
Tibial sesamoidectomy: indications and outcomes
Introduction
The hallux sesamoid complex consists of two small bones, the tibial (medial) sesamoid and the fibular (lateral) sesamoid, that lie within the tendon of the flexor hallucis brevis plantar to the first metatarsophalangeal joint of the foot (1). The sesamoids aid in biomechanical functioning of the foot, particularly in walking and running (2). The sesamoids may be excised individually or together as a complex depending upon the indication for surgery. However, whether or not isolated tibial sesamoidectomy results in joint malalignment postoperatively is debated, and the procedure is therefore not commonly performed (3).
The sesamoids function by reducing friction at the first metatarsophalangeal (MTP) joint (4), cushioning the first metatarsophalangeal joint during impact, increasing the maximum flexion force of the first metatarsophalangeal joint, and transmitting up to three times an individual’s body weight during the push-off phase of walking (1). Due to its location under the head of the first metatarsal, larger size (4), and biomechanical function, the medial sesamoid is at risk for traumatic and stress-related injury (5). This makes it the more commonly injured of the two sesamoids (4).
Initial treatment of choice for non-emergent pathologies, such as sesamoiditis and fracture, is conservative, and sesamoidectomy is typically reserved for cases refractory to nonoperative management (6). Indications reported for surgical removal include sesamoid fracture (2,4,5), osteomyelitis (7), plantar keratosis, nonunion (3), and chronic sesamoiditis (3,6). Tibial sesamoidectomy has been shown to be a safe and effective means of symptomatic relief (2,4). Additionally, it has been documented to have few postoperative complications, including transient sesamoiditis and superficial wound infection (4). Whether or not medial sesamoidectomy leads to development of hallux valgus is controversial (2,3).
To our knowledge there are no studies that assess the clinical outcomes of medial sesamoidectomy across a variety of pathological indications for surgery. Because of its documented effectiveness for pain relief and the sesamoids’ integral role in biomechanics of the foot, it is important to understand the role of medial sesamoidectomy in treatment of various foot pathologies, as well as the procedure’s associated postoperative complications, outcomes, and clinical implications. The purpose of this case series is to determine common clinical indications for medial sesamoidectomy and to evaluate the postoperative clinical course and outcomes among a cohort of 26 patients who underwent medial sesamoidectomy.
Methods
The current study was approved by our medical center’s institutional review board. A retrospective chart review was conducted on adult patients who had medial sesamoidectomy at single academic hospital from 2009 to 2018. Twenty-eight patients were identified by CPT code. Those who had total sesamoidectomy, 2, were excluded, yielding a final 26. General medical history was collected for each patient including age, sex, BMI, profession, and risk factors for complications including diabetes, diabetic neuropathy, smoking history, trauma to the foot. Symptom characteristics included side of pathology, injury mechanism, and setting of injury. Physical exam variables included tenderness, edema, ecchymosis, ulceration, among other patient-specific findings. Operative findings reported were bipartite sesamoids, loose bodies, cartilage defects, flexor hallucis longus (FHL) tears, plantar plate tear and any need for flexor hallucis brevis (FHB) repair or adjuvant surgery.
Pre- and post-operative standing three-view X-rays were reviewed by one foot and ankle trained fellow, and data were gathered including bipartite or tripartite of the medial sesamoid, hallux valgus angle (HVA), and intermetatarsal angle (IMA). For patient with an MRI, reports were reviewed to identify any discrepancy.
Preoperative and postoperative visual analog scores (VAS) were obtained for each patient. Postoperative information collected included the following complications: wound breakdown or surgical site infection, post-operative deviation of great toes, and medial plantar nerve neuritis. For patients who had diabetic foot ulcer, time to healing was noted. All patients were called to complete the Foot Function Index (FFI) questionnaire.
Surgical technique
One of three fellowship-trained foot and ankle surgeons performed a partial or complete tibial sesamoidectomy under ankle block. A medial-plantar incision was made overlying the 1st metatarsophalangeal joint. After sharp dissection through the skin and blunt dissection through the subcutaneous tissue while keeping the plantar medial neurovasculature protected, a longitudinal capsulotomy was made on the medial aspect of the joint. The medial sesamoid was removed from its soft tissue sleeve under direct visualization. The flexor hallux brevis was repaired with 2-0 fiberwire if there was loss of continuity. Medial capsulorrhaphy was then performed with careful attention paid to the position of the great toe clinically and under C-arm guidance. The wound was copiously irrigated and closed in layers.
Results
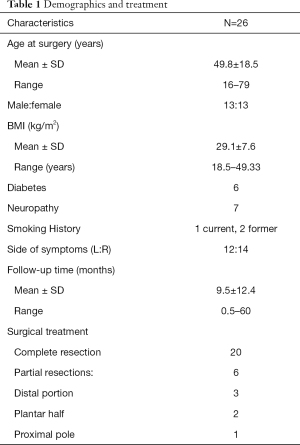
Twenty-six patients (26 feet) were identified for inclusion in this study. The average age was 49.8±18.5 (range, 16–79) years old. There were 13 female and 13 male patients. The surgical site was left in 12 cases and right in 14. Mean follow-up time was 9.5±12.4 (range, 0.5–60) months. BMI averaged 29.1±7.6. Comorbidities included diabetes (6), neuropathy (7), and smoking (3). Table 1 reports demographics and treatment type.
Full table
Among 11 patients who had described professions, four were retired, three had academic vocations, and two were manual laborers. Among the 26 respondents, 14 developed symptoms chronically, 4 from trauma, four from athletics, 2 from hyper-dorsiflexion (1 from athletic group), and 3 from diabetic neuropathy (Table 1).
Physical examination
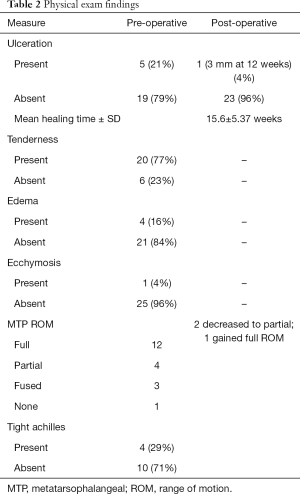
Physical exam results are shown in Table 2. Of the 19 patients who presented without ulceration, 4 recalled a specific injury, including 1 motorcycle collision, 1 basketball game, 1 football game, and 1 fall. On physical examination, all patients without ulcers had tenderness on the plantar surface over the medial sesamoid, 6 had an Achilles contracture, 4 had subtle cavus feet, 3 had planovalgus feet, 3 had specific neuropathies (2 sural and one plantar hallucal), 3 had plantar calluses, and 9 had a mild hallux valgus deformity. The most common presenting symptom was pain with localized tenderness. Other signs at presentation included ulceration, edema, ecchymosis, and tight Achilles tendon. Table 2 displays the physical exam findings of the patients.
Full table
Prior treatment
Six patients had surgery on the same foot before the initial clinic interview. Three patients had a first metatarsophalangeal fusion for hallux rigidus. One patient had a triple arthrodesis, cotton osteotomy, interphalangeal (IP) joint arthrodesis, Z-lengthening of abductor hallucis tendon, and first MTP capsulotomy for a symptomatic cavus foot. One patient had first MTP cheilectomy for hallux rigidus, and another had mid-foot arthrodesis [1,2,3 metatarsal-cuneiform (MTC)] for mid-foot arthritis.
All patients underwent conservative treatment prior to operative intervention, including premade or custom-made shoe inserts, boot, anti-inflammatory medications, physical therapy, and steroid injections. The average duration of non-operative treatment was 20.6±27.6 months (range 3 weeks to 10 years). Twenty-five patients could recall time of onset of symptoms to surgery and average was 26.0±30.7 months (range 3 weeks to 10 years).
Radiographic findings
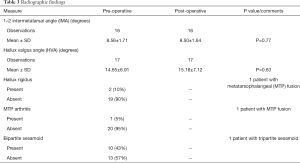
Pre- and post-operative 1–2 IMA values were recorded for 16 patients and HVA values were recorded for 17 patients. Mean pre-operative 1–2 IMA was not significantly different from post-operative 1–2 IMA (8.56º±1.71º vs. 8.50º±1.64º, P=0.77). Mean pre-operative HVA was not significantly different from post-operative HVA (14.65º±6.91º vs. 15.18º±7.12º, P=0.63). Ten of 21 patients (48%) were found to have hallux valgus when defined by either IMA >9º or HVA >15º. Of the 7 patients in this group with radiographic results, there was no statistically significant change pre-operatively to post-operatively in 1–2 IMA and HVA. One patient had a preoperative MTP fusion. Bipartite sesamoids were present in 10 of 23 patients (43%). Hallux rigidus was present in 2 of 21 patients (10%). MTP arthritis was present in only 1 of 21 patients (5%). These findings are reported in Table 3.
Full table
Intra-operative findings
The most common intra-operative findings were a bipartite sesamoid (9/15 or 38%) and plantar plate tears (6 of 21 or 29%). One cartilage defect was found consistent with arthritic changes in the medial sesamoid-metatarsal articulation. No FHL tears or loose bodies were identified.
Additional intraoperative findings included avascular necrosis [4], sclerosis of the sesamoid [2], bony fragmentation [2], hypertrophy of the bone [1], and arthritic changes [1]. The flexor hallucis brevis was repaired in 11 patients. Three patients received adjuvant surgeries. One patient who had plantar hallucal neuropathy underwent neurectomy and redirection to the soft tissue plane. A patient with mild hallux valgus underwent purse-stringing of the flexor brevis to prevent valgus drift of the first metatarsophalangeal joint. Finally, one patient with concomitant equinus had a gastrocnemius recession. Intra-operative findings are displayed in Table 4.

Full table
Outcomes
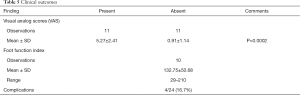
VAS and FFI were the two primary outcome measures, displayed in Table 5. VAS improved significantly from pre-operative period (5.27±2.41) to the post-operative period (0.91±1.14), (P=0.0002). FFI was reported for 10 patients post-operatively with a mean of 132.75±50.68, ranging from 29 to 210. Pre-operative VAS, post-operative VAS, pre-to-post operative change in VAS, and FFI were not significantly correlated with age, BMI, time between injury onset and surgery, or follow-up length. With respect to diabetes, FFI was greater in the group with diabetes (196±19.8) as opposed to those without diabetes (116.9±42.6) (P=0.039).
Full table
Complications
Four of 24 (16.7%) patients developed complications. One patient who began with mild hallux valgus deformity continued to have symptoms postoperatively and elected to have a first metatarsal Chevron osteotomy 1-year postoperatively. Two patients developed post-operative digital nerve neuritis. One patient had persistent cockup deformity that was present pre-operatively (Table 5).
Discussion
The function of the hallux sesamoids is threefold: to absorb weightbearing forces thereby reducing pressure on the first metatarsophalangeal joint, to optimize the lever arm of the flexor hallucis brevis, and to decrease frictional forces beneath the first metatarsophalangeal joint. The tibial sesamoid, occupying the more medial groove beneath the first metatarsal head, is larger and bears more weight during ambulation, and is therefore more prone to injury. Although conservative treatment—orthotics, physical therapy, and activity modification—is often successful, some patients continue to progress symptomatically and eventually require surgical intervention. Tibial sesamoidectomy is indicated after a failure of conservative treatment for a number of conditions: metatarsosesamoid arthritis, sesamoid osteonecrosis, fracture, nonunion, osteomyelitis, and non-healing ulcers. The present retrospective case review is an attempt to validate the indications, findings, and results of isolated tibial sesamoidectomy at a single institution.
The results of medial sesamoidectomy in athletes have been reviewed by many authors. The most common pathology leading to medial sesamoidectomy in athletes is fracture nonresponsive to conservative treatment (5,6). In our study, a majority of patients did not self-identify as athletes. Moreover, the pre-operative diagnosis was more commonly chronic conditions, including sesamoiditis, osteonecrosis and metatarsosesamoid arthritis. In addition to these findings, there was a high incidence of concurrent anatomic variations in our study including contracted heel cords (thought to contribute to sesamoid disorders), subtle cavus feet, planovalgus feet, and hallux valgus deformities. Although care must be taken to tailor the surgical procedure to the patient’s complaints, consideration of coexisting osseous and soft-tissue pathology would be wise before undertaking an isolated procedure.
The reported incidence of bipartite sesamoids varies in the literature from 1% to 33%. Favinger et al. [2015] found that the prevalence of a bi/multipartite sesamoid was 14.3% in their population of 531 patients without sesamoid pathology 82% of which were the tibial sesamoid (8). The most recent systematic review by Shimozono et al. [2018] demonstrated an incidence of approximately 11% in patients undergoing sesamoidectomy (9). Our data revealed an incidence of multipartite tibial sesamoid of approximately 43% (10/23) radiographically and 38% (9/15) surgically. The higher than previously reported percentages of multipartite sesamoids in our study may be the result of a true increased incidence in the medial as opposed to lateral sesamoid, or an increase in pathologic processes with multipartite sesamoids.
A number of studies have demonstrated reliable relief of pain with sesamoidectomy. A systematic review by Shimozono et al. [2018] showed that across 196 feet, isolated tibial or fibular sesamoidectomy reduced preoperative visual analog scale (VAS) for pain from 6.5±0.3 to 1.2±0.5 (9). Another study from Bichara et al. [2012] showed that in their cohort of 24 sesamoid fractures in athletes that failed conservative treatment, sesamoidectomy resulted in a decrease of VAS score from 6.2±1.4 to 0.7±1; 91.6% of patients in their study group returned to their previous level of play (2). In this study, we demonstrated a similar statistically significant reduction in pain post-procedure for medial sesamoidectomy alone, from 5.27±2.41 to 0.91±1.14 (P<0.01). To our knowledge, this study is the first to report on VAS outcomes following isolated tibial sesamoidectomy in a large and diverse cohort.
Few studies have commented on the outcomes of tibial sesamoidectomy for treatment of diabetic ulcerations. In our cohort, 5/24 patients presented with ulcerations directly overlying the tibial sesamoid and were treated with excision. At mean time of 15.6±5.37 weeks, all but one of the treated patients had complete resolution of the ulcer. Sesamoidectomy, when applied judiciously, is an effective adjuvant to the established techniques of surgical equinus correction, total contact casting, and wound care for plantar ulcer healing.
As with any surgical procedure, tibial sesamoidectomy is not without risk for complications. Historical studies demonstrated a high rate of adverse outcomes; however, more recent investigations have reported a more reasonable incidence, likely a result of more meticulous soft tissue tensioning. Shimozono et al. [2018] in their systematic review reported a complication rate of approximately 22.5% with a revision rate of 3.0%. Lee et al. [2005] identified two patients with postoperative transfer metatarsalgia but otherwise acceptable results (10). This study reported a 17% incidence of postoperative complications, consistent with other studies. Two patients developed medial sensory nerve neuritis, one patient developed transfer metatarsalgia, and the last patient had a persistent cock-up deformity postoperatively. These complications reflect known adverse outcomes, and patients undergoing tibial sesamoidectomy should be made aware of their risk prior to intervention.
Several studies have been devoted to describing the risk of iatrogenic hallux valgus deformity following tibial sesamoidectomy, as historically the incidence of this complication was reported to be as high as 42%. Kane et al. [2017] described a cohort of 46 sesamoid fractures treated with sesamoidectomy, 22 of which were medial (4). Their data demonstrated a statistically significant difference in both HVA and IMA between lateral and medial sesamoidectomy patients, with a trend toward increasing HVA and IMA in medial sesamoidectomy patients. They did not report on the statistical significance of the change in HVA and IMA for the medial sesamoidectomy patients alone; however, the authors do mention that while their results were statistically significant, they were not clinically significant as all medial sesamoidectomy patients returned to their preinjury level of activity. Bichara et al. [2012] followed 24 patients who failed conservative treatment for fractures (2). They reported excellent reduction in pain and return to preinjury level of activity with only one patient progressing to symptomatic hallux valgus. Lee et al. [2005] investigated first ray alignment and pedobarographic data following isolated medial sesamoidectomy in 20 patients and did not detect a statistically significant change in either (10). The data from our study is consistent with these previously reported findings. There was no statistically significant change in IMA (8.35º±1.87º to 8.29º±1.79º, P=0.93) or HVA (14.94º±6.82º to 14.28º±7.78º, P=0.79). Despite a 48% prevalence of hallux valgus prior to intervention, only one patient went on to develop a symptomatic first ray which eventually required a chevron osteotomy. We attributed this low incidence of revision to the meticulous medial capsulorrhaphy. Isolated tibial sesamoidectomy does not appear to place patients at greater risk of developing symptomatic hallux valgus requiring surgery, even in cases of preexisting deformity.
This investigation is not without its weaknesses. First, as with any retrospective study, it is subject to historical biases and accuracy of collected data. It also represents of the changing practice patterns of three different fellowship-trained orthopaedic foot and ankle physicians, who may have different indications and surgical techniques. Lastly, by including tibial sesamoidectomies for any indication, the data may be diluted with outcomes data that is not reflective of the intention of the procedure, e.g. ulcer healing as opposed to pain relief.
Conclusions
Isolated tibial sesamoidectomy, when utilized judiciously and with the right indications, can prove to be a very effective procedure. Significant improvements in pain scores and reliable ulcer healing can be expected with a reasonable complication rate. The risk of iatrogenic hallux valgus deformity is largely mitigated with proper soft tissue dissection and tensioning, even in patients with preexisting deformity, and first ray alignment is left unaltered by the procedure.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Vinod K. Panchbhavi and Maninder Shah Singh) for the series “Foot & Ankle Surgery” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: The series “Foot & Ankle Surgery” was commissioned by the editorial office without any funding or sponsorship. AS is a board/committee member of the American Orthopaedic Foot and Ankle Society. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional review board of University of Alabama at Birmingham Approval Number (300000382). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dedmond BT, Cory JW, McBryde A Jr. The hallucal sesamoid complex. J Am Acad Orthop Surg 2006;14:745-53. [Crossref] [PubMed]
- Bichara DA, Henn RF 3rd, Theodore GH. Sesamoidectomy for hallux sesamoid fractures. Foot Ankle Int 2012;33:704-6. [Crossref] [PubMed]
- Canales MB, DeMore M 3rd, Bowen MF, et al. Fact or fiction? Iatrogenic hallux abducto valgus secondary to tibial sesamoidectomy. J Foot Ankle Surg 2015;54:82-8. [Crossref] [PubMed]
- Kane JM, Brodsky JW, Daoud Y. Radiographic Results and Return to Activity After Sesamoidectomy for Fracture. Foot Ankle Int 2017;38:1100-6. [Crossref] [PubMed]
- Biedert R, Hintermann B. Stress fractures of the medial great toe sesamoids in athletes. Foot Ankle Int 2003;24:137-41. [Crossref] [PubMed]
- Saxena A, Krisdakumtorn T. Return to activity after sesamoidectomy in athletically active individuals. Foot Ankle Int 2003;24:415-9. [Crossref] [PubMed]
- Rahn KA, Jacobson FS. Pseudomonas osteomyelitis of the metatarsal sesamoid bones. Am J Orthop (Belle Mead NJ) 1997;26:365-7. [PubMed]
- Favinger JL, Porrino JA, Richardson ML, et al. Epidemiology and imaging appearance of the normal bi-/multipartite hallux sesamoid bone. Foot Ankle Int 2015;36:197-202. [Crossref] [PubMed]
- Shimozono Y, Hurley ET, Brown AJ, et al. Sesamoidectomy for Hallux Sesamoid Disorders: A Systematic Review. J Foot Ankle Surg 2018;57:1186-90. [Crossref] [PubMed]
- Lee S, James WC, Cohen BE, et al. Evaluation of hallux alignment and functional outcome after isolated tibial sesamoidectomy. Foot Ankle Int 2005;26:803-9. [Crossref] [PubMed]
Cite this article as: Peng J, He JK, Christie M, Robin J, McKissack H, Alexander B, Naranje S, Shah A. Tibial sesamoidectomy: indications and outcomes. Ann Joint 2019;4:48.


