetry of the lateral compartment of the knee (5,6,10,12). Peroneal palsy is rare, but transient common peroneal injury is often associated with types II, III and IV. Inferolateral dislocation of the PTFJ is usually associated with popliteal artery transection as the anterior tibial vessels and the anterior peroneal vessels pass through the oval apertures in the superior and distal aspects of the interosseous membrane. Associated tibial or fibular head fractures in patients with polytrauma are rare, but because of its rarity this entity may easily go unnoticed.
Differential diagnoses include meniscal or ligament tear and injury to the postero-lateral structures. Antero-posterior (AP) and lateral view radiographs of both knees are used as first approach, knowing that contralateral comparison is essential to confirm the diagnosis. Radiographs can be normal and computed tomography (CT) scan can be a useful modality to corroborate the clinical findings.
Early diagnosis and treatment are crucial to prevent chronic knee pain and instability (13). It is important to exclude concomitant lesions such as bony, ligamentous and neurological, in the affected knee and ipsilateral ankle to avoid misdiagnosed complications that can compromise good outcomes. Closed reduction is described as the initial approach to the majority of cases (5,6,9) (as Ogden type II is the most common type) (11), taking into account that in postero-medial or superior dislocation cases, open reduction should be the first choice (14).
In this paper, we present two cases of Ogden type II (antero-lateral) isolated PTFJ dislocations, including a successful closed reduction in one of them, and an open reduction internal fixation (ORIF) after the closed reduction failure in a first approach in the other patient.
The authors have obtained the patient’s informed written consent for print and electronic publication of the case report.
Case presentation
Case 1
A 19-year-old male soccer player presented to emergency room after twisting his left knee. When suddenly changing the direction with his left foot fixed to the ground, he felt an acute knee pain being unable to weight bear.
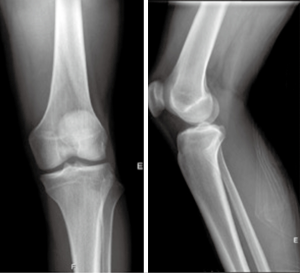
The patient presented with a protruding fibular head (Figure 1) with pain on direct palpation, and was unable to fully extend the injured knee, holding it in a 10-degree flexion position. No signs of joint effusion, meniscus injuries, instability or neurovascular disorders. There was no pain in ipsilateral ankle or hip joint, with full range of motion. Contralateral knee showed no alterations when performing physical examination.
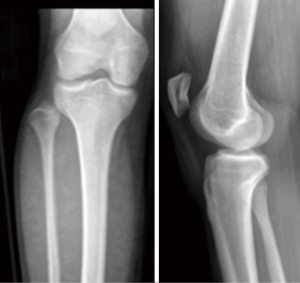
Plain radiographs (AP and lateral) were obtained revealing an isolated antero-lateral PTFJ dislocation (Ogden type II) (Figure 2). CT scan corroborated this diagnosis (Figure 3).
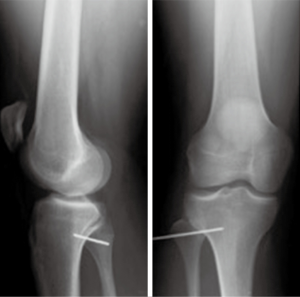
Closed reduction under general anesthesia was performed successfully. With patient under general anesthesia in supine position, the knee was held in a flexion (relaxing femoral biceps tendon, lateral collateral ligaments) and ankle eversion and dorsiflexion were performed (relaxing the anterolateral compartment muscles and interosseous membrane), followed by a direct AP manual pressure over fibular head, until a “pop” was heard. Immediate post-reduction radiographs were obtained to confirm the anatomical reduction (Figure 4) as well as a MRI, excluding concomitant injuries. A Robert-Jones type immobilization was applied and weight bearing was limited for the first 3 weeks with a gradual return to full weight bearing over 6 weeks—no complaints at that time. General rehabilitation program was followed. Return to play with no restrictions was possible after 3 months.
Case 2
A 23-year-old male rugby player presented to emergency room after a right knee injury, whereas trauma mechanism was not exactly known.
Physical examination revealed lateral knee pain and swelling, with visual lateral asymmetry, with no joint effusion, joint instability, peroneal nerve palsy or ankle pain.
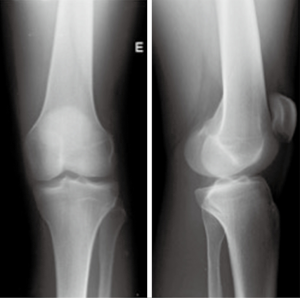
Plain radiographs (AP and lateral) were taken in both knees, revealing antero-lateral isolated dislocation of PTFJ (Ogden type II) (Figure 5). CT scan confirmed the diagnosis as well as absence of concomitant lesions (Figure 6).
Closed reduction under general anesthesia failed therefore ORIF was performed. As previously described in the literature, a lateral approach to the knee was made over the postero-lateral aspect of the knee, doing a neurolysis of the posterior aspect of the fibular head. After open fibular head reduction, PTFJ was transfixed with a K-wire (Figure 7), respecting the postero-lateral structures: popliteus tendon and ligament and fibular collateral ligament, then a Robert-Jones type immobilization was applied. MRI investigation was made the day after this procedure to exclude associated injuries. K-wire was extracted after a 5-week non-weight bearing period. Partial weight bearing with crutches for 2 weeks preceded a general rehabilitation protocol. After a 3-month period, patient was able to return to play with no restrictions.
Discussion
Antero-lateral is the commonest type of PTFJ dislocation accounting for 85% of total cases (2,5,6). The mechanism is an acute twisting with an inverted and plantar flexed ankle (2,5,15) (causing tension in peroneal, extensor hallucis longus and extensor digitorum longus muscles) and a flexed knee (relaxing the fibular collateral ligament and biceps femoris tendon) resulting in antero-lateral dislocation.
Closed reduction is recommended as the first treatment choice for such type II injuries (15). If this first approach fails, ORIF should be performed using a screw or a K-wire to stabilize the PTFJ (16). There is no clear consensus on K-wire versus screw fixation after open reduction.
About post-reduction therapy there is still no consensus in literature (17), suggesting from early rehabilitation exercises to a 6-week immobilization with no weight bearing.
Nieuwe Weme et al. showed, in a literature review, low complication rates independently from therapeutic strategy (17). There is a lack of report in long-term outcomes. The longest follow-up is reported by Aladin et al. with only occasional ache after 108 months (3). It is a commonly misdiagnosed injury and could be a potential cause of chronic knee pain and disability, that can be caused by concomitant injuries that should be excluded by MRI imaging.
In those cases where luxation becomes recurrent, other surgical treatments are available including reconstruction of the PTFJ with a portion of the biceps femoris tendon or iliotibial band, fibular head resection or arthrodesis (9,15,18,19). Even though, the best surgical treatment for this case are not well defined as pain and instability of the lateral compartment of the knee and ankle joint have been reported (5,6,9,15).
We present two different approaches, previously described in literature, for the same PTFJ type of dislocation, both with good results and an early full return to sport, appearing to be reasonable treatment choices in an area where there is yet no consensus.
Conclusions
This case report aims to make clinicians aware of a pathology that can be easily misdiagnosed in an emergency context. Despite its rare incidence rates, maybe undervalued, it can be readily treated, with excellent prognosis.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.01.07). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bozkurt M, Yilmaz E, Akseki D, et al. The evaluation of the proximal tibiofibular joint for patients with lateral knee pain. Knee 2004;11:307-12. [Crossref] [PubMed]
- Resnick D, Newell JD, Guerra J Jr, et al. Proximal tibiofibular joint: anatomic-pathologic-radiographic correlation. AJR Am J Roentgenol 1978;131:133-8. [Crossref] [PubMed]
- Aladin A, Lam KS, Szypryt EP. The importance of early diagnosis in the management of proximal tibiofibular dislocation: a 9- and 5-year follow-up of a bilateral case. Knee 2002;9:233-6. [Crossref] [PubMed]
- Espregueira-Mendes JD, da Silva MV. Anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc 2006;14:241-9. [Crossref] [PubMed]
- Ogden JA. Subluxation of the proximal tibiofibular joint. Clin Orthop Relat Res 1974;192-7. [PubMed]
- Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res 1974;186-91. [PubMed]
- Harvey GP, Woods GW. Anterolateral dislocation of the proximal tibiofibular joint: case report and literature review. Todays OR Nurse 1992;14:23-7. [PubMed]
- Horst PK, LaPrade RF. Anatomic reconstruction of chronic symptomatic anterolateral proximal tibiofibular joint instability. Knee Surg Sports Traumatol Arthrosc 2010;18:1452-5. [Crossref] [PubMed]
- Sekiya JK, Kuhn JE. Instability of the proximal tibiofibular joint. J Am Acad Orthop Surg 2003;11:120-8. [Crossref] [PubMed]
- Thomason PA, Linson MA. Isolated dislocation of the proximal tibiofibular joint. J Trauma 1986;26:192-5. [Crossref] [PubMed]
- Horan J, Quin G. Proximal tibiofibular dislocation. Emerg Med J 2006;23:e33 [Crossref] [PubMed]
- Semonian RH, Denlinger PM, Duggan RJ. Proximal tibiofibular subluxation relationship to lateral knee pain: a review of proximal tibiofibular joint pathologies. J Orthop Sports Phys Ther 1995;21:248-57. [Crossref] [PubMed]
- Marshall JL, Girgis FG, Zelko RR. The biceps femoris tendon and its functional significance. J Bone Joint Surg Am 1972;54:1444-50. [Crossref] [PubMed]
- Van Seymortier P, Ryckaert A, Verdonk P, et al. Traumatic proximal tibiofibular dislocation. Am J Sports Med 2008;36:793-8. [Crossref] [PubMed]
- Falkenberg P, Nygaard H. Isolated anterior dislocation of the proximal tibiofibular joint. J Bone Joint Surg Br 1983;65:310-1. [Crossref] [PubMed]
- Parkes JC 2nd, Zelko RR. Isolated acute dislocation of the proximal tibiofibular joint. Case report. J Bone Joint Surg Am 1973;55:177-83. [Crossref] [PubMed]
- Nieuwe Weme RA, Somford MP, Schepers T. Proximal tibiofibular dislocation: a case report and review of literature. Strategies Trauma Limb Reconstr 2014;9:185-9. [Crossref] [PubMed]
- Cazeneuve JF, Bracq H, Meeseman M. Weinert and Giachino ligament arthroplasty for the surgical treatment of chronic superior tibiofibular joint instability. Knee Surg Sports Traumatol Arthrosc 1997;5:36-7. [Crossref] [PubMed]
- Weinert CR Jr, Raczka R. Recurrent dislocation of the superior tibiofibular joint. Surgical stabilization by ligament reconstruction. J Bone Joint Surg Am 1986;68:126-8. [Crossref] [PubMed]
Cite this article as: Nunes J, Direito-Santos B, Costa A, Tavares N, Varanda P, Duarte R. Acute proximal tibiofibular joint dislocation: a sports related injury?—two different cases. Ann Joint 2019;4:11.