Society for translational medicine-expert consensus on the treatment of osteoarthritis
Introduction
Osteoarthritis (OA), also known as osteoarthrosis, is the most prevalent form of joint pathology. It is attributed to diverse causes like joint injury, obesity, aging, and genetic predisposition. The result is the degeneration of the articular cartilage, the subchondral bone, and the entire joint organ. The articular cartilage destruction, typical of OA, is associated with joint space narrowing and periarticular hypertrophic changes. Chronic knee pain significantly affects quality of life (1). People suffering from OA are often confused about the management of their condition. Healthcare professionals must provide support and clear advice on the possible ways to regulate symptoms like pain and decreased physical function, which have an impact on self-efficacy and social engagement.
Symptoms and signs (2)
- Pain: pain in the affected joints can occur in the early stage and it is often well localized. The pain tends to worsen with activity but usually is alleviated by rest. Pain and discomfort in the knee joint after prolonged sitting, for example, is an early symptom of knee OA; persistent pain with weightbearing activities and nocturnal pain may occur in severe cases or in the advanced stages; pain intensity is poorly correlated with joint space narrowing (3); ultimately, pain may or may not be triggered by changes in weather.
- Stiffness: joint stiffness or tightness typically occurs after waking up in the morning, although it is relatively mild, lasts for a limited period of time (e.g., 30 minutes), and improves with activity.
- Joint effusion: local inflammation and synovitis often lead to joint effusion, both during the acute exacerbations of OA as well as later in the severe stages of the disease.
- Tenderness: tissues including muscles and ligaments around the affected joint may suffer from tenderness on palpation.
- Clicking/crepitus: these are usually signs of advanced OA, especially when articular cartilage wear or tear is present. As a result, clicking, catching and crepitus may be heard or felt during joint motion.
- Limitation of joint movement or function: the affected joints can suffer from various degrees of reduction in movement, and flexion contractures often occur over time.
- Joint deformity: in advanced or severe OA cases, joint deformity often occurs due to major osteophyte formation and bony erosion leading to mal-alignment. Varus, valgus and flexion deformities are common in the knee joint.
Radiographic findings (4)
The diagnosis of OA can usually be made on clinical grounds alone. In most cases, standard radiological evaluation can be used to confirm a clinical relevant OA diagnosis. Radiographic evaluation is worldwide used for grading of OA both for research and clinical use. The main radiographic findings include bony hyperplasia at joint margin, osteophyte formation, increased subchondral bone density, and cystic degeneration. In more advanced cases joint space narrowing (or even disappearance) and deformities in the joint alignment may be visible. Modern CT scanning can in some cases be useful as well. However, the sensitivity of X-ray is low to detect the improvement in cartilage remodeling.
MRI
Magnetic Resonance Imaging (MRI) is not a first line diagnostic tool. Nevertheless, it can detect an early degeneration, articular cartilage thinning and destruction, and can also reveal different intra-articular comorbidities, like meniscal tears, ligament injuries, synovial hyperplasia and joint effusion. Moreover, bone edema, associated with OA activity and progression, is detected. T2 sequences, dGemric and sodium MRI offers new possibility of assessing quality & functionality of cartilage tissue. The water content is a reflection of proteoglycan in the extracellular matrix (ECM), and is quantified through these new MRI analyses.
Laboratory tests (5)
Routine and biochemical blood and urine tests typically show normal results. Erythrocyte sedimentation rate (ESR) and C reactive protein (CRP) are within the normal ranges but occasionally may be increased slightly. Serum immune complexes and complements are also normal.
Treatment
General treatment
Exercise therapy (ET) (strongly recommended)
The growing body of evidence has shown that exercise interventions may improve pain, function and quality of life in patients with knee OA (6). Low-intensity aerobic activities are highly recommended: walking and cycling represent first line activities together with swimming and water aerobics. The main purpose of ET is to improve periarticular strength (e.g., quadriceps femoris muscle, hip abductors and external rotators and calf muscles); improving ROM and augmenting proprioception represent other goals of an ET program. In a RCT, it has shown that all modes of aerobic exercise (lower limbs with and without weight bearing and upper limb) combined with resistance training may lead to reduced pain and improved function in mild to moderate knee OA (7,8). Besides, Moderate quality evidence suggests that exercise reduces pain; improves physical function, has small benefits for depression, little or no effect on anxiety. There is low quality evidence that exercise improves self-efficacy and social interaction (9). In the scenario of isolated patellofemoral arthritis, walking (120–140 steps per minute) and cycling are highly recommended since more challenging sports, such as mountain-climbing and stair-climbing, should be avoided. However, assessment and correction of the modifiable risk factors may bring additional treatment effects on pain and function (8). Obese patients and patients with severe, multi-joint arthritis should perform low-load exercises (10-12).
Mind-body intervention—Tai Chi (strongly recommended)
Mind-body intervention are highly recommended. Studies have suggested that mind-body intervention/exercises, particularly the Tai Chi, may be a promising treatment option for patients with KOA. For instance, investigators found that Tai Chi (13-16) a popular mind-body exercises, can significantly reduce KOA pain. Similar finding has also been observed in Baduanjin (15-17), another popular mind-body intervention.
Activities modification (generally recommended)
Weight reduction. The aim of such a program would be to achieve a normal BMI with the goal to reduce the weight being transferred through the joint to reduce symptoms and further joint destruction. A healthy weight loss program should aim for at least 5% of body weight reduction by its end or to reduce 0.25% of body weight weekly within a 20-week timeframe; at the end of this, the ideal body weight should be maintained through proper exercise and diet (18). Female patients should also avoid wearing high-heeled shoes (19) (generally recommended). Patients engaging in high-intensity exercise or heavy physical work should reduce or avoid such exercise or work.
Patient education and supervision (strongly recommended)
Both verbal and written information on OA should be provided for patients and a close connection with them, in terms of scheduled follow-ups, should be established (20,21). Research has found 1a level of evidence for the effect of patient education on pain in knee and hip OA. Education techniques have benefits also in improving function, increasing coping skills, improving psychological outcomes and fewer visits to primary physician and improved quality of life (22-24).
Non-pharmaceutical therapies
Such treatments, including hydrotherapy, thermotherapy, cryotherapy, acupuncture and moxibustion, transcutaneous electrical nerve stimulation (TENS), neuromuscular electrical stimulation (NMES), photobiomodulation therapy (PBMT), and massage have been used because of their capabilities of increasing local blood circulation, alleviating pain and/or inflammation, increasing muscle structure and muscle force, and increasing functionality.
Hydrotherapy/balneotherapy
Hydrotherapy can be applied for multiple-joint OA (strongly recommended) and isolated knee OA (limitedly recommended). Hydrotherapy is suitable for the treatment of OA and other symptoms similar to OA in multiple joints (25,26). However, its role in treating isolated knee OA remains unclear due to the limitations in multiple study designs and poor overall evidence (27,28).
Thermotherapy (moderately recommended)
Thermotherapy can improve the local blood supply to the joint affected by OA. By increasing collagen fibers, it can improve joint function, increase pain threshold, improve muscle metabolism, and thus achieve an overall analgesic effect. However, thermotherapy may cause increased fluid exudation into the periarticular area and exacerbate the symptoms when used in the acute phase. Therefore, use of thermotherapy is recommended only in the remission stage of the disease (29,30).
Cryotherapy (moderately recommended)
Cryotherapy can relieve pain by alleviating local inflammation (31,32) and reducing the conduction velocity of nerve impulses (33). It is especially suitable for the treatment of OA in the acute phase.
Acupuncture and moxibustion (strongly recommended)
Many studies have shown that acupuncture and moxibustion can improve knee function and relieve pain (34,35). A recent meta-analysis found that acupuncture had more total effective rate, short-term effective rate, and less adverse reactions than western medicine in treating KOA based on high-quality outcomes (36). In another systematic review on laser Acupuncture, a less commonly used acupuncture modality, indicated that the laser acupuncture can effectively reduce knee pain in patients with KOA at short term, but the effect obtained likely fades away during the subsequent follow-up period (37). Interestingly, a Network Meta-Analysis on efficacy comparison of five different acupuncture methods showed that acupuncture with heat pain (fire needle) or electrical stimulation might produce better improvement in all acupuncture methods to OA of the knee (38). In addition to acupuncture, a recent meta-analysis on moxibustion suggest that it is effective for pain reduction and symptom management in KOA compared to sham moxibustion and oral drugs (39). Therefore, acupuncture, particularly the electroacupuncture, as well as moxibustion are recommended for treatment of OA.
Electrical stimulation and TENS (limitedly recommended)
TENS is a non-pharmacologic and non-invasive peripheral stimulation technique that is used to relieve nociceptive, neuropathic, and musculoskeletal pain (40,41). During TENS pulsed electrical currents are delivered across the intact surface of the skin to activate underlying nerves (42). The goal of conventional TENS is to stimulate selectively large diameter, low threshold non-noxious afferents (A-beta) in dermatomes related to the pain. This should inhibit activity in second order nociceptive transmission neurons in the central nervous system, and is achieved by increasing TENS pulse amplitude to generate a strong, comfortable, non-painful paraesthesia beneath the electrodes (42). However, as shown in six studies with good level of evidence, electrical stimulation and TENS had no significant effect in alleviating pain, improving function, or strengthening periarticular muscles in OA patients (29,43-45).
NMES (moderately recommended)
NMES can be defined as the application of a series of intermittent electrical stimuli to a group of intramuscular nerve branches that determine visible skeletal muscle contractions with the aim of restoring muscle function (46). The best-evidence analysis showed moderate evidence in favor of NMES alone or combined with exercise for isometric quadriceps strengthening in elderly with OA (47). In addition, there is increasing evidence that NMES has a significant effect on improving periarticular muscles structure and strength (48-51), decreasing pain (52) and improving OA patients’ health status (49). As muscle weakness is a risk factor for OA development and progression, improving periarticular muscles structure and function might alleviate joint contact forces, thereby reducing the mechanical risk factor of OA development and/or progression.
PBMT or low-level laser therapy (LLLT) (limitedly recommended)
PBMT, also known as LLLT, is a form of light therapy that utilizes non-ionizing forms of light sources, including lasers, LEDs, and broadband light, in the visible and infrared spectrum. PBMT is a nonthermal process involving endogenous chromophores eliciting photophysical (i.e., linear and nonlinear) and photochemical events at various biological scales. This process results in beneficial therapeutic outcomes including but not limited to the alleviation of pain or inflammation, immunomodulation, and promotion of wound healing and tissue regeneration (53,54). There is increasing evidence showing positive effects of PBMT in patients with OA. PBMT has been shown to increase knee-extensor muscle activation and knee-extensor torque in elderly with knee OA after an 8-week intervention program (51). PBMT has also been shown to reduce pain in knee OA (55,56) and to improve microcirculation in the irradiated area (55). However, a systematic review and meta-analysis (57) evaluated the effectiveness of PBMT on symptoms and function in patients with knee OA, and concluded that the best available current evidence does not support the effectiveness of PBMT as a therapy for patients with knee OA. Therefore, additional high quality randomized clinical trials need to be performed before a final conclusion can be reached regarding the use of PBMT to treat OA. Nevertheless, there is new evidence from OA experimental models (58) that PBMT promotes cartilage recovery and reduces the progression or maintenance of spinal cord sensitization, suggesting a potential role of PBMT in reducing cartilage degradation and long-term central sensitization associated with chronic OA (59).
Electromagnetic fields (limitedly recommended)
Current evidence suggests that electromagnetic field may provide moderate benefit for OA sufferers in terms of pain relief (60).
Massage (limitedly recommended)
For non-acute knee and hip OA, massage, combined with multiple exercise techniques, can reduce pain and improve functions (28,58,61). A meta-analysis including 352 patients found low- to moderate-quality evidence that massage can produce greater effect than nonactive therapies in reducing pain and improving certain functional outcomes in patients with arthritis (62).
Mobility assistive devices (moderately recommended)
Mobility assistive devices are designed to reduce weight bearing on the affected joints. Canes, crutches, and other walking aids may be used. Patients should be encouraged to wear soft, flat, thick-soled and casual shoes. It is recommended to use walking aids and auxiliary equipment both at work as well as during activities of daily living. Canes are particularly suitable for patients with isolated knee or hip OA. A cane or crutch may be used by a patient with unilateral limb disease on the contralateral healthy side, whereas a walking frame or a wheeled walker is more suitable for patients with bilateral diseases. Notably, the use of crutches may occasionally cause secondary injuries such as brachial plexus and radial nerve traction injuries, lymphatic carcinogenesis, arteriosclerosis, wrist sprains, and lateral chest wall abrasions (26,63-65). For patients with hip or knee OA, soft, flat, thick-soled, and casual shoes are highly recommended by the current literature (66,67).
Unloading Knee braces, regular knee braces and knee pads (moderately recommended)
According to the type of deformity associated with knee OA (i.e., varus or valgus), corresponding biomechanical interventions are recommended to alter a non-anatomical mechanical axis. For instance, unloading knee braces, regular knee braces, knee pads, and foot orthoses may be applied to balance the load between the medial and lateral tibial plateau, which have been shown to be effective in reducing pain, joint stiffness, and medications use and dosage (26,68-73).
Lateral wedge insoles (not recommended)
Lateral wedge insoles to correct varus mal-alignment of the knee may be used according to patients’ symptoms; however, relevant clinical evidence is still lacking.
Functional diets, herbs and antioxidants supplements
Apart from indirect action of functional foods and herbs that help in reducing body weight and improving OA, there is an increasing interest on the direct and beneficial role of a balanced nutrition on the management of OA (74). Consumption of diets, fruits and herbs rich in antioxidants including vitamin A (Carotenoids), vitamin C (Ascorbate) and Vitamin E (tocopherol) limits damaging effects of reactive oxygen species (ROS) and therefore moderately improves OA (75). Diets rich in vitamin K mainly Phylloquinones (vitamin K1) help in mineralization of bones and cartilage. Herbs from Indian medicine (Ayurvedic) as well as Chinese and Taiwanese herbs like Du-huo-ji-sheng-tang have been reported to have moderate efficacy on OA (76). A recent randomized clinical trial reports the beneficial use of cucumber extracts against Glucosamine-Chondroitin for the reduction of pain intensity and improvement of physical conditions of patients suffering from moderate OA. Fishoil (omega 3) has been recommended for OA patients as well. However, evidence from quality clinical studies are missing despite some support from animal studies (77,78).
Pharmaceutical treatment: when non-pharmaceutical options fail, pharmaceutical treatments should be applied according to the severity of joint pain
Topical medications (strongly recommended)
Before the use of oral medications, topical drug therapy is recommended. Topical drugs include pastes, creams, gel pastes, and ointments, gels, and liniments containing non-steroidal anti-inflammatory drugs (NSAIDs). They can effectively relieve mild and moderate joint pain. Topical NSAIDs to treat OA pain have comparable efficacies to their oral counterparts, having fewer adverse reactions. The combined use of both oral and topical NSAIDs may be considered for patients with severe osteoarthritic pain (79).
Systemic analgesics (80 )
Systemic analgesics may be administered as oral, injection or suppository.
- Principles of drug administration:
- Any potential risk should be assessed before the administration of systemic analgesics, in particular the potential risk of GI bleeding and allergic reactions;
- The dosing of systemic analgesics should be tailored to the patient’s conditions;
- The minimum effective dose should be used when possible, in order to avoid drug overdose especially in the scenario of concomitant use of similar drugs;
- After 3 months of treatment, routine blood and stool tests, fecal occult blood test and liver and kidney function tests should be performed in order to detect any abnormalities deriving from the use of a new medication.
- Drugs and their usage
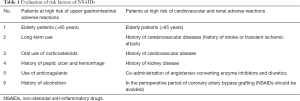
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (strongly recommended): NSAIDs include non-selective NSAIDs and selective COX-2 inhibitors. Efficacy and adverse effects of oral NSAIDs may vary in different patients. Any drugs should be carefully selected by referring to its indications and after assessing any NSAIDs-associated and district related risk factors, including gastrointestinal, liver, kidney, and cardiovascular (Table 1). In the scenario of elevated risk factors for gastrointestinal complication risk, selective COX-2 inhibitors should be used. Alternatively, non-selective NSAIDs combined with H2 receptor antagonists, proton pump inhibitors, misoprostol, or other gastric mucosal protective agents should be used. If the patient is at high risk for developing cardiovascular disease, the use of selective COX-2 inhibitors should be used cautiously. The co-administration of two NSAIDs should be avoided because it does not increase the therapeutic effect but may increase the collateral side effects.
 Table 1 Evaluation of risk factors of NSAIDs
Table 1 Evaluation of risk factors of NSAIDs
Full table - Acetaminophen (generally non-recommended): in a recent meta-analysis, acetaminophen was shown to have minimal short-term benefit for people with OA (81). In addition, there is increased concern for acetaminophen toxicity (82).
- Other analgesics (generally recommended): for OA patients in whom NSAIDs are ineffective or poorly tolerated, tramadol, opioid analgesics, or compound opioid/paracetamol analgesics may be used (83). However, opioid abuse in chronic non-cancer pain is problematic—long-time daily use not to be recommended for OA pain, for most patients (84,85).
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (strongly recommended): NSAIDs include non-selective NSAIDs and selective COX-2 inhibitors. Efficacy and adverse effects of oral NSAIDs may vary in different patients. Any drugs should be carefully selected by referring to its indications and after assessing any NSAIDs-associated and district related risk factors, including gastrointestinal, liver, kidney, and cardiovascular (Table 1). In the scenario of elevated risk factors for gastrointestinal complication risk, selective COX-2 inhibitors should be used. Alternatively, non-selective NSAIDs combined with H2 receptor antagonists, proton pump inhibitors, misoprostol, or other gastric mucosal protective agents should be used. If the patient is at high risk for developing cardiovascular disease, the use of selective COX-2 inhibitors should be used cautiously. The co-administration of two NSAIDs should be avoided because it does not increase the therapeutic effect but may increase the collateral side effects.
Intraarticular injections
- Corticosteroids
- In patients having failed standard NSAIDs treatment, intraarticular injection of glucocorticoids is a feasible (26,85,86) next step treatment, which might achieve significant and fast pain relief. However, long-term use is not recommended, and repeated use should be avoided, as they may become less effective leading to more severe cartilage destruction. Generally, injection should not be repeated more than 3–4 times annually.
- Viscosupplementation
- Growth factors or platelet-rich plasma (PRP) PRP, i.e., an autologous blood derivative rich in growth factors, may be used for intra-articular injection if the triple injections fail (HA + corticosteroids + lidocaine). A few trials have shown that PRP is superior to placebo in terms of symptomatic relief and functional recovery (89,90). Anyway, currently available randomized controlled trials against viscosupplementation were unable to detect a clear superiority of PRP compared to HA, thus preventing endorsement of this blood-derived product as a first line treatment for OA.
- Mesenchymal stem cell (MSC) therapy (under clinical investigation).
The poor self-healing ability of articular cartilage advocates for triggering regeneration through different pathways, including stem cell therapy. Conventional and current surgical treatment procedures for OA are incapable of reversing the damage of articular cartilage. To overcome these hurdles, cell-based therapies are currently being investigated to repair and regenerate the structure and function of articular tissues. In particular, in clinical practice, the use of MSCs has been tested. MSCs can be obtained from different sources [bone marrow (BM), synovial fat pad, adipose tissue, peripheral blood, placental tissue] and can be concentrated or expanded in laboratory for subsequent intra-articular delivery. The most commonly adopted strategies involve the use of bone marrow concentrate (BMC), bone marrow-derived MSCs (BM-MSCs), adipose-derived MSCs (AD-MSCs). In the former case, BM is harvested and concentrated by centrifugation to obtain a product rich in MSCs; in the latter, after a liposuction from the abdominal area or buttocks, the lipoaspirate is treated usually by adding collagenases to digest the ECM and, after filtration or centrifugation, the final output is obtained, containing AD-MSCs together with endothelial cells, pericytes, macrophages and other cellular types, all playing a therapeutic role within the joint (95).
Compare uncultured concentrated cells, cultured cells include a high-purity stem cells that can fulfill their potential for tissue regeneration, and possess paracrine and immune-modulating effects through growth factor and cytokine release (96). There have been a few clinical trials of OA treatment using cultured autologous peripheral blood stem cells (97), allogenic (98) or autologous (99) BM-derived stem cells, autologous adipose tissue-derived MSCs (AD-MSCs) (100) and allogenic human umbilical cord blood MSCs (101), the results confirmed through meta-analysis a modest improvement in function and pain (WOMAC score) of the knee joint without causing adverse events. Further MRI studies in the long term are needed to demonstrate a reduction in cartilage defects by regeneration of hyaline-like articular cartilage. As Caplan, the father of MSCs mentioned, the stem cell therapy for KOA could be a promising option, while the clinical evidence is lacking so far (102).
Symptomatic slow-acting drugs for OA (SYSADOAs)
This drugs category includes diacerein, glucosamine, avocado soybean, unsaponifiables (ASU) and chondroitin. While it has been shown that they have certain roles in protecting cartilage and relieving symptoms, their clinical treatment efficacy on OA remains very controversial (26,83,87,93,94). For example, in a recent study, pharmaceutical-grade chondroitin sulfate was found to be superior to placebo and similar to celecoxib (103). Nonetheless, methodological issues make it difficult to consider the results to be conclusive (104). Diacerein is an IL-1 inhibitor, and its oral treatment for OA might last up to 3 months.
Antidepressants
Duloxetine can effectively alleviate the persistent pain in OA patients and thus can be used as an oral medication for OA. Notably, it has high incidences of side effects such as nausea and developing dry mouth (26,87,88,91,93-95).
Surgical treatment
High tibial osteotomy for treating knee OA (moderately recommended)
For patients with isolated symptomatic medial or lateral compartment knee OA, osteotomies (e.g., high tibial osteotomy or distal femoral osteotomy) to correct eventual misalignment could be performed, with the aim of unloading the affected compartment. The results are especially good for medial knee OA and replacement surgery can be delayed following osteotomy (105). Osteotomy was suggested to be considered for younger patients, which could be often combined with arthroscopic procedures if indicated. Furthermore, to protect cartilage, some concurrent procedures may be associated with osteotomy, such as ligaments reconstructions in case of symptomatic instability, meniscal transplantation in case of previous meniscectomy and chondral/osteochondral treatments if focal defects are present. The indication to this specific approach should be carefully evaluated based on the patient’s age, gender, occupation, functional requirements, and other factors (88). Arthroscopic surgery alone, including debridement, partial synovectomy and meniscus, was not supported by clinical evidence in the literature. However, Arthroscopic surgery may be beneficial in treating severe mechanical problems or inflammation. Sometimes arthroscopic examination is useful to find the best surgical treatment for the patient as well (106).
Joint replacement surgery
- Total joint replacement (strongly recommended)
- Joint replacement surgery may be recommended for patients with advanced stages of shoulder, hip, knee, and ankle OA, in whom pain, stiffness, and function have not improved after conservative treatment with medical or non-medical interventions. For patients with persisting or worsening symptoms, associated or not with functional limitation, joint replacement surgery is highly efficient and cost-effective and can significantly improve the patients’ quality of life.
- Unicompartmental Knee Replacement (generally recommended)
- In case of unicompartmental knee OA in stable joints in patients without major axial deviation and no history of rheumatic disease, unicompartmental knee replacement is a feasible and effective treatment option, which allows a faster recovery and less morbidity for the patient.
Joint replacement surgery is rated as a safe and effective procedure for patients with advanced OA (2). However, in the future, infections may be even more problematic than today due to antibiotic resistance. Infections and other risk factors must always be considered as well.
Conclusions
The diagnosis of OA can be made clinically according to the patient’s signs and symptoms, and affirmed with radiological investigations. There are numerous non-operative measures, non-pharmacological and pharmacological, that can help control the patients’ symptoms. However, if these should fail, with persistent pain and functional limitation, operative intervention may be an option, but the patient should recognize that this does carry the risks of potential surgery complications.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.12.13). DS serves as unpaid Executive Editor-in-Chief of Annals of Joint from Mar 2016 to Feb 2021. SI serves as Editor-in-Chief of Annals of Joint from Mar 2016 to Feb 2021. FHF serves as unpaid Honorary Editor-in-Chief of Annals of Joint from Sep 2019 to Aug 2021. JL serves as an unpaid editorial board member of Annals of Joint from Jun 2018 to May 2020. QJ serves as an Editor-in-Chief of Annals of Joint from Mar 2016 to Feb 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Martel-Pelletier J, Barr AJ, Cicuttini FM, et al. Osteoarthritis. Nat Rev Dis Primers 2016;2:16072. [Crossref] [PubMed]
- Glyn-Jones S, Palmer AJ, Agricola R, et al. Osteoarthritis. Lancet 2015;386:376-87. [PubMed]
- Perrot S, Bertin P. "Feeling better" or "feeling well" in usual care of hip and knee osteoarthritis pain: determination of cutoff points for patient acceptable symptom state (PASS) and minimal clinically important improvement (MCII) at rest and on movement in a national multicenter cohort study of 2414 patients with painful osteoarthritis. Pain 2013;154:248-56. [Crossref] [PubMed]
- Boesen M, Ellegaard K, Henriksen M, et al. Osteoarthritis year in review 2016: imaging. Osteoarthritis Cartilage 2017;25:216-26. [Crossref] [PubMed]
- Zhang W, Doherty M, Peat G, et al. EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis 2010;69:483-9. [Crossref] [PubMed]
- Fransen M, McConnell S, Harmer AR, et al. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med 2015;49:1554-7. [Crossref] [PubMed]
- Kabiri S, Halabchi F, Angoorani H, et al. Comparison of three modes of aerobic exercise combined with resistance training on the pain and function of patients with knee osteoarthritis: A randomized controlled trial. Phys Ther Sport 2018;32:22-8. [Crossref] [PubMed]
- Halabchi F, Mazaheri R, Mansournia MA, et al. Additional Effects of an Individualized Risk Factor-Based Approach on Pain and the Function of Patients With Patellofemoral Pain Syndrome: A Randomized Controlled Trial. Clin J Sport Med 2015;25:478-86. [PubMed]
- Hurley M, Dickson K, Hallett R, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev 2018;4:CD010842 [PubMed]
- Richmond J, Hunter D, Irrgang J, et al. American Academy of Orthopaedic Surgeon clinical practice guideline on the treatment of osteoarthritis (OA) of the knee. J Bone Joint Surg Am 2010;92:990-3. [Crossref] [PubMed]
- Bennell KL, Hinman RS. A review of the clinical evidence for exercise in osteoarthritis of the hip and knee. J Sci Med Sport 2011;14:4-9. [Crossref] [PubMed]
- Kroon FP, van der Burg LR, Buchbinder R, et al. Self-management education programmes for osteoarthritis. Cochrane Database Syst Rev 2014;CD008963 [PubMed]
- Wang C, Schmid CH, Iversen MD, et al. Comparative effectiveness of Tai Chi versus physical therapy for knee osteoarthritis: A randomized trial. Annals of Internal Medicine 2016;165:77-86. [Crossref] [PubMed]
- Lee AC, Harvey WF, Price LL, et al. Dose-Response Effects of Tai Chi and Physical Therapy Exercise Interventions in Symptomatic Knee Osteoarthritis. PM R 2018;10:712-23. [Crossref] [PubMed]
- Liu J, Chen L, Chen X, et al. Modulatory effects of different exercise modalities on the functional connectivity of the periaqueductal grey and ventral tegmental area in patients with knee osteoarthritis: a randomised multimodal magnetic resonance imaging study. Br J Anaesth 2019;123:506-18. [Crossref] [PubMed]
- Liu J, Chen L, Tu Y, et al. Different exercise modalities relieve pain syndrome in patients with knee osteoarthritis and modulate the dorsolateral prefrontal cortex: A multiple mode MRI study. Brain Behav Immun 2019;82:253-63. [Crossref] [PubMed]
- An B, Dai K, Zhu Z, et al. Baduanjin Alleviates the Symptoms of Knee Osteoarthritis. The Journal of Alternative and Complementary Medicine 2008;14:167-74. [Crossref] [PubMed]
- Christensen R, Bartels EM, Astrup A, et al. Effect of weight reduction in obese patients diagnose with knee osteoarthritis: a systematic review and meta-analysis. Ann Rheum Dis 2007;66:433-9. [Crossref] [PubMed]
- Kerrigan DC, Johansson JL, Bryant MG, et al. Moderate-heeled shoes and knee joint torques relevant to the development and progression of knee osteoarthritis. Arch Phys Med Rehabil 2005;86:871-5. [Crossref] [PubMed]
- Goeppinger J, Armstrong B, Schwartz T, et al. Self-management education for persons with arthritis: Managing comorbidity and eliminating health disparities. Arthritis Rheum 2007;57:1081-8. [Crossref] [PubMed]
- Conaghan PG, Dickson J, Grant RL. Care and management of osteoarthritis in adults: summary of NICE guidance. BMJ 2008;336:502-3. [Crossref] [PubMed]
- Ilieva EM, Oral A, Kucukdeveci AA, et al. Osteoarthritis. The role of physical and rehabilitation medicine physicians. The European perspective based on the best evidence. A paper by the UEMS-PRM Section Professional Practice Committee. Eur J Phys Rehabil Med 2013;49:579-93. [PubMed]
- Bezalel T, Carmeli E, Katz-Leurer M. The effect of a group education programme on pain and function through knowledge acquisition and home-based exercise among patients with knee osteoarthritis: a parallel randomised single-blind clinical trial. Physiotherapy 2010;96:137-43. [Crossref] [PubMed]
- Devos-Comby L, Cronan T, Roesch SC. Do exercise and self-management interventions benefit patients with osteoarthritis of the knee? A metaanalytic review. J Rheumatol 2006;33:744-56. [PubMed]
- Falagas ME, Zarkadoulia E, Rafailidis PI. The therapeutic effect of balneotherapy: evaluation of the evidence from randomized controlled trials. Int J Clin Pract 2009;63:1068-84. [Crossref] [PubMed]
- Harzy T, Ghani N, Akasbi N, et al. Short- and long-term therapeutic effects of thermal mineral waters in knee osteoarthritis: a systematic review of randomized controlled trials. Clin Rheumatol 2009;28:501-7. [Crossref] [PubMed]
- Sherman G, Zeller L, Avriel A, et al. Intermittent balneotherapy at the Dead Sea area for patients with knee osteoarthritis. Isr Med Assoc J 2009;11:88-93. [PubMed]
- Forestier R, Desfour H, Tessier JM, et al. Spa therapy in the treatment of knee osteoarthritis: a large randomised multicentre trial. Ann Rheum Dis 2010;69:660-5. [Crossref] [PubMed]
- Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 Recommendations for the Use of Nonpharmacologic and Pharmacologic Therapies in Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res (Hoboken) 2012;64:465-74. [Crossref] [PubMed]
- Ochiai S, Watanabe A, Oda H, et al. Effectiveness of thermotherapy using a heat and steam generating sheet for cartilage in knee osteoarthritis. J Phys Ther Sci 2014;26:281-4. [Crossref] [PubMed]
- Schaser KD, Dish AC, Stover JF, et al. Prolonged superficial local cryotherapy attenuates microcirculatory impairment. Regional inflammation. And muscle necrosis after closed soft tissue injury in rats. Am J Sports Med 2007;35:93-102. [Crossref] [PubMed]
- Schaser KD, Stover JF, Melcher I, et al. Local cooling restores microciculatory hemodynamics after closed soft-tissue trauma in rats. J Trauma 2006;61:642-9. [Crossref] [PubMed]
- Saito N, Horiuchi H, Kobayashi S, et al. Continuous local cooling for pain relief following total hip arthroplasty. J Arthroplasty 2004;19:334-7. [Crossref] [PubMed]
- Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 2012;172:1444-53. [Crossref] [PubMed]
- Vickers AJ, Linde K. Acupuncture for chronic pain. JAMA 2014;311:955-6. [Crossref] [PubMed]
- Chen Z, Ma C, Xu L, et al. Laser Acupuncture for Patients with Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Placebo-Controlled Trials. Evid Based Complement Alternat Med 2019;2019:6703828 [Crossref] [PubMed]
- Li J, Li YX, Luo LJ, et al. The effectiveness and safety of acupuncture for knee osteoarthritis: An overview of systematic reviews. Medicine (Baltimore) 2019;98:e16301 [Crossref] [PubMed]
- Li S, Xie P, Liang Z, et al. Efficacy Comparison of Five Different Acupuncture Methods on Pain, Stiffness, and Function in Osteoarthritis of the Knee: A Network Meta-Analysis. Evid Based Complement Alternat Med 2018;2018:1638904 [Crossref] [PubMed]
- Choi TY, Lee MS, Kim JI, et al. Moxibustion for the treatment of osteoarthritis: An updated systematic review and meta-analysis. Maturitas 2017;100:33-48. [Crossref] [PubMed]
- DeSantana JM, Santana-Filho VJ, Guerra DR, et al. Hypoalgesic effect of the transcutaneous electrical nerve stimulation following inguinal herniorrhaphy: a randomized, controlled trial. J Pain 2008;9:623-9. [Crossref] [PubMed]
- Johnson MI, Jones G. Transcutaneous electrical nerve stimulation: current status of evidence. Pain Manag 2017;7:1-4. [Crossref] [PubMed]
- Johnson M. Transcutaneous Electrical Nerve Stimulation: Mechanisms, Clinical Application and Evidence. Rev Pain 2007;1:7-11. [Crossref] [PubMed]
- Wu Y, Zhang J, Li S. Clinical observation on treatment of knee osteoarthritis by warm needling method. Journal of Acupuncture and Tuina Science 2009;7:349-51. [Crossref]
- Fary RE, Carroll GJ, Briffa TG, et al. The effectiveness of pulsed electrical stimulation in the management of osteoarthritis of the knee: results of a double-blind, randomized, placebo controlled, repeated-measures trial. Arthritis Rheum 2011;63:1333-42. [Crossref] [PubMed]
- Zizic TM, Hoffman KC, Holt PA, et al. The treatment of osteoarthritis of the knee with pulsed electrical stimulation. J Rheumatol 1995;22:1757-61. [PubMed]
- Maffiuletti NA, Cometti G, Amiridis IG, et al. The effects of electromyostimulation training and basketball practice on muscle strength and jumping ability. Int J Sports Med 2000;21:437-43. [Crossref] [PubMed]
- de Oliveira Melo M, Aragão FA, Vaz MA. Neuromuscular electrical stimulation for muscle strengthening in elderly with knee osteoarthritis - a systematic review. Complement Ther Clin Pract 2013;19:27-31. [Crossref] [PubMed]
- Bruce-Brand RA, Walls RJ, Ong JC, et al. Effects of home-based resistance training and neuromuscular electrical stimulation in knee osteoarthritis: a randomized controlled trial. BMC Musculoskelet Disord 2012;13:118. [Crossref] [PubMed]
- Vaz MA, Baroni BM, Geremia JM, et al. Neuromuscular electrical stimulation (NMES) reduces structural and functional losses of quadriceps muscle and improves health status in patients with knee osteoarthritis. J Orthop Res 2013;31:511-6. [Crossref] [PubMed]
- Melo Mde O, Pompeo KD, Brodt GA, et al. Effects of neuromuscular electrical stimulation and low-level laser therapy on the muscle architecture and functional capacity in elderly patients with knee osteoarthritis: a randomized controlled trial. Clin Rehabil 2015;29:570-80. [Crossref] [PubMed]
- Melo MO, Pompeo KD, Baroni BM, et al. Effects of neuromuscular electrical stimulation and low-level laser therapy on neuromuscular parameters and health status in elderly women with knee osteoarthritis: A randomized trial. J Rehabil Med 2016;48:293-9. [Crossref] [PubMed]
- Laufer Y, Shtraker H, Elboim Gabyzon M. The effects of exercise and neuromuscular electrical stimulation in subjects with knee osteoarthritis: a 3-month follow-up study. Clin Interv Aging 2014;9:1153-61. [Crossref] [PubMed]
- Anders JJ, Lanzafame RJ, Arany PR. Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg 2015;33:183-4. [Crossref] [PubMed]
- Hamblin MR. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys 2017;4:337-61. [Crossref] [PubMed]
- Hegedus B, Viharos L, Gervain M, et al. The effect of low-level laser in knee osteoarthritis: a double-blind, randomized, placebo-controlled trial. Photomed Laser Surg 2009;27:577-84. [Crossref] [PubMed]
- Soleimanpour H, Gahramani K, Taheri R, et al. The effect of low-level laser therapy on knee osteoarthritis: prospective, descriptive study. Lasers Med Sci 2014;29:1695-700. [Crossref] [PubMed]
- Huang Z, Chen J, Ma J, et al. Effectiveness of low-level laser therapy in patients with knee osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage 2015;23:1437-44. [Crossref] [PubMed]
- Trock DH, Bollet AJ, Markoll R. The effect of pulsed electromagnetic fields in the treatment of osteoarthritis of the knee and cervical spine. Report of randomized, double blind, placebo controlled trials. J Rheumatol 1994;21:1903-11. [PubMed]
- Balbinot G, Schuch CP, Nascimento PSD, et al. Photobiomodulation Therapy Partially Restores Cartilage Integrity and Reduces Chronic Pain Behavior in a Rat Model of Osteoarthritis: Involvement of Spinal Glial Modulation. Cartilage 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Li S, Yu B, Zhou D, et al. Electromagnetic fields for treating osteoarthritis. Cochrane Database Syst Rev 2013;CD003523 [PubMed]
- Atamaz FC, Durmaz B, Baydar M, et al. Comparison of the efficacy of transcutaneous electrical nerve stimulation, interferential currents, and shortwave diathermy in knee osteoarthritis: a double-blind, randomized, controlled, multicenter study. Arch Phys Med Rehabil 2012;93:748-56. [Crossref] [PubMed]
- Nelson NL, Churilla JR. Massage Therapy for Pain and Function in Patients With Arthritis: A Systematic Review of Randomized Controlled Trials. Am J Phys Med Rehabil 2017;96:665-72. [Crossref] [PubMed]
- Battisti E, Piazza E, Rigato M, et al. Efficacy and safety of a musically modulated electromagnetic field (TAMMEF) in patients affected by knee osteoarthritis. Clin Exp Rheumatol 2004;22:568-72. [PubMed]
- Baghaei Roodsari R, Esteki A, Aminian G, et al. The effect of orthotic devices on knee adduction moment, pain and function in medial compartment knee osteoarthritis: a literature review. Disabil Rehabil Assist Technol 2017;12:441-9. [Crossref] [PubMed]
- Perlman AI, Ali A, Njike VY, et al. Massage therapy for osteoarthritis of the knee: a randomized dose-finding trial. PLoS One 2012;7:e30248 [Crossref] [PubMed]
- Mann WC, Hurren D, Tomita M. Assistive devices used by home-based elderly persons with arthritis. Am J Occup Ther 1995;49:810-20. [Crossref] [PubMed]
- Fang MA, Heiney C, Yentes JM, et al. Clinical and Spatiotemporal Gait Effects of Canes in Hip Osteoarthritis. PM R 2012;4:30-6. [Crossref] [PubMed]
- Jones A, Silva PG, Silva AC, et al. Impact of cane use on pain, function, general health and energy expenditure during gait in patients with knee osteoarthritis: a randomised controlled trial. Ann Rheum Dis 2012;71:172-9. [Crossref] [PubMed]
- Simonsen EB, Svendsen MB, Norreslet A, et al. Walking on high heels changes muscle activity and the dynamics of human walking significantly. J Appl Biomech 2012;28:20-8. [Crossref] [PubMed]
- Turpin KM, De VA, Apps AM, et al. Biomechanical and clinical outcomes with shock-absorbing insoles in patients with knee osteoarthritis: immediate effects and changes after 1 month of wear. Arch Phys Med Rehabil 2012;93:503-8. [Crossref] [PubMed]
- Raja K, Dewan N. Efficacy of knee braces and foot orthoses in conservative management of knee osteoarthritis: a systematic review. Am J Phys Med Rehabil 2011;90:247-62. [Crossref] [PubMed]
- Cheung RT, Chung RC, Ng GY. Efficacies of different external controls for excessive foot pronation: a meta-analysis. Br J Sports Med 2011;45:743-51. [Crossref] [PubMed]
- Kirkley A, Webster-Bogaert S, Litchfield R, et al. The effect of bracing on varus gonarthrosis. J Bone Joint Surg Am 1999;81:539-48. [Crossref] [PubMed]
- Thomas S, Browne H, Mobasheri A, et al. What is the evidence for a role for diet and nutrition in osteoarthritis? Rheumatology (Oxford) 2018;57:iv61-iv74. [Crossref] [PubMed]
- Messina OD, Vidal Wilman M, Vidal Neira LF. Nutrition, osteoarthritis and cartilage metabolism. Aging Clin Exp Res 2019;31:807-13. [Crossref] [PubMed]
- Grover AK, Samson SE. Benefits of antioxidant supplements for knee osteoarthritis: rationale and reality. Nutr J 2016;15:1. [Crossref] [PubMed]
- Nash RJ, Azantsa BK, Sharp H, et al. Effectiveness of Cucumis sativus extract versus glucosamine-chondroitin in the management of moderate osteoarthritis: a randomized controlled trial. Clin Interv Aging 2018;13:2119-26. [Crossref] [PubMed]
- Knott L, Avery NC, Hollander AP, et al. Regulation of osteoarthritis by omega-3 (n-3) polyunsaturated fatty acids in a naturally occurring model of disease. Osteoarthritis Cartilage 2011;19:1150-7. [Crossref] [PubMed]
- Rodriguez-Merchan EC. Topical therapies for knee osteoarthritis. Postgrad Med 2018;130:607-12. [Crossref] [PubMed]
- Cutolo M, Berenbaum F, Hochberg M, et al. Commentary on recent therapeutic guidelines for osteoarthritis. Semin Arthritis Rheum 2015;44:611-7. [Crossref] [PubMed]
- Machado GC, Maher CG, Ferreira PH, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ 2015;350:h1225. [Crossref] [PubMed]
- Roberts E, Delgado Nunes V, et al. Paracetamol: not as safe as we thought? A systematic literature review of observational studies. Ann Rheum Dis 2016;75:552-9. [Crossref] [PubMed]
- Baker K, Goggins J, Xie H, et al. A randomized crossover trial of a wedged insole for treatment of knee osteoarthritis. Arthritis Rheum 2007;56:1198-203. [Crossref] [PubMed]
- Kaye AD, Jones MR, Kaye AM, et al. Prescription Opioid Abuse in Chronic Pain: An Updated Review of Opioid Abuse Predictors and Strategies to Curb Opioid Abuse: Part 1. Pain Physician 2017;20:S93-109. [PubMed]
- Kaye AD, Jones MR, Kaye AM, et al. Prescription Opioid Abuse in Chronic Pain: An Updated Review of Opioid Abuse Predictors and Strategies to Curb Opioid Abuse (Part 2). Pain Physician 2017;20:S111-33. [PubMed]
- Maillefert JF, Hudry C, Baron G, et al. Laterally elevated wedged insoles in the treatment of medial knee osteoarthritis: a prospective randomized controlled study. Osteoarthritis Cartilage 2001;9:738-45. [Crossref] [PubMed]
- Pham T, Maillefert JF, Hudry C, et al. Laterally elevated wedged insoles in the treatment of medial knee osteoarthritis. A two-year prospective randomized controlled study. Osteoarthritis Cartilage 2004;12:46-55. [Crossref] [PubMed]
- Treatment of Osteoarthritis of the Knee (2nd edition). Available online: http://www.orthoguidelines.org/topic?id=1005
- McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 2014;22:363-88. [Crossref] [PubMed]
- Brown GA. AAOS clinical practice guideline: treatment of osteoarthritis of the knee: evidence-based guideline, 2nd edition. J Am Acad Orthop Surg 2013;21:577-9.
- Legré-Boyer V. Viscosupplementation: Techniques, indications, results. Orthop Traumatol Surg Res 2015;101:S101-8. [Crossref] [PubMed]
- Smith PA. Intra-articular Autologous Conditioned Plasma Injections Provide Safe and Efficacious Treatment for Knee Osteoarthritis: An FDA-Sanctioned, Randomized, Double-blind, Placebo-controlled Clinical Trial. Am J Sports Med 2016;44:884-91. [Crossref] [PubMed]
- Patel S, Dhillon MS, Aggarwal S, et al. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med 2013;41:356-64. [Crossref] [PubMed]
- Sheth U, Simunovic N, Klein G, et al. Efficacy of autologous platelet-rich plasma use for orthopaedic indications: a meta-analysis. J Bone Joint Surg Am 2012;94:298-307. [Crossref] [PubMed]
- Nelson AE, Allen KD, Golightly YM, et al. A systematic review of recommendations and guidelines for the management of osteoarthritis: The chronic osteoarthritis management initiative of the U.S. bone and joint initiative. Semin Arthritis Rheum 2014;43:701-12. [Crossref] [PubMed]
- Wei CC, Lin AB, Hung SC. Mesenchymal stem cells in regenerative medicine for musculoskeletal diseases: bench, bedside, and industry. Cell Transplant 2014;23:505-12. [Crossref] [PubMed]
- Castro-Manrreza ME, Montesinos JJ. Immunoregulation by mesenchymal stem cells: biological aspects and clinical applications. J Immunol Res 2015;2015:394917-20. [Crossref] [PubMed]
- Freitag J, Bates D, Boyd R, et al. Mesenchymal stem cell therapy in the treatment of osteoarthritis: reparative pathways, safety and efficacy - a review. BMC Musculoskelet Disord 2016;17:230. [Crossref] [PubMed]
- Saw KY, Anz A, Siew-Yoke JC, et al. Articular cartilage regeneration with autologous peripheral blood stem cells versus hyaluronic acid: a randomized controlled trial. Arthroscopy 2013;29:684-94. [Crossref] [PubMed]
- Vega A, Martín-Ferrero MA, Del CF, et al. Treatment of knee osteoarthritis with allogeneic bone marrow mesenchymal stem cells: A randomized controlled trial. Transplantation 2015;99:1681-90. [Crossref] [PubMed]
- Vangsness CT Jr, Farr J 2nd, Boyd J, et al. Adult human mesenchymal stem cells delivered via intra-articular injection to the knee following partial medial meniscectomy: a randomized, double-blind, controlled study. J Bone Joint Surg Am 2014;96:90-8. [Crossref] [PubMed]
- Caplan AI. Mesenchymal Stem Cells: Time to Change the Name! Stem Cells Transl Med 2017;6:1445-51. [Crossref] [PubMed]
- Reginster JY, Dudler J, Blicharski T, et al. Pharmaceutical-grade Chondroitin sulfate is as effective as celecoxib and superior to placebo in symptomatic knee osteoarthritis: the ChONdroitin versus CElecoxib versus Placebo Trial (CONCEPT). Ann Rheum Dis 2017;76:1537-43. [Crossref] [PubMed]
- Herrero-Beaumont G, Largo R. Osteoarthritis: Chondroitin sulfate - CONCEPT clear, uncertainties unchanged. Nat Rev Rheumatol 2017;13:576-7. [Crossref] [PubMed]
- Ekeland A, Nerhus TK, Dimmen S, et al. Good functional results following high tibial opening-wedge osteotomy of knees with medial osteoarthritis: A prospective study with a mean of 8.3years of follow-up. Knee 2017;24:380-9. [Crossref] [PubMed]
- Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. Br J Sports Med 2018;52:313. [Crossref] [PubMed]
Cite this article as: Shi D, Clement ND, Bhonde R, Ikegawa S, Mascarenhas VV, Di Matteo B, Indelli PF, Kourkoumelis N, Rodríguez-Merchán EC, Sheykhhasan M, Fu FH, Vaz MA, Kong J, Azantsa BGK, Ye C, Halabchi F, Cornish SM, Hausmann LRM, Campos ALS, Lopes de Jesus CC, Jorgensen C, Ilieva EM, Wang W, Martínez LV, Ahn H, Shirinsky IV, Cheung C, Knutsen G, Petersen W, Lane NE, Cai H, Xu W, Wu J, Lu J, Zhang Y, Jiang Q. Society for translational medicine-expert consensus on the treatment of osteoarthritis. Ann Joint 2019;4:49.