
Anatomical rectangular tunnel ACL reconstruction with a bone-patellar tendon-bone graft: its concept, indication and efficacy
Concept
For achieving the goal of ACL reconstruction (ACLR) to restore stability of the knee without loss of motion, we believe that the implanted graft should closely resemble the native ACL in macroscopic morphology, orientation, alignment of internal fibers and tension. Thus, it is mandatory to select a suitable graft, to create the tunnel apertures inside the native ACL attachment areas, to place it properly, and to fix it under adequate tension.
A bone-patellar tendon-bone (BTB) autograft is one of the most suitable tissues for ACLR (1), while the graft of 10-mm width has been widely used via 10-mm round tunnels to reconstruct a single bundle (SB). In this SB ACLR procedure with the graft, the following issues had been concerned: (I) the graft could not mimic the internal fiber arrangement of the native ACL; (II) there is futile space between the trapezoid/triangular pillar bone plugs and the round/cylindrical tunnels; (III) there is unfavorable space between the proximal portion of the round tibial tunnel and tendinous portion of the graft of rectangular cross section.
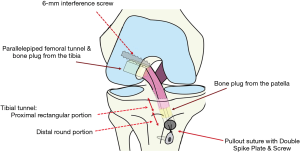
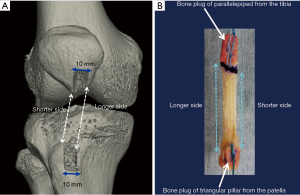
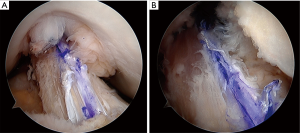
In order to resolve these issues, the anatomical rectangular tunnel (ART) ACLR with a single BTB graft was developed (Figures 1,2), as we found it possible to arrange the graft to mimic not only the orientation of the native ACL but its internal fiber arrangement (2). In this procedure (3,4), the BTB graft with rectangular cross section could fairly resemble the normal ACL in internal fiber arrangement (4), as well as contact with tunnel wall without little futile space. In other words, this technique could realize the concept of double bundle ACLR with a single BTB graft. Biomechanically, ART ACLR has been proven superior to the conventional trans-tibial SB ACLR based on the isometric grafting concept (5).
Indications for BTB grafting
One of the advantages for ART ACLR with a BTB graft is earlier integration of bone plug to bone tunnel wall (6), while the graft harvest site morbidity is relatively high in autografting. Therefore, the autogenous BTB graft may be indicated for young athletes with high motivation for returning strenuous/contact sports including football or judo. On the contrary, this graft may not be suitable for aged patients with weaker bone plug due to osteoporosis or less active female patients with higher risk of arthrofibrosis.
Operative procedure
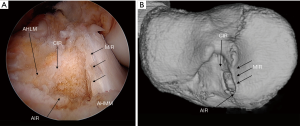
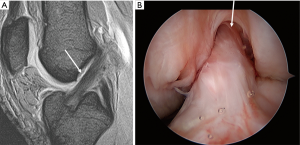
A BTB autograft of 10 to 13 mm width is harvested from the central portion of the medial half of the patellar tendon. A rectangular parallelepiped femoral tunnel in accordance with the rectangular cross section of the graft is created inside the femoral attachment area (Figure 3) (7,8). The tibial tunnel of proximal rectangular parallelepiped and of distal round cylinder is made inside the tibial attachment area (Figure 4) (9-11). The graft is passed through the tibial tunnel to the femoral one. Femoral fixation is achieved with 6 to 7 mm interference screw or pull out sutures to the femoral cortex. Then tibial fixation is performed as the following special pull out suture technique: (I) the sutures tied to the bone plug are connected to the top hole of Double Spike Plate® (DSP, Meira, Nagoya, Japan); (II) the tensioning suture passed through the bottom hole of DSP is connected to a tensioner mounted to the tensioning boot fixed to the tibia with a bandage; (III) the graft is in situ pretensioned by repetitive strong manual pulls of 10 times; (IV) an initial tension of 10–20N is applied to the graft at 20 degree of flexion; (V) the final graft fixation is achieved with the DSP and a screw installed.
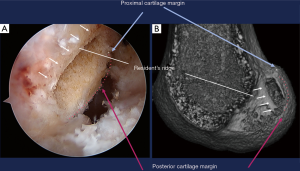
In this procedure the notchplasty is not required to avoid the graft impingement to the notch in extension (Figure 5).
Postoperative rehabilitation
After brace immobilization for one week, ROM exercise is begun. Partial weight bearing is allowed at two weeks, followed by full weight bearing at four weeks. Jogging is recommended at three months, followed by return to sports activities at 7–9 months.
Efficacy
Our 2-year follow-up study has just been published (12). We prospectively enrolled 71 patients in this study from the total number of 242 patients undergoing the ART ACLR for primary unilateral ACL injury from January 2009 to June 2014. The inclusion criteria were as follows: (I) contra-lateral healthy knee; (II) no radiological osteoarthritic change; (III) consent of undergoing postoperative CT scans and outpatient follow-up evaluation at 2 years. During the postoperative follow-up term, 10 patients were excluded due to secondary ACL injury: 6 patients, graft rupture; 4 patients, contralateral ACL injury. Then 61 patients were finally included. They were 40 males and 21 females with a mean age of 22.7±8.0 [14–48] years at the time of ACLR. None of the patients sustained secondary meniscal injuries. The International Knee Documentation Committee (IKDC) subjective assessment showed that all the 61 patients who had not sustained traumatic graft rupture were classified as ‘normal’ or ‘nearly normal’. The Lachman and pivot-shift test were negative in 98.4% and 95.1% of them, respectively. The mean side-to-side difference of the anterior laxity at the maximum manual force with KT-1000 Knee Arthrometer was 0.2±0.9 mm, with 95.1% of patients ranging from −1 to +2 mm (Figure 6) (12). Furthermore, tunnel expansion following the current procedure is much less than that after the reconstruction using hamstring tendons (13).
Discussion
There is a concern on higher graft rupture rate following the anatomical ACLRs including ART procedure compared to that after non-anatomical ACLRs which had been frequently performed in the last century (14). One of the reasons for the higher graft rupture rate could be full return to pre-injury strenuous sports without fear of instability. However, it should be noted that subsequent meniscal tears after the anatomical ACLRs are much fewer compared to those following the non-anatomical ACLRs. This suggests that the anatomical ACLRs are more effective to stabilize the knee or to preserve the menisci.
Improved rehabilitation, proprioceptive training and adequate education may be required to prevent secondary ACL injury.
Conclusions
ART ACLR with a single BTB graft is an effective procedure to stabilize the knee without loss of motion by closely mimicking the native ACL. No lateral extra-articular tenodesis is required.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Takeshi Muneta) for the series “Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.01.04). The series “Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy” was commissioned by the editorial office without any funding or sponsorship. KS received funding from Smith & Nephew Inc., MA, USA. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Noyes FR, Butler DL, Grood ES, et al. Biomechanical Analysis of Human Ligament Grafts used in Knee-Ligament Repairs and Reconstructions. J Bone Joint Surg 1984;66:344-52. [Crossref] [PubMed]
- Friedrich NF, O’Brien WR. Functional anatomy of the cruciate ligaments. In: Jakob RP, Staeubli HU. editors. The Knee and the Cruciate Ligaments. Berlin: Springer-Verlag, 1992:78-91.
- Shino K, Nakata K, Nakamura N, et al. Anatomically oriented anterior cruciate ligament reconstruction with a bone-patellar tendon-bone graft via rectangular socket and tunnel: a snug-fit and impingement-free grafting technique. Arthroscopy 2005;21:1402. [Crossref] [PubMed]
- Shino K, Nakata K, Horibe S, et al. Rectangular tunnel double-bundle anterior cruciate ligament reconstruction with bone–patellar tendon–bone graft to mimic natural fiber arrangement. Arthroscopy 2008;24:1178-83. [Crossref] [PubMed]
- Suzuki T, Shino K, Otsubo H. at al. Biomechanical comparison between the rectangular-tunnel and the round-tunnel anterior cruciate ligament reconstruction procedures with a bone-patellar tendon-bone graft. Arthroscopy 2014;30:1294-302. [Crossref] [PubMed]
- Suzuki T, Shino K, Nakamura N, et al. Early integration of a bone plug in the femoral tunnel in rectangular tunnel ACL reconstruction with a bone-patellar tendon-bone graft: a prospective computed tomography analysis. Knee Surg Sports Traumatol Arthrosc 2011;19:S29-S35. [Crossref] [PubMed]
- Iwahashi T, Shino K, Nakata K, et al. Direct ACL insertion to the femur assessed by histology and three-dimensional volume-rendered computed tomography. Arthroscopy 2010;26:S13-S20. [Crossref] [PubMed]
- Shino K, Suzuki T, Iwahashi T, et al. The resident’s ridge as an arthroscopic landmark for anatomical femoral tunnel drilling in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2010;18:1164-8. [Crossref] [PubMed]
- Siebold R, Schumacher P, Fernandez F, et al. Flat midsubstance of the anterior cruciate ligament with tibial “C”-shaped insertion site. Knee Surg Sports Traumatol Arthrosc 2015;23:3136-42. [Crossref] [PubMed]
- Tensho K, Shimodaira H, Aoki T, et al. Bony Landmarks of the Anterior Cruciate Ligament Tibial Footprint: A Detailed Analysis Comparing 3-Dimensional Computed Tomography Images to Visual and Histological Evaluations. Am J Sports Med 2014;42:1433-40. [Crossref] [PubMed]
- Kusano M, Yonetani Y, Mae T, et al. Tibial insertions of the anterior cruciate ligament and the anterior horn of the lateral meniscus: A histological and computed tomographic study. The Knee 2017;24:782-91. [Crossref] [PubMed]
- Tachibana Y, Shino K, Mae T, et al. Anatomical rectangular tunnels identified with the arthroscopic landmarks result in excellent outcomes in ACL reconstruction with a BTB graft. Knee Surg Sports Traumatol Arthrosc 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Tachibana Y, Mae T, Shino K, et al. Femoral tunnel enlargement after anatomic anterior cruciate ligament reconstruction: Bone-patellar tendon-bone/single rectangular tunnel versus hamstring tendon/double tunnels. J Orthop Sci 2018;23:1011-8. [Crossref] [PubMed]
- Mae T, Shino K, Matsumoto N, et al. Risk factors for ipsi-lateral graft rupture or contralateral anterior cruciate ligament tear after anatomic double-bundle reconstruction. Asia-Pacific Journal of Sports Medicine 2014;1:90-5.
Cite this article as: Shino K, Mae T, Uchida R, Yokoi H, Ohori T, Tachibana Y. Anatomical rectangular tunnel ACL reconstruction with a bone-patellar tendon-bone graft: its concept, indication and efficacy. Ann Joint 2019;4:12.


