
Pelvic reconstruction after partial acetabular resection of bone sarcoma
Introduction
Pelvic bone tumour surgery is challenging. Tumour surgeons have to achieve a negative resection margin for the best oncological outcomes with the reduced risk of local recurrence and improved patient survival (1-4). Tumour surgeons perform tumour resections that base on the preoperative assessment of the radiological images and intraoperative execution of the mental surgical planning.
Given that the pelvic bone has a complex geometry with intricately related vital neurovascular structures, surgeons may resect tumours with more margin than oncologically necessary when taking into account the inaccuracy in planning and resection. The lesser normal bone may be retained for reconstruction to restore limbs function. Therefore, bone sarcoma locating near the acetabulum is often resected including the entire acetabulum, PII resection according to Enneking and Dunham Classification (5). Various types of reconstruction have been reported to restore the acetabular defect with pelvic discontinuity after PII resections. They include hip transposition, allografts, endoprostheses. The surgeries are associated with a high rate of complications such as nonunion, infection and hardware failure (6-12) due to the extensive bone being resected at the weight-bearing hip joint without ideal reconstructive methods. It leads to a fair limb function. In one study, the mean functional score by Musculoskeletal Tumor Society (MSTS) after the surgeries was reported to be 14.5 out of 30 (13).
Partial acetabular resection of bone sarcoma with pelvic reconstruction has been described in selected patients with periacetabular tumours in a few case series (14-18). Early promising results were reported with the advantages of preserving more host bone for reconstruction without compromising the oncological resection margin and increasing the risk of local recurrence when the surgeries were performed with good preoperative planning and guided resection under computer navigation guidance. This article is to review the pelvic reconstruction after partial acetabular resection of bone sarcoma, its pathoanatomy, surgical considerations, current evidence and limitations.
Pathoanatomy of the acetabulum bone tumours
The pelvis forms a ring structure, consisting of the two innominate bones, the sacrum and coccyx (19,20). The innominate bones are formed by the fusion of the ilium, ischium and pubis. The lateral surface of each innominate bone lies the acetabulum with the ilium contributing to its superior part, the ischium to its posterior part and the pubis to its anterior part. The central non-articular depression, the cotyloid fossa, divides the acetabulum into the anterior and posterior column.
The hip joint is a ball and socket joint, articulating the femoral head and the acetabulum. The fibrocartilaginous labrum lining at the rims of the acetabulum further deepens the socket for hip stability. Capsular ligaments around the hip joint provide additional stability. Iliofemoral and pubofemoral ligaments contribute to anterior hip stability. Ischiofemoral ligament reinforces the hip posterior stability. Ligamentum teres gives the internal stability to hip joint as it connects the femoral head at the fovea centralis to the acetabulum at the transverse acetabular ligament.
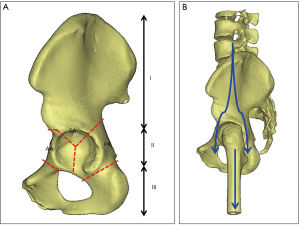
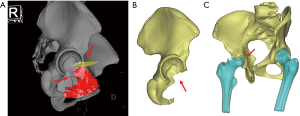
To date, there is no classification to describe the bone sarcoma partially involving the acetabulum. Anatomically, a tumour can affect the whole acetabulum (IIA). It can arise solely from the anterior column of the acetabulum (IIAA) or the posterior column of the acetabulum (IIPA). It can also be an extension of an ischial tumour to the posterior column (III + IIPA), superior pubic ramus tumour to the anterior column (III+ IIAA) or an iliac tumour to the superior dome of the acetabulum (I + IISA) (Figure 1A). Pelvic resection was classified into three main types by Enneking and Dunham (21). Type I (PI) is the resection confined to the ilium. Type II (PII) is the resection confined to the periacetabulum. Type III (PIII) is the resection confined to the pubis. Partial acetabular resection of the tumours is theoretically possible if negative resection margin can be achieved. The retained acetabular bone after resection not only can partially maintain the pelvic continuity for load transfer from spine to lower extremities but also provide the additional bone strut to restore the acetabular integrity for hip motion (Figure 1B).The acetabular bone defect or nearby hip ligaments may also require reconstruction to maintain hip stability after tumour resection.
Surgical considerations of a partial acetabular resection
The surgical goal is to resect bone tumours with complete tumour removal while sparing the host bone for functional reconstruction. In selected groups of patients with acetabular bone tumours, partial acetabular resections with negative margins, instead of segmental resection of the entire acetabulum, may be considered as a treatment option.
Based on the limited available literature (14-18) (Table 1), several factors are considered if contemplating a partial acetabular resection of periacetabular bone tumours. They are (I) types of bone tumours, (II) resections with limited wide margins, (III) surgical planning and assistive tools with guided resection, and (IV) the types of bone reconstruction after tumour resection.
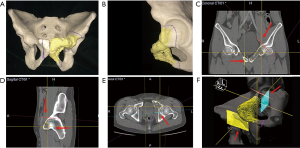
Full table
Type of bone tumours
The bone tumours indicated for the technique may include low-grade chondrosarcoma (14,15,17), high-grade bone sarcoma responding to neoadjuvant chemotherapy (16) or benign but locally aggressive giant cell tumour of bone (18). Low-grade sarcoma has less aggressive tumour biology. Some authors reported limited resection with negative margins by performing hemicortical resections in low-grade surface bone sarcoma (22,23). The resection retained a part of the host cortical circumference to enhance bone healing that may restore better function. High-grade sarcoma may be modulated and marginalized by the neoadjuvant chemotherapy. With the advent of effective chemotherapy, a joint-preserving tumour resection with a close but negative margin was possible in selected patients with high-grade osteosarcoma involving metaphysis around the knee joints (24-26). The similar joint-preserving approach may be considered in selected patients with high-grade bone sarcoma involving part of the acetabulum. In a study of surgical management of pelvic Ewing’s sarcoma in paediatric patients, open triradiate cartilage without tumour invasion allowed partial acetabular resection (16). In giant cell tumours involving the pelvis, wide resection has been reported to have a lower risk of local recurrence than intralesional curettage (27,28). Given the benign nature of the giant cell tumour of bone, it is beneficial to maximize the hip function by preserving host bone as much as possible for reconstruction after wide resection.
Resections with limited wide margins
The smallest safe distance from the tumor in bone sarcoma resection is controversial. The best size of surgical margin may depend on the factors like tumour grade, histology type and response to neoadjuvant chemotherapy (29-32). Among 885 osteosarcoma patients undergoing neoadjuvant chemotherapy and limb-sparing surgeries, no difference in local tumour recurrence was reported for different surgical margin (33). In a cohort of 389 high-grade osteosarcoma patients with neoadjuvant chemotherapy and tumour resection, surgical margin >2 mm and more than 90% chemonecrosis showed less local recurrence and better overall survival than those with margin <2 mm and less than 90% chemonecrosis (34). Another study of 186 high-grade osteosarcomas also concurred that a margin distance of >2 mm significantly decreased the risk of local tumour recurrence (35). The studies might indicate that in selected osteosarcoma patients who respond to neoadjuvant chemotherapy, local tumour control may not be compromised provided that a negative margin is ensured even if the margin is comparatively narrow. The results contradict the traditional thinking of the necessity of a minimum of 3cm bone margin for local tumour control (36).
A resection with a limited wide margin in bone sarcoma surgery was first described in 2010 (37). The technique was to treat selected patients with high-grade bone sarcomas with the goal of minimizing bone and soft tissue removal. The authors arbitrarily used 1cm as the minimum required margin. In order to achieve limited wide margins, multiplanar osteotomy by using angled bone cuts was described to completely resect bone tumours while sparing host tissue. In a retrospective study of six patients with high-grade bone sarcoma involving the long bones, there was no local tumour recurrence and all allograft healed at an average follow-up of 39 months. The study concluded that in carefully selected patients, the technique might be considered an option for treating high-grade bone sarcoma when compared with traditional techniques by segmental resection. It may allow improved healing and function of the operated limbs without compromising oncological control (37). In case reports or small cohorts (14-18), other authors reported using uniplanar or biplanar osteotomies in the partial acetabular resection of pelvic bone tumours. Negative resection margin could be achieved in all patients while preserving a part of the acetabulum, in particular, its superior portion that is important for weight-bearing function. Multiplanar osteotomies around the tumour edge could preserve more host bone than uniplanar osteotomies (15,17). In carefully selected patients, the technique may be oncologically safe as there was no local recurrence noted at the short-term follow-up in the published reports.
Surgical planning and assistive tools with guided resection
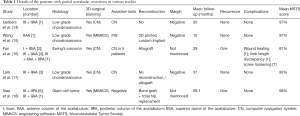
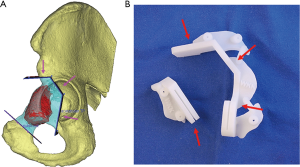
It is technically challenging in partial acetabular bone tumour resections given the complexity of pelvic bone anatomy. Also, the intraosseous tumour extent and resection margin are difficult to determine accurately even with the help of intraoperative fluoroscopy. A detailed 3D surgical planning has been advocated if contemplating a partial acetabular tumour resection (14,15,17,18). The 3D planning was carried out with either computer navigation software (14,17) (Figure 2A,B,C,D,E,F) or engineering software (MIMICS, Materialise, Leuven, Belgium) (15,18) (Figure 3A). The Digital Imaging and Communications in Medicine (DICOM) files of patient’s CT and/or MR images were imported into the software. The extent of the tumour was mapped. A virtual 3D model of pelvic bone and tumour could be created. The optimal resection planes could thus be defined in the software, based on all the reformatted 2D images and the 3D bone-tumour model (Figure 2C,D,E,F). In order to translate the surgical planning to the patient at the operating theatre, the partial acetabular resection was performed and guided with assistive tools, either by the intraoperative guidance of computer navigation (14,16,17) or 3D printed patient-specific instrument (15). Under the real-time tracking of the pelvic bone with reference to the preoperative CT/MR images, the computer navigation allowed visualizing the intraosseous tumour extent and identifying the planned sites of bone resection. The 3D printed patient-specific instrument had cutting platforms that could confine the orientation of the cutting saw blade along the planned resection planes (Figure 3B). The 3D preoperative planning and intraoperative assistive tools are essential to replicate the planned multiplanar osteotomies at the acetabulum, so to allow partial acetabular resection while sparing part of the acetabulum.
The types of bone reconstruction after tumour resection
The aim of the bone reconstruction after partial acetabular resection is to restore acetabular integrity and achieve a stable hip joint movement. It can range from no reconstruction, biological to prosthetic reconstruction. To date, the amount of the acetabular bone defect after partial acetabular resection that begins to affect hip stability is not known. Only cadaveric studies were reported to investigate the stability of the hip joint after simulated acetabular fractures (38,39). One of these studies suggested that the hip was stable if the weight-bearing part of the acetabulum had the roof-arc angle (medial, anterior and posterior) of 45, 25 or 70 degrees or less in the corresponding AP views, obturator oblique view, and iliac oblique views of the radiograph (39). However, the reference results may not be applicable to acetabular tumour resection as an acetabular bone defect after resection of the tumour and its nearby soft tissue may lead to more unstable hip than after acetabular fracture. Also, the radiographs for assessing roof-arc angles may be difficult to acquire intraoperatively because patients usually lie in a lateral position on the operative table.
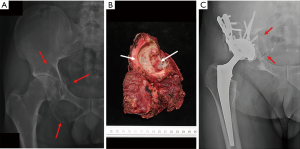
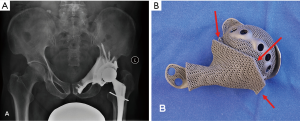
There is no reported method to determine hip stability after partial acetabular tumour resection. It is then practical to intraoperatively test the hip stability after the resection by manual hip movement. In general, the partial acetabular tumour resection that includes the whole acetabular column requires some form of reconstruction to restore stable hip movement. If only a portion of the acetabular column is resected and ligamentum teres can be spared, no reconstruction is needed (14,17) if the hip is stable at the intraoperative manual hip testing (Figure 4A,B,C). Therefore, ischial tumours affecting the inferior part of the posterior acetabular columns or superior pubic ramus tumours affecting the inferior part of the anterior acetabular columns may require no reconstruction if undergoing partial acetabular resections. If bone reconstruction is necessary to restore stable hip movement after the resection, biological or prosthetic reconstruction has been described in the small cohorts or a case report (15,16,18). Studies have reported using allograft to restore the acetabular defect after partial acetabular tumour resection (16,17). The allograft was trimmed and fixed to the remaining pelvis by plates and screws. It prevented hip dislocation and allowed stable hip movement. In a cohort of seven patients with pelvic giant cell tumour undergoing a partial acetabular resection (18), the ipsilateral femoral head and neck were used to reconstruct the acetabular defect. The autogenous bone graft was fixed to the remaining acetabulum with screws. The femoral head was then trimmed and reamed to match to the remaining acetabular socket into which an acetabular cup was impacted. A femoral stem was placed in the usual way of a total hip arthroplasty (Figure 5A,B,C). The surgical planning was simulated in the engineering software, MIMICS before contemplating in the actual patient. At a mean follow-up of 38.1 months, all bone graft healed and neither acetabular failure nor hip dislocation was noted. The mean functional MSTS score was excellent with 29.4 out of 30. The acetabular bone defect could also be reconstructed with a custom-made implant after partial acetabular tumour resection (15). A paper reported a 65-year-old patient had low grade chondrosarcoma involving the anterior acetabular column. He underwent a multiplanar, partial acetabular tumour resection with the assistance of a 3D-printed patient-specific instrument that guided the planned resection planes. The geometric bone defect was then reconstructed with a 3D-printed pelvic implant that was secured to the remaining pelvic bone by multiple screws (Figure 6A,B). The patient had excellent hip function without implant loosening at the latest follow-up. One limitation of the method was that the implant was not readily available for tumour surgery. The lead time may take about two months for the design and manufacture of the custom-made implant. Therefore, only slow-growing tumours or tumours responding to neoadjuvant chemotherapy may adopt the technique.
The early results of the partial acetabular tumour resection were reported to be safe as no major complications and local recurrence were noted (14-18). As part of the normal acetabulum can be preserved, the limb function was good with reported MSTS score ranging from 24 to 30 (14-18). Although the early results were promising, there are limitations. First, the published data are only non-comparative cohorts studying a small number of patients with different histological types. Second, the duration of follow-up in the studies was short. Loco-regional relapse or distant metastases may happen with longer follow-up. Third, not every periacetabular tumour is suitable for the partial acetabular resection. It may benefit only less than half of the patients with periacetabular tumours under careful selection criterion (17,18). Fourth, the method may need accurate 3D surgical planning or assistive tools (like computer navigation or 3D printed patient-specific instruments) to achieve the multiplanar, limited-wide resection with a negative margin. Not every unit has the facilities and expertise to implement the technically demanding surgical technique. However, with the advent of a more user-friendly platform for 3D surgical planning and guided resection with assistive tools, more tumour surgeons are able to use the technology. Fifth, there is no anatomical study to determine the size of the acetabular defect that the hip begins to become unstable. The best reconstructive method for the partial acetabular defect is also unknown, and no long-term data is available for the fate of the partially retained acetabulum with regards to the functional results. Studies with more patients and longer follow-up are still required to confirm the long-term oncological safety and superior function limb function when compared with the traditional complete PII acetabular resection.
Conclusions
In carefully selected patients with periacetabular tumours, a part of normal acetabulum may be spared after a partial acetabular resection with limited-wide margin. The 3D surgical planning and guided resection with assistive tools like computer navigation or 3D-printed patient-specific instruments facilitate the resection and help replicate the surgical planning. The bone-preserving surgery of the hip joint may offer the potential advantages of superior limb function without compromising the oncological clearance. Biological or prosthetic options were used to reconstruct the partial acetabular defects with early good results of limb function. However, as concrete evidence of superior results is lacking when compared with complete PII acetabular resection, long-term studies with more patients are needed to confirm the oncological safety and potential superior limb function in partial acetabular tumour resection and reconstruction.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Wei Guo, Tao Ji, Paul Jutte and Eric Henderson) for the series “Reconstruction in Orthopaedic Oncology - Frontier and Future Trends” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.04.02). The series “Reconstruction in Orthopaedic Oncology - Frontier and Future Trends” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kawai A, Healey JH, Boland PJ, et al. Prognostic factors for patients with sarcomas of the pelvic bones. Cancer 1998;82:851-9. [Crossref] [PubMed]
- Pring ME, Weber KL, Unni KK, et al. Chondrosarcoma of the pelvis. A review of sixty-four cases. J Bone Joint Surg Am 2001;83-A:1630-42. [Crossref] [PubMed]
- Han I, Lee YM, Cho HS, et al. Outcome after surgical treatment of pelvic sarcomas. Clin Orthop Surg 2010;2:160-6. [Crossref] [PubMed]
- Sherman CE, O'Connor MI, Sim FH. Survival, local recurrence, and function after pelvic limb salvage at 23 to 38 years of followup. Clin Orthop Relat Res 2012;470:712-27. [Crossref] [PubMed]
- Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am 1978;60:731-46. [Crossref] [PubMed]
- Gebert C, Gosheger G, Winkelmann W. Hip transposition as a universal surgical procedure for periacetabular tumors of the pelvis. J Surg Oncol 2009;99:169-72. [Crossref] [PubMed]
- Bell RS, Davis AM, Wunder JS, et al. Allograft reconstruction of the acetabulum after resection of Stage IIB sarcoma: intermediate term result. J Bone Joint Surg Am 1997;79:1663-74. [Crossref] [PubMed]
- Hillmann A, Hoffmann C, Gosheger G, et al. Tumors of the pelvis: complications after reconstruction. Arch Orthop Trauma Surg 2003;123:340-4. [Crossref] [PubMed]
- Aljassir F, Beadel GP, Turcotte RE, et al. Outcome after pelvic sarcoma resection reconstructed with saddle prosthesis. Clin Orthop Relat Res 2005;36-41. [Crossref] [PubMed]
- Guo W, Li D, Tang X, et al. Reconstruction with modular hemipelvic prostheses for periacetabular tumor. Clin Orthop Relat Res 2007;180-8. [PubMed]
- Brown TS, Salib CG, Rose PS, et al. Reconstruction of the hip after resection of periacetabular oncological lesions: a systematic review. Bone Joint J 2018;100-B:22-30. [Crossref] [PubMed]
- Ogura K, Susa M, Morioka H, et al. Reconstruction using a constrained-type hip tumor prosthesis after resection of malignant periacetabular tumors: A study by the Japanese Musculoskeletal Oncology Group (JMOG). J Surg Oncol 2018;117:1455-63. [Crossref] [PubMed]
- Hoffmann C, Gosheger G, Gegert C, et al. Functional results and quality of life after treatment of pelvic sarcomas involving the acetabulum. J Bone Joint Surg Am 2006;88:575-82. [PubMed]
- Gerbers JG, Jutte PC. Hip-sparing approach using computer navigation in periacetabular chondrosarcoma. Comput Aided Surg 2013;18:27-32. [Crossref] [PubMed]
- Wong KC, Kumta SM, Geel NV, et al. One-step reconstruction with a 3D-printed, biomechanically evaluated custom implant after complex pelvic tumor resection. Comput Aided Surg 2015;20:14-23. [Crossref] [PubMed]
- Fan H, Guo Z, Fu J, et al. Surgical management of pelvic Ewing's sarcoma in children and adolescents. Oncol Lett 2017;14:3917-26. [Crossref] [PubMed]
- Lam YL, Yau R, Ho KW, et al. Is it possible and safe to perform acetabular-preserving resections for malignant neoplasms of the periacetabular region? Clin Orthop Relat Res 2017;475:656-65. [Crossref] [PubMed]
- Xiao C, Zhou Y, Zhang W, et al. An acetabular-preserving procedure for pelvic giant cell tumor involving partial acetabulum. World J Surg Oncol 2017;15:200. [Crossref] [PubMed]
- Lawrence DA, Menn K, Baumgaertner M, et al. Acetabular fractures: anatomic and clinical considerations. AJR Am J Roentgenol 2013;201:W425-36 [Crossref] [PubMed]
- Scheinfeld MH, Dym AA, Spektor M, et al. Acetabular fractures: what radiologists should know and how 3D CT can aid classification. Radiographics 2015;35:555-77. [Crossref] [PubMed]
- Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am 1978;60:731-46. [Crossref] [PubMed]
- Agarwal M, Puri A, Anchan C, et al. Hemicortical excision for low-grade selected surface sarcomas of bone. Clin Orthop Relat Res 2007;161-6. [Crossref] [PubMed]
- Deijkers RL, Bloem RM, Hogendoorn PC, et al. Hemicortical allograft reconstruction after resection of low-grade malignant bone tumours. J Bone Joint Surg Br 2002;84:1009-14. [Crossref] [PubMed]
- Muscolo DL, Ayerza MA, Aponte-Tinao LA, et al. Partial epiphyseal preservation and intercalary allograft reconstruction in high-grade metaphyseal osteosarcoma of the knee. J Bone Joint Surg Am 2005;87:226-36. [Crossref] [PubMed]
- Agarwal M, Puri A, Gulia A, et al. Joint-sparing or physeal sparing diaphyseal resections: the challenge of holding small fragments. Clin Orthop Relat Res 2010;468:2924-32. [Crossref] [PubMed]
- Wong KC, Kumta SM. Joint-preserving tumor resection and reconstruction using image-guided computer navigation. Clin Orthop Relat Res 2013;471:762-73. [Crossref] [PubMed]
- Guo W, Sun X, Zang J, et al. Intralesional excision versus wide resection for giant cell tumor involving the acetabulum: which is better? Clin Orthop Relat Res 2012;470:1213-20. [Crossref] [PubMed]
- Zheng K, Wang Z, Wu SJ, et al. Giant cell tumor of the pelvis: a systematic review. Orthop Surg 2015;7:102-7. [Crossref] [PubMed]
- Picci P, Sangiorgi L, Rougraff BT, et al. Relationship of chemotherapy-induced necrosis and surgical margins to local recurrence in osteosarcoma. J Clin Oncol 1994;12:2699-705. [Crossref] [PubMed]
- Bielack SS, Kempf-Bielack B, Winkler K. Osteosarcoma: relationship of response to preoperative chemotherapy and type of surgery to local recurrence. J Clin Oncol 1996;14:683-4. [Crossref] [PubMed]
- Bielack SS, Kempf-Bielack B, Delling G, et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol 2002;20:776-90. [Crossref] [PubMed]
- Bacci G, Longhi A, Briccoli A, et al. The role of surgical margins in treatment of Ewing’s sarcoma family tumors: experience of a single institution with 512 patients treated with adjuvant and neoadjuvant chemotherapy. Int J Radiat Oncol Biol Phys 2006;65:766-72. [Crossref] [PubMed]
- Andreou D, Bielack SS, Carrle D, et al. The influence of tumor- and treatment-related factors on the development of local recurrence in osteosarcoma after adequate surgery. An analysis of 1355 patients treated on neoadjuvant Cooperative Osteosarcoma Study Group protocols. Ann Oncol 2011;22:1228-35. [Crossref] [PubMed]
- Jeys LM, Thorne CJ, Parry M, et al. A Novel System for the Surgical Staging of Primary High-grade Osteosarcoma: The Birmingham Classification. Clin Orthop Relat Res 2017;475:842-50. [Crossref] [PubMed]
- Cates JM. Reporting Surgical Resection Margin Status for Osteosarcoma: Comparison of the AJCC, MSTS, and Margin Distance Methods. Am J Surg Pathol 2017;41:633-642. [Crossref] [PubMed]
- Gitelis S, Malawer M, MacDonald D, et al. Principles of limb salvage surgery. In: Chapman MW. Editor. Chapman’s Orthopaedic Surgery, 3rd edition. Philadelphia, PA: Lippincott Williams and Wilkins 2001:3309-81.
- Avedian RS, Haydon RC, Peabody TD. Multiplanar osteotomy with limited wide margins: a tissue preserving surgical technique for high-grade bone sarcomas. Clin Orthop Relat Res 2010;468:2754-64. [Crossref] [PubMed]
- Thomas KA, Vrahas MS, Noble JW Jr, et al. Evaluation of hip stability after simulated transverse acetabular fractures. Clin Orthop Relat Res 1997;244-56. [Crossref] [PubMed]
- Vrahas MS, Widding KK, Thomas KA. The effects of simulated transverse, anterior column, and posterior column fractures of the acetabulum on the stability of the hip joint. J Bone Joint Surg Am 1999;81:966-74. [Crossref] [PubMed]
Cite this article as: Wong KC, Niu X, Xu H, Li Y, Kumta SM. Pelvic reconstruction after partial acetabular resection of bone sarcoma. Ann Joint 2019;4:23.


