
Then and now, design matters: significant improvements in the clinical and radiological performance of cementless hip resurfacing
Introduction
Metal-on-metal (MoM) bearing with a cemented femoral component and a cementless acetabular shell has historically been the gold standard for fixation in surface arthroplasty (SA) of the hip (1,2). Several studies have reported on the excellent clinical and radiological outcomes of the hybrid hip resurfacing at 10- to 15-year follow-up, with overall survival rates greater than 90% (3-5).
Undoubtedly, cementing has been associated with some disadvantages such as loosening and increased risk of thermal necrosis (6). Although cementing the femoral head increases the contact area between implant and bone, the heat produced from the polymerization process can lead to thermal necrosis of the cancellous bone, depending on the thickness of the cement mantle (7). Furthermore, a cemented femoral component transfers more load through the stem to the surrounding bone, exacerbating stress shielding (8). In this sense, while hip resurfacing preserves bone stock, stress shielding and periprosthetic bone resorption might lead to aseptic loosening over time (8).
Even though initial attempts at cementless femoral fixation showed high failure rates in the early 1990s (9,10), further research by Gross et al., after experimenting with diverse fixation methods, demonstrated outstanding results of a porous-coated component at 7 years of follow-up (11). Potential advantages of cementless femoral fixation include a shorter operative time, no risk of thermal necrosis to bone, less stress shielding and improved longevity with physiologic bone ingrowth over cemented mechanical fixation. Since the early 2000s, there has been a significant increase in the number of companies bringing to market a component with femoral cementless fixation (12).
Since there is a paucity of literature on the clinical performance of cementless designs in SA, we aimed to perform an updated review of the literature on this type of fixation, as well as to report our institutional mid-term survival with a MoM cementless hip design.
Non-porous, non-hydroxyapatite coated femoral designs
Following the catastrophic failure reported for metal-on-polyethylene hip resurfacing (13,14), Wagner and Wagner described the first series of cementless femoral fixation for MoM SA of the hip (10). In their study, bony attachment was achieved by a roughened titanium surface (on the backside) pressed into bone without cement and without a true porous ingrowth surface, whereas a forged cobalt-chrome-molybdenum (CoCrMo) alloy was mounted on the articulating surface (10). This implant was manufactured in 2 versions. In the first form, the cap was screwed onto the reamed femoral head with a large screw thread, similar to a screw cup. However, due to insertion difficulties, a ‘press-fit’ version was developed without the screw. While the first model was used in 12 patients, the second one was used in 23; of the 35 cases, 31 were females and 4 were males (10). The authors described 5 (14.3%) revision surgeries (of which 3 corresponded to femoral loosening) at a short follow-up period of 6 to 54 months.
Almost simultaneously, McMinn et al. performed a pilot study of different types of fixation used over time (9). Between 1991 and 1992, 70 hips were replaced with their first type of resurfacing, which consisted of an uncemented, uncoated, smooth press-fit type femoral and acetabular component. The femoral head had a chamfered-cylinder design with a short stem in order to aid in adequate alignment and to bridge the head/neck junction, an area considered as vulnerable to fracture. Between February 1992 and March 1992, 6 hips received a second design of SA, which was exactly the same as the first but with the addition of hydroxyapatite coating to the shell. Finally, the third design was cemented both at the acetabular and femoral sides and was implanted in 43 hips between 1992 and 1993. At short-term follow-up, the aseptic failure rate was 9%, 0% and 7% for the first, second and third prosthetic designs, respectively. While the cementless designs exhibited more failures on the femoral side, the cemented one had them on the acetabular side (9). Despite short follow-up, the authors thought that the combination of a polar (cemented femoral component and cementless acetabular component) MoM bearing would harvest a method of preserving bone stock in the younger and active patient (9).
Hydroxyapatite-coated femoral implant
In the early 2000s, Lilikakis et al. published their preliminary experience with hydroxyapatite coating as the means of fixation of the femoral head in SA (15). The femoral and acetabular implants of the uncemented version of the Cormet 2000 (Corin; Cirencester, UK) were used; which were made from high-carbon, plasma-sprayed CoCrMo alloy and were hot isostatic pressed and solution annealed. The femoral component was fully hydroxyapatite-coated in the inner surface except for the part of the stem outside the head, which was polished; whereas the cup was coated with vacuum plasma sprayed titanium and hydroxyapatite. The survival rate of 70 implants was 98.6% at a minimum 2-year follow-up, with no femoral fractures, aseptic loosening, or stem radiolucencies. Although thinning of the femoral neck at the inferomedial cup-neck rim was a repeated radiologic finding (27%), it had no clinical implication in their review (15).
Later on, Gross and Liu showed excellent outcomes at a mean of 7.4 years of follow-up in a series of 20 hip resurfacings using the same implant (Corin Cormet 2000 Version-I, Corin; Cirencester, UK) (11). They reported four revisions, none of which were due to aseptic femoral component failure: 2 due to cup loosening, 1 due to a late haematogenous infection, and 1 due to persistent pain despite normal radiographic findings (11).
Likewise, Berstock et al. compared the outcome at 2 years of follow-up of 30 hybrid hip resurfacings to that of 30 uncemented hip resurfacings (Corin; Cirencester, UK) using the transgluteal approach (16). The authors found acceptable radiological and functional results with no radiological complications in both groups, with better femoral offset and femoral seating in the uncemented group and with no evidence of uncemented femoral component loosening. Thus, this study reinforced the concept that cement fixation was not required to maintain stability, thereby removing all potential complications associated with cement (16).
A multicenter evaluation of SAs done with cementless fixation by six surgeons in different centers in the United Kingdom, showed 95% survivorship at 4 to 5 years of follow-up (17). These results were slightly superior to those achieved by the same surgeons using hybrid fixation over the previous 7 to 10 years (12). Interestingly, of 24 failures, only one was clearly attributable to an adverse reaction to metal debris (17).
Dixon et al. were the first to report a 10% failure rate for aseptic loosening and overall revision rate of 15% at a mean 5-year follow-up in 190 patients using the Cormet 2000 (Corin; Cirencester, UK) dual-coat acetabular component (18). The authors observed all of the failures on the acetabular side, with no cases of femoral loosening; they only mentioned one case of femoral neck thinning, suggesting that this issue may be multifactorial and potentially related to stress shielding and biological factors, and/or surgical technique (18).
Even though femoral neck thinning may be a drawback, a randomized controlled trial showed that, through bone mineral density analysis, bone preservation of the femoral neck with a cementless femoral component was significantly better than a cemented one after two years of follow-up (19).
Porous-coated femoral implant
Gross and Liu reported that cement fixation failure (3%) was the most common cause of revision surgery at midterm (average 5.6 years) follow-up with the Corin (Corin, Cirencester, Gloucestershire, UK) hybrid SA, accounting for half of all failures (20). Afterwards, and in order to analyze any component fixation superiority, the same authors performed a comparison of fully porous-coated (cementless Recap femoral component with full coating of titanium plasma spray under the entire undersurface of the femoral component, excluding the stem; Biomet, Warsaw, IN, USA) and hybrid SA (cemented Recap femoral component with grit blast cobalt chrome surface; Biomet, Warsaw, IN, USA) with a minimum 2-year follow-up, concluding that there were no differences in the failure rate nor in the clinical performance between both groups; hence, fully porous-coated femoral components proved to be non-inferior to cemented fixation (21). After having a longer follow-up assessment, the same 2 authors showed that fully porous-coated hip resurfacing had even better clinical and radiological outcomes than those reported by others using hybrid fixation methods at five years post-operatively (22). Recently, the same authors showed that the Kaplan-Meier 10-year implant survivorship using aseptic femoral failure as an end point was 98.9% for the cemented and 100% for the uncemented femoral component in 3,274 cases (23).
In a systematic review of the literature, Girard encouraged the use of ‘fit-and-fill’ cementless femoral components in SA in order to avoid potential complications associated with cement (24). In the same study, Girard also showed his results at a mean of 13.1 (range, 8–16) months with the Conserve Plus cementless femoral component (Wright Medical, Arlington, TN, USA), reporting no revisions due to aseptic loosening. Narrowing of the femoral neck was seen in less than 10% of all hips in that series (24).
Le Duff et al. compared the biomechanics between hybrid and porous-coated fixation and no significant differences were observed in femoral offset or leg length despite implantation with a larger metaphyseal stem to femoral shaft angle in the hybrid group (Table 1) (25).
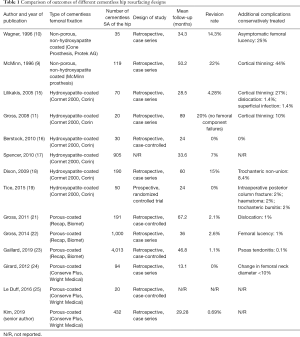
Full table
Institutional experience with a cementless design at our center
The senior author performed 432 consecutive hip resurfacings (13 females, 419 males) between 2009 and 2018, at a large tertiary care centre using the Conserve Plus component (Wright Medical, Arlington, TN, USA) with both cementless femoral and acetabular fixation (Figure 1). All cases were performed through a modified posterolateral approach in the lateral decubitus position (26). Mean follow-up of the series was 2.44 years (range, 1–10.9 years). The two-, five-, and eight-year Kaplan-Meier survivorships were 99.6% (95% CI: 98.8–100%), 98.3% (95% CI: 96.3–100%), and 98.3% (95% CI: 96.3–100%), respectively (Figure 2). There were 3 revisions in the series. Two were for femoral neck fractures and one for aseptic cup loosening. All were treated with revision to a total hip arthroplasty through the same posterolateral approach. There was one infection in the series that was treated with irrigation and debridement and component retention. The patient remains infection free at 5 years follow-up. There were no statistically significant differences in outcomes when comparing males (98.2%, 95% CI: 96.1–100%) with females (100%) (P=0.711).
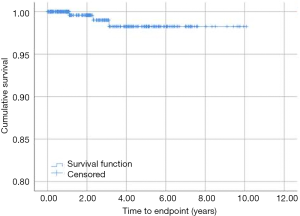
Cementless SA demonstrated excellent survivorship at mid-term follow-up in our series. However, a longer follow-up with at least 10 years is required to assess the potential superiority over cemented devices.
Conclusions
In SA of the hip, cementless femoral fixation has evolved in such a fashion that it is becoming the standard of care in many centers (27). However, there are still several aspects of design that need to be further studied: bearing surface, implant thickness, and optimal fixation coating (28). So far, modern uncemented femoral fixation has proven to be non-inferior to cemented fixation. Long-term clinical trials and large-registry database studies are still necessary to determine whether there is any superiority over cemented fixation.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (George Grammatopoulos and Paul E. Beaulé) for the series “Hip Resurfacing for the Young Arthritic Hip” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.09.01). The series “Hip Resurfacing for the Young Arthritic Hip” was commissioned by the editorial office without any funding or sponsorship. PK reports personal fees and other from Stryker, personal fees from Zimmer Biomet, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Amstutz HC, Beaulé PE, Dorey FJ, et al. Metal-on-Metal Hybrid Surface Arthroplasty: Two to Six-Year Follow-up Study. J Bone Joint Surg Am 2004;86:28-39. [Crossref] [PubMed]
- Amstutz HC, Le Duff MJ. Hip resurfacing: History, current status, and future. HIP Int 2015;25:330-8. [Crossref] [PubMed]
- Daniel J, Pradhan C, Ziaee H, et al. Results of Birmingham hip resurfacing at 12 to 15 years. Bone Joint J 2014;96-B:1298-306. [Crossref] [PubMed]
- Matharu GS, Pandit HG, Murray DW, et al. The future role of metal-on-metal hip resurfacing. Int Orthop 2015;39:2031-6. [Crossref] [PubMed]
- Amstutz HC, Le Duff MJ. Hip Resurfacing: A 40-Year Perspective. HSS J 2012;8:275-82. [Crossref] [PubMed]
- Janssen D, Srinivasan P, Scheerlinck T, et al. Effect of cementing technique and cement type on thermal necrosis in hip resurfacing arthroplasty--a numerical study. J Orthop Res 2012;30:364-70. [Crossref] [PubMed]
- Little JP, Gray HA, Murray DW, et al. Thermal effects of cement mantle thickness for hip resurfacing. J Arthroplasty 2008;23:454-8. [Crossref] [PubMed]
- Pal B, Gupta S, New AM. A numerical study of failure mechanisms in the cemented resurfaced femur: effects of interface characteristics and bone remodelling. Proc Inst Mech Eng H 2009;223:471-84. [Crossref] [PubMed]
- McMinn D, Treacy R, Lin K, et al. Metal on metal surface replacement of the hip. Experience of the McMinn prothesis. Clin Orthop Relat Res 1996;S89-98. [Crossref] [PubMed]
- Wagner M, Wagner H. Preliminary results of uncemented metal on metal stemmed and resurfacing hip replacement arthroplasty. Clin Orthop Relat Res 1996;S78-88. [Crossref] [PubMed]
- Gross TP, Liu F. Metal-on-Metal Hip Resurfacing with an Uncemented Femoral Component. A seven-year follow-up study. J Bone Joint Surg Am 2008;90:32-7. [Crossref] [PubMed]
- Spencer RF. Evolution in hip resurfacing design and contemporary experience with an uncemented device. J Bone Joint Surg Am 2011;93:84-8. [Crossref] [PubMed]
- Freeman MA. Total surface replacement hip arthroplasty. Clin Orthop Relat Res 1978;2-4. [PubMed]
- Amstutz HC, Dorey F, O’Carroll PF. THARIES resurfacing arthroplasty. Evolution and long-term results. Clin Orthop Relat Res 1986;92-114. [PubMed]
- Lilikakis AK, Vowler SL, Villar RN. Hydroxyapatite-coated femoral implant in metal-on-metal resurfacing hip arthroplasty: Minimum of two years follow-up. Orthop Clin North Am 2005;36:215-22. [Crossref] [PubMed]
- Berstock J, Barakat MJ, Annamalais S, et al. An early comparison of clinical and mechanical aspects of hybrid and uncemented hip resurfacing. Eur J Orthop Surg Traumatol 2010;20:623-7. [Crossref]
- Spencer RF. Hip resurfacing, UK experience. Eighth Symposium on Joint Preserving and Minimally Invasive Surgery of the Hip, June 10–12, 2010, Ottawa, Canada.
- Dixon SM, Jeavons L, Reddy RP, et al. Early failure of the dual coat cormet 2000 metal on metal acetabular component. HIP Int 2009;19:128-30. [Crossref] [PubMed]
- Tice A, Kim P, Dinh L, et al. A randomised controlled trial of cemented and cementless femoral components for metal-on-metal hip resurfacing: A bone mineral density study. Bone Joint J 2015;97-B:1608-14. [Crossref] [PubMed]
- Gross TP, Liu F. Eight year clinic outcome of the metal-on-metal hybrid hip surface replacement. AAOS Annual Meeting, New Orleans, United States, 2010.
- Gross TP, Liu F. Comparison of Fully Porous-Coated and Hybrid Hip Resurfacing: A Minimum 2-Year Follow-Up Study. Orthop Clin North Am 2011;42:231-9. [Crossref] [PubMed]
- Gross TP, Liu F. Current status of modern fully porous coated metal-on-metal hip resurfacing arthroplasty. J Arthroplasty 2014;29:181-5. [Crossref] [PubMed]
- Gaillard-Campbell DM, Gross TP. Femoral Fixation Methods in Hip Resurfacing Arthroplasty: An 11-Year Retrospective Comparison of 4013 Cases. J Arthroplasty 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Girard J. Is it Time for Cementless Hip Resurfacing? HSS J 2012;8:245-50. [Crossref] [PubMed]
- Le Duff MJ, Bhaurla SK, Takamura KB, et al. Are there differences in Hip Biomechanics after hybrid and cementless resurfacing arthroplasty? Acta Orthop Belg 2016;82:516-21. [PubMed]
- Steffen RT, De Smet KA, Murray DW, et al. A Modified Posterior Approach Preserves Femoral Head Oxgenation During Hip Resurfacing. J Arthroplasty 2011;26:404-8. [Crossref] [PubMed]
- Girard J. Hip Resurfacing: International Perspectives: Review Article. HSS J 2017;13:7-11. [Crossref] [PubMed]
- Su EP. Design Considerations for the Next Generation Hip Resurfacing Implant HSS J 2017;13:50-3. Commentary. [Crossref] [PubMed]
Cite this article as: Slullitel P, Tubin N, Kim P. Then and now, design matters: significant improvements in the clinical and radiological performance of cementless hip resurfacing. Ann Joint 2019;4:38.



