
Does metal allergy have relevance in patients undergoing arthroplasty—an electronic survey of surgeon attitudes
Introduction
Metallic implants are an integral part of the practice of orthopaedic surgery. Metal hypersensitivity (on patch testing) is reported to be from 10−17% of the general population (1-6). However, higher rates of hypersensitivity described in literature on body piercing suggests that the rates might be higher than previously imagined and have potential demographically related risk factors. For example, two recent studies looking into metal hypersensitivity as it relates to body piercing showed geographic variations in hypersensitivity rates in the general population. These studies demonstrated that hypersensitivity was also related to body piercings with rates increasing with increased number of piercings (7,8). In the Schuttelaar et al. study (European), a history of piercings was associated with a 20.8% incidence of nickel allergy. Having three or more piercings increase the incidence to 27.6%, with females age 31−45 having the highest incidence (31.8%) (7). Similarly, Warshaw et al. (North America) showed that having five or more piercing increased the incidence to 34% (8).
No consensus or standard exists on how to screen or what changes in treatment plans need to be implemented when there is reported a sensitivity to metals or jewelry (2-4,6,9-13). Recent studies examined the role of metal sensitivities in painful hip (9,14-19) and knee arthroplasties (18,20-22). Based on these studies, the role of metal sensitivity in persistently painful or aseptic loosening of lower extremity arthroplasties was found to be uncertain, the evidence inconclusive. Numerous literature reviews and meta-analyses regarding metal hypersensitivity and allergy to orthopaedic implants have been published, with large variance on incidence (1,3-5,10-13,23-25) and existence of metal hypersensitivity (10,26-30). These reviews suggest that preoperative testing, with methods such as metal allergy patch testing, serum metal ion testing, lymphocyte transformation testing, or leukocyte migration testing may influence surgical practice (9). However, it is not understood whether these studies correlate with metal hypersensitivity in the context of metal implants.
The lack of compelling data correlating metal hypersensitivities to metal implants has created controversy in the field of orthopaedic surgery about the relevance of metal hypersensitivity. There is currently only one study to date to have surveyed orthopaedic experts in arthroplasty. The Delphi Consensus Study, in the UK (6). This study unfortunately had only a 19% (17/90) response rate and was limited in the scope of its questioning, with consensus being made by just ten responses, reducing its relevance to “expert opinion” rather than true consensus. By contrast, the goal of this study is to gain insight into the experience of orthopaedic surgeons, as it relates to metal allergies to metallic orthopaedic implants. This study also aims to examine the trends in screening and evaluation of patients who have metal hypersensitivity and to understand if this data influences treatment.
Methods
The online survey consisted of 35 questions. The survey questions were aimed at determining orthopaedic surgeons’ experiences and opinions on the prevalence, screening protocols, and treatment adjustments being made when metal hypersensitivity is suspected. E-mail requests were sent to specialty orthopaedic societies and the author’s state orthopedic societies and other orthopedic groups. Several of the orthopaedic specialty societies declined distribution of the survey for a variety of reasons including internal policies preventing the solicitation of their membership. The American Shoulder and Elbow Surgeons (ASES), Orthopaedic Trauma Association (OTA), California Orthopaedic Association (COA), Wisconsin Orthopaedic Society (WOS), Wilson-Bost Orthopaedic Society, Medical College of Wisconsin Orthopedic Surgery alumni, and the Kerlan-Jobe Orthopaedic Fellowship alumni (KJOC) groups were willing to distribute the survey to their membership. The survey was distributed via a survey weblink. Individual physician participation was voluntary and anonymous. The survey was performed by SurveyMonkey.com, which provided data acquisition and analysis. The survey was open from May 15, 2015 through December 31, 2015. Question response totals and percentages were calculated. Survey questionnaire is presented in (http://fp.amegroups.cn/cms/aoj.2019.04.01-1.pdf).
IRB Approval: Cedars-Sinai Office of Research Compliance has determined that the proposed research referenced below is exempt from the requirements for IRB review and approval in accordance with federal regulations, 45 CFR 46.101(b). IRB No. Pro00040463.
Results
A total of 230 responses were obtained for the seven-month collection period.
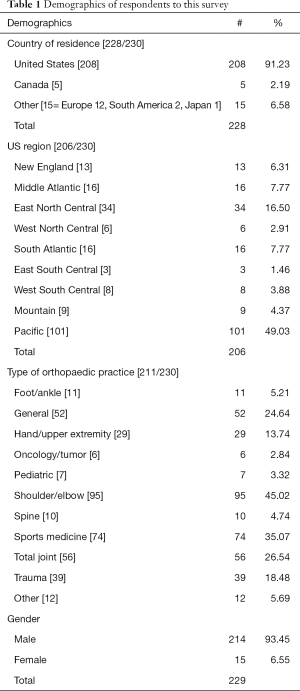
Demographics: respondents were primarily from the United States (Table 1). All regions of the country were represented. The average number years in practice was 21 years. A diverse type and specialty focus within orthopedic surgery was represented (Table 1). The distribution of practice focus is representative of the specialty organizations and orthopaedic groups willing to send out the survey.
Full table
This study first asked whether the respondents believe that metal allergies occurred to orthopaedic implants. 108/157 (69%) believed that metal allergies occur with orthopedic implants, while 29/157 (18%) disagreed. Another 20/157 (13%) stated “other”, such as “not sure”, “I don’t know”, or “possibly”.
Respondents were then questioned if they have had a patient develop a metal allergy to an implant. Twenty-five percent (52/206) of respondents reported having had a patient develop a metal allergy to an implant.
The most commonly seen metal allergies reported were nickel (77/142 positive responses) responses, cobalt (21/142), and chromium (23/142). Titanium (8/142 positive responses), molybdenum (3/142), iron (3/142), aluminum (2/142), and zirconium (1/142) were also observed.
Metal hypersensitivity presented (in decreasing frequency) as pain, swelling, rash/skin manifestation, sterile effusion, osteolysis, and loss of motion (Table 2). Most reactions occurred within one year of implantation (63/110 or 57% of responses). Twenty-six percent (29/110 responses) occurred between one and two years after implantation. Respondents stated that the diagnosis of metal hypersensitivity to an orthopaedic implant was primarily made by consultation with an allergist/dermatologist, along with evaluation of signs and symptoms (Table 2). When testing was performed by orthopaedic surgeons, metal disk and patch testing were performed more frequently than serum testing.
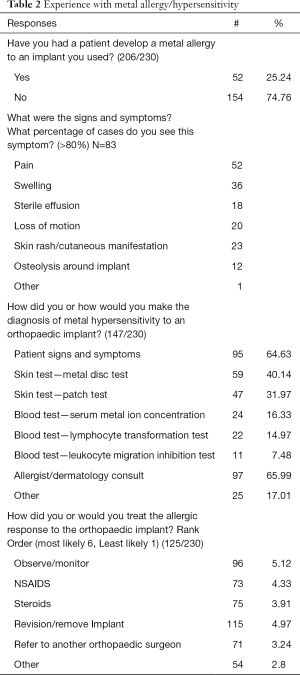
Full table
Revision was listed as the first choice of treatment in 47% of respondents, although this was second in rank order (4.97/6), while observation was listed as first choice by 33% of respondents (first in rank order 5.12/6) (Table 2). The rank order list weighted how the respondents ordered their choice of treatment. First choice was given six points, second choice was given five points, and subsequent choices were given one less point for each position of rank.
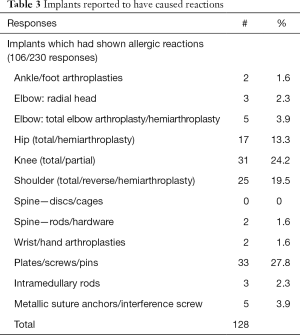
Respondents reported reactions primarily to plates/screws/pins, knee arthroplasties, shoulder arthroplasties, and hip arthroplasties (Table 3).
Full table
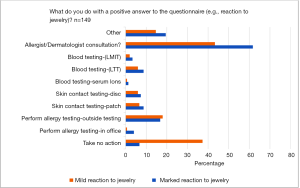
Only 41% of respondents asked their patients if they were allergic to metal or jewelry and only 25% of patient questionnaires included a question about metal allergy (Table 4).

Full table
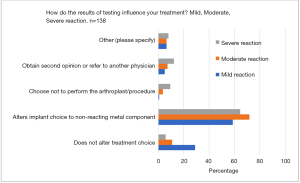
For a reported mild reaction to metal or jewelry, 43% would consult an allergist or dermatologist and 37% would take no action. If a marked reaction were reported, 62% would consult a dermatologist or allergist, only 7% would take no action (Figure 1). Fifty-nine percent of respondents stated that a mild reaction results from allergy testing altered their implant choice, whereas 29% did not alter their choice of implant (Figure 2). When the reaction was moderate, 72% altered their implant choice (11% did not). When the reaction was severe, 64% altered their implant, 12% obtained a second opinion, and 6% did not alter their implant choice.
SurveyMonkey.com raw data results presented in (http://fp.amegroups.cn/cms/aoj.2019.04.01-2.pdf).
Discussion
This study is the first to survey a broad cross-section of orthopedic surgeons across the country and across subspecialty focus to assess their attitudes/opinions on metal allergy, incidence, diagnosis, screening, implant choice changes, and treatment of metal allergy in their patients. A large-scale consensus study does not exist to guide practitioners in how to manage their patients who report a sensitivity to metal or jewelry, nor on how to treat patients who have painful arthroplasties or hardware yet demonstrate a positive metal allergy test. This is a topic of great debate for which there is very little consensus, with recent reviews by Lachiewicz et al., Akil et al., Faschingbauer et al., Middleton et al., and Mitchelson et al. have summarizing the debate on the numerous questions surrounding metal allergies and whether it is a significant issue in orthopaedics (10-12,25,31). The Delphi consensus study is the only prior consensus study performed relating to metal allergy or hypersensitivity in orthopaedic surgery (6). This study surveyed orthopaedic arthroplasty surgeons in the UK in 2013. It consisted of two rounds of questionnaires, which were sent via electronic mail. Ninety joint arthroplasty experts in the UK were surveyed (60 hip/knee surgeons, 30 shoulder/UE surgeons). There was only a 19% response rate (17/90). Absolute agreement could not be obtained, as 60% agreement (10 responses) was set as consensus. Their findings were that patients having metal arthroplasty should not be routinely questioned about metal allergy prior to surgery. If patch testing was performed and the result was negative, then traditional Cobalt-Chromium/stainless steel implants were to be used. If the patients tested positive for cobalt, chromium, or nickel, consensus was also reached that using traditional cobalt-chromium and stainless-steel implants was appropriate. The report concluded that patch testing was not necessary to confirm the presence of metal allergy.
Review of the Delphi study reveals a poor response rate to the questionnaires. Only 17 responses were obtained, which meant that concurrence of only ten responses was considered a consensus. There may be a sampling bias or error due to the limited number of responses. It could be argued that a consensus of 10−17 orthopaedic surgeons does not constitute a “consensus of opinion” but rather an expert opinion.
This study concluded that there is a wide range of beliefs as to whether metal hypersensitivity/allergy is of concern. Sixty-nine percent of respondents believe in metal allergy, 18% do not, and 13% are not sure. Twenty-five percent of respondents have had a patient with a presumed metal allergy. The diagnosis was made primarily by signs and symptoms or consultation with an allergist/dermatologist. Interestingly, only 41% ask their patients if they have a sensitivity to metal and only 25% have a question of metal allergy on their patient intake questionnaires. If the questionnaire noted a mild positive reaction, 37% would take no action whereas the majority would consult an allergist/dermatologist or perform testing. When the questionnaire noted a more severe reaction, only 7% would take no action.
When a positive allergy test was obtained, the actions taken varied by severity of the reaction. For a mild reaction, 29% did not change their implant choice; in cases of moderate reactions—11% did not change implant choice; with a severe reaction—only 6% did not change their implant. Fifty-nine to 72% stated they would change the implant based on severity of reaction. Observation and monitoring ranked first for treatment of a patient with a metal allergy, followed by revision surgery.
The strength of this study is that it includes many orthopaedic surgeons [230] from a broad spectrum of specialties and from all regions of the United States; it also included surgeons from other parts of the world. The limitation is that it is purely the opinions of the surgeons willing to take the survey. Although we asked all the major subspecialty societies to send out the survey to their memberships, several declined to participate in the survey. This may have biased the opinions generated. Overall, the survey does give insight into the beliefs and opinions of the orthopaedic community regarding metal hypersensitivity and allergy.
Further investigational studies will need to be performed to establish a connection between metal sensitivity and the occurrence of pain and implant loosening following arthroplasty procedures. Further studies may demonstrate improvement in arthroplasty outcome and decreases in metal hypersensitivity reactions in patients who have implant choices which are changed due to patient reporting or positive testing to metal hypersensitivity. It is important to consider that such testing can be costly, with metal allergy patch testing typically costing between $60 and $300 USD, with blood tests being between $200−1,000 (32). These tests also may not be covered by patients’ insurance plans, creating a potential in exorbitant cost to patients. It is unclear whether a greater awareness of a history of hypersensitivity will lead to improved outcome and less reactions in joint replacement surgery.
Conclusions
This study is the first to survey orthopedic surgeons on their opinions regarding metal allergy, screening, and treatment. It is unique in that surgeons from a broad geographic representation and across orthopedic subspecialties were surveyed. Orthopaedic surgeons vary in their level of belief on whether metal allergy to orthopaedic implants is of a concern. Sixty-nine percent do believe in metal allergy, but a sizable number (18%) do not believe it occurs. The prevalence of reported metal allergy to an implant was low. These reactions usually occurred within one year of implantation. Surgeons tend to alter their choice of implant more frequently as the reaction becomes more severe on testing. Observation and revision surgery are frequently used to treat an allergic reaction to an implant. Although many orthopaedic physicians would obtain an allergy/dermatology consult or perform metal allergy testing, a minority of orthopaedic surgeons inquire about metal hypersensitivity in their patients and most patient questionnaires do not inquire about metal allergy. Greater awareness of a history of hypersensitivity may prevent patient exposure to implants containing metals that they may react to. Further studies will need to be done to show an improvement in arthroplasty outcome and decreases in metal hypersensitivity reactions in patients who have implant choices which are changed due to patient reported or tested positive to metal hypersensitivity. More evidence is needed to establish a connection between metal sensitivity and the occurrence of pain and implant loosening following arthroplasty procedures.
Acknowledgments
We would like to thank the American Shoulder and Elbow Surgeons (ASES), Orthopaedic Trauma Association (OTA), California Orthopaedic Association (COA), Wisconsin Orthopaedic Society (WOS), Wilson-Bost Orthopaedic Society, Medical College of Wisconsin Orthopedic Surgery alumni, and the Kerlan-Jobe Orthopaedic Fellowship alumni (KJOC) groups for being willing to distribute this survey to their membership.
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Cedars-Sinai Office of Research Compliance has determined that the proposed research referenced below is exempt from the requirements for IRB review and approval in accordance with federal regulations, 45 CFR 46.101(b). IRB No.: Pro00040463.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Amini M, Mayes WH, Tzeng A, et al. Evaluation and Management of Metal Hypersensitivity in Total Joint Arthroplasty: A Systematic Review. J Long Term Eff Med Implants 2014;24:25-36. [Crossref] [PubMed]
- Bloemke AD, Clarke HD. Prevalence of self-reported metal allergy in patients undergoing primary total knee arthroplasty. J Knee Surg 2015;28:243-6. [Crossref] [PubMed]
- Granchi D, Cenni E, Giunti A, et al. Metal hypersensitivity testing in patients undergoing joint replacement: a systematic review. J Bone Joint Surg Br 2012;94:1126-34. [Crossref] [PubMed]
- Morwood MP, Garrigues GE. Shoulder arthroplasty in the patient with metal hypersensitivity. J Shoulder Elbow Surg 2015;24:1156-64. [Crossref] [PubMed]
- Razak A, Ebinesan AD, Charalambous CP. Metal Hypersensitivity in Patients with Conventional Orthopaedic Implants. JBJS Rev 2014;2:1-11. [Crossref] [PubMed]
- Razak A, Ebinesan AD, Charalambous CP. Metal Allergy Screening Prior to Joint Arthroplasty and Its Influence on Implant Choice: A Delphi Consensus Study Amongst Orthopaedic Arthroplasty Surgeons. Knee Surg Relat Res 2013;25:186. [Crossref] [PubMed]
- Schuttelaar MLA, Ofenloch RF, Bruze M, et al. Prevalence of contact allergy to metals in the European general population with a focus on nickel and piercings: The EDEN Fragrance Study. Contact Dermatitis 2018;79:1-9. [Crossref] [PubMed]
- Warshaw EM, Aschenbeck KA, DeKoven JG, et al. Piercing and Metal Sensitivity: Extended Analysis of the North American Contact Dermatitis Group Data, 2007-2014. Dermatitis 2017;28:333-41. [Crossref] [PubMed]
- Atanaskova Mesinkovska N, Tellez A, Molina L, et al. The effect of patch testing on surgical practices and outcomes in orthopedic patients with metal implants. Arch Dermatol 2012;148:687-93. [Crossref] [PubMed]
- Akil S, Newman JM, Shah NV, et al. Metal hypersensitivity in total hip and knee arthroplasty: Current concepts. J Clin Orthop Trauma 2018;9:3-6. [Crossref] [PubMed]
- Lachiewicz PF, Watters TS, Jacobs JJ. Metal Hypersensitivity and Total Knee Arthroplasty. J Am Acad Orthop Surg 2016;24:106-12. [Crossref] [PubMed]
- Middleton S, Toms A. Allergy in total knee arthroplasty: a review of the facts. Bone Joint J 2016;98-B:437-41. [Crossref] [PubMed]
- Thomas P. Clinical and diagnostic challenges of metal implant allergy using the example of orthopaedic surgical implants: Part 15 of the Series Molecular Allergology. Allergo J Int 2014;23:179-85. [Crossref] [PubMed]
- Nam D, Li K, Riegler V, et al. Patient-Reported Metal Allergy: A Risk Factor for Poor Outcomes After Total Joint Arthroplasty?. J Arthroplasty 2016;31:1910-5. [Crossref] [PubMed]
- Thomas P, von der Helm C, Schopf C, et al. Patients with intolerance reactions to total knee replacement: combined assessment of allergy diagnostics, periprosthetic histology, and peri-implant cytokine expression pattern. Biomed Res Int 2015;2015:910156 [Crossref] [PubMed]
- Frigerio E, Pigatto PD, Guzzi G, Altomare G. Metal sensitivity in patients with orthopaedic implants: a prospective study. Contact Dermatitis 2011;64:273-9. [Crossref] [PubMed]
- Zeng Y, Feng W, Li J, et al. A prospective study concerning the relationship between metal allergy and post-operative pain following total hip and knee arthroplasty. Int Orthop 2014;38:2231-6. [Crossref] [PubMed]
- Kręcisz B, Kieć-Świerczyńska M, Chomiczewska-Skóra D. Allergy to orthopedic metal implants — A prospective study. Int J Occup Med Environ Health 2012;25:463-9. [Crossref] [PubMed]
- Kubba R. Cutaneous Complications of Orthopedic Implants. Arch Dermatol 1981;117:554. [Crossref] [PubMed]
- Furrer S, Scherer Hofmeier K, Grize L, et al. Metal hypersensitivity in patients with orthopaedic implant complications-A retrospective clinical study. Contact Dermatitis 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Lionberger DR, Samorajski J, Wilson CD, et al. What role does metal allergy sensitization play in total knee arthroplasty revision? J Exp Orthop 2018;5:30. [Crossref] [PubMed]
- Somerson JS, Hsu JE, Neradilek MB, et al. Analysis of 4063 complications of shoulder arthroplasty reported to the US Food and Drug Administration from 2012 to 2016. J Shoulder Elbow Surg 2018;27:1978-86. [Crossref] [PubMed]
- Pinson ML, Coop CA, Webb CN. Metal hypersensitivity in total joint arthroplasty. Ann Allergy Asthma Immunol 2014;113:131-6. [Crossref] [PubMed]
- Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surg Am 2001;83–A:428-36. [Crossref] [PubMed]
- Mitchelson AJ, Wilson CJ, Mihalko WM, et al. Biomaterial hypersensitivity: is it real? Supportive evidence and approach considerations for metal allergic patients following total knee arthroplasty. Biomed Res Int 2015;2015:137287 [Crossref] [PubMed]
- Saccomanno MF, Sircana G, Masci G, et al. Allergy in total knee replacement surgery: Is it a real problem? World J Orthop 2019;10:63-70. [Crossref] [PubMed]
- Eftekhary N, Shepard N, Wiznia D, et al. Metal Hypersensitivity in Total Joint Arthroplasty. JBJS Rev 2018;6:e1 [Crossref] [PubMed]
- Phedy P, Djaja YP, Boedijono DR, et al. Hypersensitivity to orthopaedic implant manifested as erythroderma: Timing of implant removal. Int J Surg Case Rep 2018;49:110-4. [Crossref] [PubMed]
- Thomas P, Summer B. Implant allergy. Allergol Select 2017;1:59-64. [Crossref] [PubMed]
- Christensen TJ, Samant SA, Shin AY. Making Sense of Metal Allergy and Hypersensitivity to Metallic Implants in Relation to Hand Surgery. J Hand Surg Am 2017;42:737-46. [Crossref] [PubMed]
- Faschingbauer M, Renner L, Boettner F. Allergy in Total Knee Replacement. Does It Exist? HSS J 2017;13:12-9. [Crossref] [PubMed]
- ABIM Foundation. Allergy tests—When you need them and when you don’t. Choosing Wisely. Available online: http://www.choosingwisely.org/patient-resources/allergy-tests/
Cite this article as: Scheidt KB, Schultzel M, Itamura JM. Does metal allergy have relevance in patients undergoing arthroplasty—an electronic survey of surgeon attitudes. Ann Joint 2019;4:25.


