
Psychological interventions in the pain management after hip and knee arthroplasty: a mini review
Introduction
Joint arthroplasty is one of the most effective therapeutic methods for patients with severe osteoarthritis (OA), hip fragility fracture caused by osteoporosis, and osteonecrosis of the femoral head (1). Most of the pain or functional disability induced by these diseases can be improved by the surgery. But still some patients do not report amelioration of their performance after the arthroplasty surgery, although their radiologic findings are normal (2). The major cause for this abnormal phenomenon may be the persistent post-surgical pain, which results in the emotional upset and individual suffering (3). This chronic pain can last from 3 months to more than 1 year in about 20% patients, which has a negative impact on clinical outcomes (4,5). Apart from the persistent chronic pain, acute pain is another commonly anticipated problem after surgery. It will directly delay the healing process and increase the post-surgery morbidity (6). Moreover, acute pain is of great significance in the occurrence of chronic post-surgical pain (7,8). Thus, the management of post-surgical acute and chronic pain has a direct relationship with the outcomes of knee and hip arthroplasty.
However, the establishment of guidelines and standards for pain management is not easy. As a psychological experience, pain is induced by complex interactions between sensory-discriminative, motivational-affective, and cognitive-evaluative dimensions (9,10). But the causes for pain are not just psychological, age, surgical trauma, nerve damage, and surgery types are other risk factors that must be considered (3). The combination and interaction of these psychological and physical factors makes the interventions for reducing pain harder. When treated with analgesics, the patients have to suffer the risk of drug addiction due to the gradually diminishing pain-reducing efficacy. Besides, other side effects, like nausea, vomiting, and constipation limit the safe and effective doses (11,12). Fortunately, the psychological research on pain predictors helps medical staff to know how the pain symptom occurs and what methods may reduce it. Several studies have proved that the pain can be exacerbated and inhibited by the affective and cognitive variables, which are considered as consistent predictors of both acute pain and chronic pain (13). The level of pain that a patient suffers is closely related to the pain intensity, catastrophizing, and fear. Therefore, distraction, imagery, relaxation, and suggestion have been employed to alter the awareness of pain (14). Except the negative psychological variables, studies on positive psychological variables support that these factors can act as buffers or adaptive coping strategies for reducing pain (15,16). Based on these conditions, psychological interventions for pain management are taken as potential methods in clinical nursing.
The routine psychological interventions are not included in general rehabilitation principles after knee or hip arthroplasty. Some psychological coping strategies have been introduced to minimize the effects of pain, but there are no particular guidelines to follow to reduce pain notably. Because the psychological interventions are different based on the surgery types, technique mechanism, and pain-specific information (17). But considering the evidence of psychological interventions in pain relieving, it is logical to involve this method in facilitating recovery from joint arthroplasty. Herein, we review the predictors for post-surgical pain, and the psychological interventions which can affect the pain perception, rehabilitation, and other treatment outcomes after arthroplasty. We expect to define the effective intervention methods in post-surgical pain management.
Predictors for post-surgical pain
The post-surgical pain can be divided into acute and chronic pain according to a specific timeline. The pain that occurs suddenly after surgery and lasts less than 3 months is considered as acute pain, and the ongoing or recurrent pain lasting for more than 3 months is considered as chronic pain (18). Thus, the predictors are respectively elaborated depending on the type of pain.
Acute pain
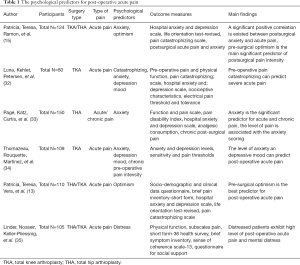
The postoperative acute pain is related to age, preoperative chronic pain, epidural analgesia, preoperative anxiety, and depression (19). Among these factors, young age, preoperative moderate to intense pain, preoperative chronic pain, anxiety, and depressive mood demonstrate higher risk for reporting acute post-surgical pain. Compared with male, female patients are more likely to suffer acute pain after arthroplasty (15). They also report higher levels in anxiety and depression. On the other hand, male patients usually represent higher levels of optimism and lower levels of pain catastrophizing (20). These four psychological variables (anxiety, depressive mood, optimism, and catastrophizing) correlate significantly with acute post-surgical pain. Optimism correlates inversely with postoperative acute pain, and the other three variables have positive relationship with this symptom. The difference in psychological status is the major cause for the variational pain intensity in male and female. Patients with optimism mood will confront surgery and the acute pain more positively. They generally pay less attention to pain stimuli, but more attentive to their hopeful medium-term life, which helps them to go through the short-term period pain after surgery (21,22). Nevertheless, patients who have a more negative emotion commonly report a higher risk to bear acute post-surgical pain. Because these emotions can induce high pain sensitivity, pessimistic prospect of the surgery, and maladaptive pain-coping strategies (23,24). Thus, we can conclude that the arthroplasty outcomes are related with the patients’ psychological status.
Except the four variables mentioned above, several other psychological factors have been assessed in the post-surgical pain management. The distress, response expectancy, and psychological robustness have impact on acute pain either (25). The distress mood is similar to depression and pain catastrophizing. Patients having this feeling may angry or upset, and directly influence the surgical outcomes (26). The preoperative response expectancy on pain experience can predict the intensity variation of acute pain immediately after surgery. The action of psychological robustness is like optimism, and it has negative relationship with pain at rest and movement evoked pain (27). Besides, various pain thresholds are evaluated in different surgeries to predict acute postoperative pain, including heat, electrical stimulation, pressure, supra-threshold cold and heat, noxious stimuli, and pain tolerance (28-31). These static psychological tests can predict the acute pain in some extent, but the sensitivity is not enough to estimate pain incidence and intensity (31). Due to the distinction of severity of symptoms, preoperative waiting period, surgery types, and surgeons, it is necessary to make individual psychological pain test based on the different preoperative conditions. The included studies are shown in Table 1.
Full table
Chronic pain
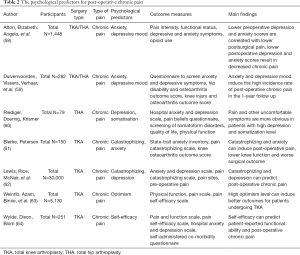
Unlike acute post-surgical pain, the occurrence of chronic pain is complex and the predictors are more complicated. This persistent pain symptom usually comes from the long-period preoperative suffering and transition from acute postoperative pain. Hence, several predictors for chronic pain are similar to acute pain, like age and some psychological variables. Patients with higher preoperative pain scores and older age are susceptible population to suffer postoperative chronic pain (36). Additionally, the severity of OA and the time these patients spend on waiting for the arthroplasty are positively correlated with the intensity of chronic pain (37,38). Especially the overlong waiting time between first visit and surgical intervention, it can induce the postoperative chronic pain and the worse function recovery (39). The low quality of life during the long-term waiting and the urgent demand of relieving severe symptoms may cause negative emotion, like anxiety, depression, and anger, which are high risk factors for postoperative chronic pain (38). Except the variables mentioned above, other social factors can predict the pain symptom with low sensitivity, like education level, living alone or with partner, and household income level.
Mechanical factors also play vital role in the occurrence of postoperative chronic pain. Several modifications and adaptations will happen after the prostheses are implanted (36). The reaction type and extent depend on the characteristics of prostheses, the quality of host tissue, and the biomechanical conditions (40,41). The shear stress and wear debris production can induce bone loss, osteolysis, and inflammation surrounding the prosthetic implant, leading to the aseptic loosening of the implant and simultaneous chronic pain (42). Fortunately, these postoperative physiological and pathological variables can be detected by radiography examination, like X-ray and dual-energy X-ray absorptiometry (DXA). A suitable prosthetic implant and revision surgery can solve most of the problems and notably relieve the postoperative pain.
However, the psychological predictors are more intricate. Some of them are same as the predict factors of acute pain, including depression, distress, anxiety, and pain catastrophizing. The psychological distress and depression result in worse symptoms at baseline, and they are more likely to cause worse pain scores before and after surgery (43). The duration of pain symptom can be as long as 1 to 2 years (44). And the intensive preoperative anxiety is another risk for the postoperative emotional disturbances and may also cause chronic pain with unclear predisposition, leading to unsatisfying surgical outcomes and extended healing process (45). Moreover, the fear of recurrent pain or preoperative injury causes exaggerated negative postoperative psychological response to pain or the anticipation of pain (46). According to the fear-avoidance model of pain, the persistent fear-avoidance behavior is correlated to worse postoperative pain and disability due to the positive regulation mechanism between pain catastrophizing and pain symptom (47,48). Meanwhile, patients with improvements in these negative emotions usually lead to greater improvements in pain scores, indicating that the mental status is closely related to the postoperative chronic pain symptom (49,50).
Optimism, self-efficacy and relevant psychological mood have negative correlation with the incidence of chronic pain, at the same time, they have positive influence on rehabilitation quality and surgical outcomes (51). The self-efficacy theory has proved that higher scores in self-confidence, optimism, and motivation lead to better improvement of symptoms after surgery (52). Patients with these emotions trend to focus on rehabilitation and home exercise adherence rather than worry about surgical trauma or the recurrent pain (53,54). The sense of coherence is another inverse predictor for chronic pain. When patients suffer from OA or the related operation, weak sense of coherence can induce more severe disability in physical and mental dimensions (55). Strong sense of coherence brings comprehensible, manageable, and meaningful feelings from the environment to patients (56). They will have effective coping strategies to decrease the level of anxiety and depression, displaying the low risk of post-surgical chronic pain (57).
We can conclude that the pain predictors induced by physical operation can be tested and corrected precisely. But the symptoms induced by social aspects or psychological mood are difficult to quantify, which hampers the pain management after arthroplasty. Therefore, the preoperative and postoperative psychological treatment is necessary and effective. The included studies are shown in Table 2.
Full table
Psychological interventions
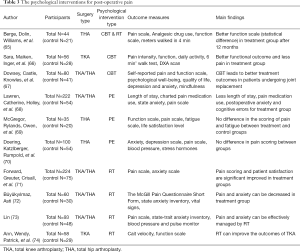
The most commonly used psychological interventions are cognitive behavior therapy (CBT), psychoeducation (PE), and relaxation therapy (RT). We summarized these contents and listed the application methods in this part. The included studies are shown in Table 3.
Full table
CBT
CBT is the first-line psychosocial treatment for patients before and after arthroplasty. This theory is developed based on the studies of Beck and Ellis, and aims to help people with psychological dysfunctional symptoms (75,76). For patients who are undergoing arthroplasty, the ABC model (Activating events-Beliefs-Consequences) is crucial in the pain relief (77). Briefly, the long term preoperative severe symptoms and pain after surgery are activating event to patients. The event will interact with the negative or irrational belief to make patients misunderstand that there is no pain in the successful surgery, which is actually impossible for any types of surgery (78). Finally, a maladaptive behavior or cognitive consequence occurs, and they feel pain and doubt the effect of arthroplasty. The deepening doubt and depression moods make them feel that the pain symptom always exists and will last forever (78,79). The knowledge of CBT is a helpful guide for patients to find appropriate cognitive and consequently adaptive behavior to cope with pain. Lots of studies have proved that CBT is effective for solving pain or pain related problems in patients from young age to elder (80,81).
According to the basic principles of CBT, the pain itself is not the core if we want to reduce the pain symptoms (82). We must focus on the interpretation of pain, helping patients to know that how the pain occurs and what they will suffer postoperatively. The changing of their thoughts about the occurrence of pain and the cognition of surgery is helpful to correct their behavioral consequences (83). Meanwhile, the positive behaviors also have powerfully positive influence on their perception of pain. The active exercise promotes fast recovery of functions, improves the surgical outcomes, and relieves the pain symptoms. A positive feedback relationship exists in the pain cognition and response behavior. Another principle is here-and-now, meaning that it is usually more fruitful to focus on current processes rather than the past (84). Telling the patients to feel the functional improvement after daily exercise instead of feeling anxious about the pain they suffered preoperative or the pain they may suffer during the exercise. More importantly, patients have to see that the pain is not a single issue as it comes from the interactions with thoughts, emotions, behavior, physiology, and environment (10). Although it is difficult for doctors and nurses to consider all these factors systematically, the more factors we take in, the better pain-reducing effect we will obtain.
For clinical application, few standardized CBT protocol is widely accepted and it is variable in number of sessions and specific techniques (82). It is commonly used by the combination of patients’ education and practice (65). The occurrence mechanism of OA, the process of arthroplasty, the anatomy of hip and knee, the thoughts and feelings about pain, the cognitive methods, and other information about pain and surgery are suitable for education (85). Although the education contents are distinguishing, almost all of the researchers reported notable improvement in functional recovery and pain relief after total hip arthroplasty (THA) and total knee arthroplasty (TKA) (65,86,87).
PE
PE is regarded as a simple therapeutic method compared with CBT, and it is often the part of CBT (78). Different from the CBT which aims to change patients’ belief and the related emotion or behavior, PE focuses on the information given to the patients (88). Patients who are enrolled into PE program will receive advice and suggestions on how to deal with pain symptoms before and after surgery. This psychological therapeutic method usually does not require any highly developed theoretical background for both therapists and patients, indicating that it is easy to employ in clinical nursing and an important add-on to pharmacological treatment (89). Based on this condition, PE is widely used in the management of inpatients, including education for hospitalization and preoperative conversation. The advantage of this method is the improvement in the care quality perceived by the patients, the better therapeutic alliance, and the better pharmacological adherence (90). It provides a therapeutic alliance between doctors and patients according to collaboration, information, and trust (91).
The mechanism of action of PE can be divided into three levels (90). The first level is the elemental mechanism. It helps patients to be aware of the pain symptom, improves the treatment adherence, and facilitates early diagnosis of other pain related symptoms. The second level is the secondary mechanism. According to the awareness of first level, therapists help patients to control their emotion, avoid anxiety, depression, and distress, and alleviate the effect of pain catastrophizing. The third level is the place to set desirable objectives. Patients in this level generally meet the fits of the first two levels. They are told developed knowledge about the pain, and know how to cope with the psycho-social consequences induced by the postoperative pain. The surgical outcomes, quality of life, and rehabilitation satisfaction are notably improved (88,92,93).
Several classical PE theories are introduced in clinical practice, including ecological systems theory, cognitive-behavioral theory, learning theory, group practice models, stress and coping models, social support models, and narrative approaches (94-96). These models release the postoperative pain symptoms through providing framework for assessing/helping patients to know their diseases, reducing isolation, allowing adaptive coping strategies with pain, recognizing personal strengths, and generating psycho-growth (92,97,98). However, this intervention method cannot be used alone to treat the pain symptoms due to the special condition in THA and TKA. The effectiveness of surgical trauma and psychological factors are usually very strong. Simply watching video, having conversation, or reading books are difficult to reverse the strong negative factors. Two RCT studies demonstrated that PE was insufficient to change behavior or improve surgical outcomes alone (69,70). Combination of PE with other psychological or physical interventions is a better option for the clinical application for postoperative pain management.
RT
RT is a special psychological intervention. It uses simple techniques to help patients to reduce physical and psychological discomfortable feelings, finally achieving a state of relaxation both physically and mentally (99). This technique can improve the negative effects caused by stress, disease, and surgery through some skills, like controlled breathing, focused muscle relaxation, and postural awareness and management (100). During the process of finishing these exercises, the preoperative anxiety and postoperative pain will be reduced in some extent (101). Based on the theory of Benson, a particular brain wave pattern, named alpha waves, will present during relaxation process, and these brain waves can make people feel well-being and happiness (102). In addition to changing the psychological mood, RT can induce some physiological reactions which are helpful to release anxiety and pain, including decreased oxygen consumption, carbon dioxide elimination, blood pressure, heart and respiratory rate, norepinephrine responsivity, increased heart rate variability, and alterations in cortical and subcortical brain regions (103-106).
Although techniques in RT are different, several common principles should be followed before this intervention (102). The first one is the appropriate surrounding environment (107). The inpatient ward is not suitable for relaxation as the noisy and privacy-free environment is hard for patients to focus on the exercise. An independent treatment room for one or two patients may be useful to realize the mental and physical relaxation before and after surgery. The second one is the personal emotion (108). Patients with severe acute pain symptoms or uncomfortable clothes are not the best candidates for RT. The psychological force and strained moods have negative influence on relaxation. Thus, participants must release in the exercise, indicating that a detailed psychological education is necessary to improve their treatment adherence. The last one is the treatment time (109). Because of the physiological reactions induced by RT, it is inappropriate to take relaxation intervention after meal or before sleep.
For the clinical application, meditation, yoga, Tai Chi, progressive muscle relaxation, biofeedback, and breathing exercises are the commonly used methods (110). Moreover, combination with guided imagery is another normal option for the clinical application of RT. After the patients are relaxed, images of relaxation or comforting place can help relieve the specific symptoms, such as pain (111,112). Other relaxation techniques, including hand and foot ‘‘M’’ technique and soothing biorhythmic music, are applicable nondrug intervention with no side effects (113,114). These methods can decrease the postoperative anxiety and pain levels, but some studies proved that the effect was not significant, suggesting that the evidence was encouraging but not conclusive (115). Like the PE, using relaxation alone may be not sufficient for improving the postoperative pain symptoms (78). It can complement analgesics or other nondrug interventions to improve the postoperative pain management in THA and TKA patients (73).
Conclusions
The joint arthroplasty is different from other types of surgeries. Patients who are willing to bear this surgery usually suffer long-term low quality of life due to the joint pain, activity limitation, and disability. These symptoms may induce complex psychological complications, including anxiety, fear, depression, and anger. All of these mental emotions are high risks for the occurrence of postoperative acute pain and chronic pain. Unfortunately, pharmaceutical and physical treatment is useless to most of the mental symptoms. But a few systematical psychological interventions are employed in the clinical nursing and rehabilitation procedures. We summarized some commonly used psychological interventions for the application and efficacy of pain management in the review. The CBT has been proved to have the best postoperative pain-reducing effect, and it can help patients to establish adaptive coping strategies on both mind and behavior. The PE and RT are insufficient when they are used alone, but they can act as the vital supplementary aids for other drug or nondrug interventions. We hope this review can help medical staff more comprehensively understand the generation mechanism of pain induced by joint arthroplasty and establish diversified psychological interventions for patients who are suffering the postoperative pain.
Acknowledgments
Funding: This study was supported by the Postgraduate Research & Practice Innovation Program of Jiangsu Province (SJKY19_0061), and Nanjing Science and Technology Development Project (201803026).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.12.06). QJ serves as an Editor-in-Chief of Annals of Joint from Mar 2013 to Feb 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Räsänen P, Paavolainen P, Sintonen H, et al. Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop 2007;78:108-15. [Crossref] [PubMed]
- Wylde V, Hewlett S, Learmonth ID, et al. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain 2011;152:566-72. [Crossref] [PubMed]
- Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet 2006;367:1618-25. [Crossref] [PubMed]
- O’Brien S, Bennett D, Doran E, et al. Comparison of hip and knee arthroplasty outcomes at early and intermediate follow-up. Orthopedics 2009;32:168. [PubMed]
- Baker PN, van der Meulen JH, Lewsey J, et al. The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br 2007;89:893-900. [Crossref] [PubMed]
- Rosen M. 2011--The global year against acute pain. Anaesth Intensive Care 2011;39:505. [PubMed]
- Macintyre P, Schug S, Scott D, et al. APM: SE working group of the Australian and New Zealand college of anaesthetists and faculty of pain medicine. Acute Pain Management: Scientific Evidence 2010;3:9-12.
- Schug SA, Palmer GM, Scott DA, et al. Acute pain management: scientific evidence, fourth edition, 2015. Med J Aust 2016;204:315-7.
- Melzack R. From the gate to the neuromatrix. Pain 1999;82:S121-6. [Crossref] [PubMed]
- Loeser JD, Melzack R. Pain: an overview. Lancet 1999;353:1607-9. [Crossref] [PubMed]
- Kokki H. Current management of pediatric postoperative pain. Expert Rev Neurother 2004;4:295-306. [Crossref] [PubMed]
- Niesters M, Overdyk F, Smith T, et al. Opioid-induced respiratory depression in paediatrics: a review of case reports. Br J Anaesth 2013;110:175-82. [Crossref] [PubMed]
- Pinto PR, McIntyre T, Araújo-Soares V, et al. Differential predictors of acute post-surgical pain intensity after abdominal hysterectomy and major joint arthroplasty. Ann Behav Med 2015;49:384-97. [Crossref] [PubMed]
- Turk DC, Gatchel RJ. Psychological approaches to pain management: A practitioner's handbook. Guilford Publications, 2018.
- Pinto PR, McIntyre T, Ferrero R, et al. Predictors of acute postsurgical pain and anxiety following primary total hip and knee arthroplasty. J Pain 2013;14:502-15. [Crossref] [PubMed]
- Peters ML, Sommer M, de Rijke JM, et al. Somatic and psychologic predictors of long-term unfavorable outcome after surgical intervention. Ann Surg 2007;245:487. [Crossref] [PubMed]
- Davidson F, Snow S, Hayden JA, et al. Psychological interventions in managing postoperative pain in children: a systematic review. Pain 2016;157:1872-86. [Crossref] [PubMed]
- Relieving Pain S SL. in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Mil Med 2016;181:397-9. [Crossref] [PubMed]
- Caumo W, Schmidt A, Schneider C, et al. Preoperative predictors of moderate to intense acute postoperative pain in patients undergoing abdominal surgery. Acta Anaesthesiologica Scandinavica 2002;46:1265-71. [Crossref] [PubMed]
- Kalkman CJ, Visser K, Moen J, et al. Preoperative prediction of severe postoperative pain. Pain 2003;105:415-23. [Crossref] [PubMed]
- DeSantis C, Ma J, Bryan L, et al. Breast cancer statistics, 2013. CA Cancer J Clin 2014;64:52-62. [Crossref] [PubMed]
- Baudic S, Jayr C, Albi-Feldzer A, et al. Effect of Alexithymia and Emotional Repression on Postsurgical Pain in Women With Breast Cancer: A Prospective Longitudinal 12-Month Study. J Pain 2016;17:90-100. [Crossref] [PubMed]
- Carr E, Brockbank K, Allen S, et al. Patterns and frequency of anxiety in women undergoing gynaecological surgery. J Clin Nurs 2006;15:341-52. [Crossref] [PubMed]
- McWilliams LA, Goodwin RD, Cox BJ. Depression and anxiety associated with three pain conditions: results from a nationally representative sample. Pain 2004;111:77-83. [Crossref] [PubMed]
- McCowat M, Fleming L, Vibholm J, et al. The Psychological Predictors of Acute and Chronic Pain in Women Following Breast Cancer Surgery: A Systematic Review. Clin J Pain 2019;35:261-71. [Crossref] [PubMed]
- Utrillas-Compaired A, De la Torre-Escuredo BJ, Tebar-Martinez AJ, et al. Does preoperative psychologic distress influence pain, function, and quality of life after TKA? Clin Orthop Relat Res 2014;472:2457-65. [PubMed]
- Brander VA, Stulberg SD, Adams AD, et al. Predicting total knee replacement pain: a prospective, observational study. Clin Orthop Relat Res 2003;27-36. [Crossref] [PubMed]
- Bisgaard T, Klarskov B, Rosenberg J, et al. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain 2001;90:261-9. [Crossref] [PubMed]
- Werner MU, Duun P, Kehlet H. Prediction of postoperative pain by preoperative nociceptive responses to heat stimulation. Anesthesiology 2004;100:115-9; discussion 5A.
- Aasvang EK, Hansen JB, Kehlet H. Can preoperative electrical nociceptive stimulation predict acute pain after groin herniotomy? J Pain 2008;9:940-4. [Crossref] [PubMed]
- Granot M. Can we predict persistent postoperative pain by testing preoperative experimental pain? Curr Opin Anaesthesiol 2009;22:425-30. [Crossref] [PubMed]
- Luna IE, Kehlet H, Petersen MA, et al. Clinical, nociceptive and psychological profiling to predict acute pain after total knee arthroplasty. Acta Anaesthesiol Scand 2017;61:676-87. [Crossref] [PubMed]
- Pagé MG, Katz J, Curtis K, et al. Acute pain trajectories and the persistence of post-surgical pain: a longitudinal study after total hip arthroplasty. J Anesth 2016;30:568-77. [Crossref] [PubMed]
- Thomazeau J, Rouquette A, Martinez V, et al. Acute pain Factors predictive of post-operative pain and opioid requirement in multimodal analgesia following knee replacement. Eur J Pain 2016;20:822-32. [Crossref] [PubMed]
- Lindner M, Nosseir O, Keller-Pliessnig A, et al. Psychosocial predictors for outcome after total joint arthroplasty: a prospective comparison of hip and knee arthroplasty. BMC Musculoskelet Disord 2018;19:159. [Crossref] [PubMed]
- Piscitelli P, Iolascon G, Innocenti M, et al. Painful prosthesis: approaching the patient with persistent pain following total hip and knee arthroplasty. Clin Cases Miner Bone Metab 2013;10:97-110. [PubMed]
- Ostendorf M, Buskens E, van Stel H, et al. Waiting for total hip arthroplasty: avoidable loss in quality time and preventable deterioration. J Arthroplasty 2004;19:302-9. [Crossref] [PubMed]
- Quintana JM, Escobar A, Arostegui I, et al. Health-related quality of life and appropriateness of knee or hip joint replacement. Arch Intern Med 2006;166:220-6. [Crossref] [PubMed]
- McHugh GA, Luker KA, Campbell M, et al. Pain, physical functioning and quality of life of individuals awaiting total joint replacement: a longitudinal study. J Eval Clin Pract 2008;14:19-26. [Crossref] [PubMed]
- Hing CB, Young DA, Dalziel RE, et al. Narrowing of the neck in resurfacing arthroplasty of the hip: a radiological study. J Bone Joint Surg Br 2007;89:1019-24. [Crossref] [PubMed]
- Frost HM A. 2003 update of bone physiology and Wolff's Law for clinicians. Angle Orthod 2004;74:3-15. [PubMed]
- Iolascon G, Di Pietro G, Capaldo A, et al. Periprosthetic bone density as outcome of therapeutic response. Clin Cases Miner Bone Metab 2010;7:27-31. [PubMed]
- Hirschmann MT, Testa E, Amsler F, et al. The unhappy total knee arthroplasty (TKA) patient: higher WOMAC and lower KSS in depressed patients prior and after TKA. Knee Surg Sports Traumatol Arthrosc 2013;21:2405-11. [Crossref] [PubMed]
- Lavernia CJ, Alcerro JC, Brooks LG, et al. Mental health and outcomes in primary total joint arthroplasty. J Arthroplasty 2012;27:1276-82. [Crossref] [PubMed]
- Caracciolo B, Giaquinto S. Self-perceived distress and self-perceived functional recovery after recent total hip and knee arthroplasty. Arch Gerontol Geriatr 2005;41:177-81. [Crossref] [PubMed]
- Leeuw M, Goossens ME, Linton SJ, et al. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med 2007;30:77-94. [Crossref] [PubMed]
- Lethem J, Slade PD, Troup JD, et al. Outline of a Fear-Avoidance Model of exaggerated pain perception--I. Behav Res Ther 1983;21:401-8. [Crossref] [PubMed]
- Archer KR, Phelps KD, Seebach CL, et al. Comparative study of short forms of the Tampa Scale for Kinesiophobia: fear of movement in a surgical spine population. Arch Phys Med Rehabil 2012;93:1460-2. [Crossref] [PubMed]
- Blackburn J, Qureshi A, Amirfeyz R, et al. Does preoperative anxiety and depression predict satisfaction after total knee replacement? Knee 2012;19:522-4. [Crossref] [PubMed]
- Flanigan DC, Everhart JS, Glassman AH. Psychological Factors Affecting Rehabilitation and Outcomes Following Elective Orthopaedic Surgery. J Am Acad Orthop Surg 2015;23:563-70. [Crossref] [PubMed]
- Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc 2015;23:752-62. [Crossref] [PubMed]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. [Crossref] [PubMed]
- Altmaier EM, Russell DW, Kao CF, et al. Role of self-efficacy in rehabilitation outcome among chronic low back pain patients. Journal of counseling psychology 1993;40:335. [Crossref]
- Desharnais R, Bouillon J, Godin G. Self-efficacy and outcome expectations as determinants of exercise adherence. Psychol Rep 1986;59:1155-9. [Crossref]
- Badura-Brzoza K, Zajac P, Brzoza Z, et al. Psychological and psychiatric factors related to health-related quality of life after total hip replacement–preliminary report. Eur Psychiatry 2009;24:119-24. [Crossref] [PubMed]
- Antonovsky A. The life cycle, mental health and the sense of coherence. Isr J Psychiatry Relat Sci 1985;22:273-80. [PubMed]
- Hassmén P, Koivula N, Uutela A. Physical exercise and psychological well-being: a population study in Finland. Prev Med 2000;30:17-25. [Crossref] [PubMed]
- Hassett AL, Marshall E, Bailey AM, et al. Changes in Anxiety and Depression Are Mediated by Changes in Pain Severity in Patients Undergoing Lower-Extremity Total Joint Arthroplasty. Reg Anesth Pain Med 2018;43:14-8. [Crossref] [PubMed]
- Duivenvoorden T, Vissers MM, Verhaar JA, et al. Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthritis Cartilage 2013;21:1834-40. [Crossref] [PubMed]
- Riediger W, Doering S, Krismer M. Depression and somatisation influence the outcome of total hip replacement. Int Orthop 2010;34:13-8. [Crossref] [PubMed]
- Bierke S, Petersen W. Influence of anxiety and pain catastrophizing on the course of pain within the first year after uncomplicated total knee replacement: a prospective study. Arch Orthop Trauma Surg 2017;137:1735-42. [Crossref] [PubMed]
- Lewis GN, Rice DA, McNair PJ, et al. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth 2015;114:551-61. [Crossref] [PubMed]
- Weinrib AZ, Azam MA, Birnie KA, et al. The psychology of chronic post-surgical pain: new frontiers in risk factor identification, prevention and management. Br J Pain 2017;11:169-77. [Crossref] [PubMed]
- Wylde V, Dixon S, Blom AW. The role of preoperative self-efficacy in predicting outcome after total knee replacement. Musculoskeletal Care 2012;10:110-8. [Crossref] [PubMed]
- Berge DJ, Dolin SJ, Williams AC, et al. Pre-operative and post-operative effect of a pain management programme prior to total hip replacement: a randomized controlled trial. Pain 2004;110:33-9. [Crossref] [PubMed]
- Birch S, Stilling M, Mechlenburg I, et al. Effectiveness of a physiotherapist delivered cognitive-behavioral patient education for patients who undergoes operation for total knee arthroplasty: a protocol of a randomized controlled trial. BMC Musculoskelet Disord 2017;18:116. [Crossref] [PubMed]
- Dowsey MM, Castle DJ, Knowles SR, et al. The effect of mindfulness training prior to total joint arthroplasty on post-operative pain and physical function: study protocol for a randomised controlled trial. Trials 2014;15:208. [Crossref] [PubMed]
- Daltroy LH, Morlino CI, Eaton HM, et al. Preoperative education for total hip and knee replacement patients. Arthritis Care Res 1998;11:469-78. [Crossref] [PubMed]
- McGregor AH, Rylands H, Owen A, et al. Does preoperative hip rehabilitation advice improve recovery and patient satisfaction? J Arthroplasty 2004;19:464-8. [Crossref] [PubMed]
- Doering S, Katzlberger F, Rumpold G, et al. Videotape preparation of patients before hip replacement surgery reduces stress. Psychosom Med 2000;62:365-73. [Crossref] [PubMed]
- Forward JB, Greuter NE, Crisall SJ, et al. Effect of Structured Touch and Guided Imagery for Pain and Anxiety in Elective Joint Replacement Patients--A Randomized Controlled Trial: M-TIJRP. Perm J 2015;19:18-28. [PubMed]
- Büyükyılmaz F, Asti T. The effect of relaxation techniques and back massage on pain and anxiety in Turkish total hip or knee arthroplasty patients. Pain Manag Nurs 2013;14:143-54. [Crossref] [PubMed]
- Lin PC. An evaluation of the effectiveness of relaxation therapy for patients receiving joint replacement surgery. J Clin Nurs 2012;21:601-8. [Crossref] [PubMed]
- Jacobson AF, Umberger WA, Palmieri PA, et al. Guided Imagery for Total Knee Replacement: A Randomized, Placebo-Controlled Pilot Study. J Altern Complement Med 2016;22:563-75. [Crossref] [PubMed]
- Beck AT. Cognitive therapy: Nature and relation to behavior therapy. J Psychother Pract Res 1993;2:342-56. [PubMed]
- Ellis A. Reason and emotion in psychotherapy. 1962.
- Ellis A. The revised ABC's of rational-emotive therapy (RET). J Ration Emot Cogn Behav Ther 1991;9:139-72. [Crossref]
- Bay S, Kuster L, McLean N, et al. A systematic review of psychological interventions in total hip and knee arthroplasty. BMC Musculoskelet Disord 2018;19:201. [Crossref] [PubMed]
- O'Connor KP. A constructionist clinical psychology for cognitive behaviour therapy. Routledge, 2015.
- Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev 2012;11:CD007407 [PubMed]
- Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive-behavioral therapy for chronic pain. Pain 2007;127:276-86. [Crossref] [PubMed]
- Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol 2014;69:153-66. [Crossref] [PubMed]
- Kennerley H, Kirk J, Westbrook D. An introduction to cognitive behaviour therapy: Skills and applications. Sage 2016;
- Robertson D. The philosophy of cognitive-behavioural therapy (CBT): Stoic philosophy as rational and cognitive psychotherapy. Routledge, 2018.
- Thorn BE, Burns JW. Common and specific treatment mechanisms in psychosocial pain interventions: the need for a new research agenda. Pain 2011;152:705-6. [Crossref] [PubMed]
- Wetherell JL, Afari N, Rutledge T, et al. A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain 2011;152:2098-107. [Crossref] [PubMed]
- Levy RL, Langer SL, Walker LS, et al. Cognitive-behavioral therapy for children with functional abdominal pain and their parents decreases pain and other symptoms. Am J Gastroenterol 2010;105:946-56. [Crossref] [PubMed]
- Lukens EP, McFarlane WR. Psychoeducation as Evidence-Based Practice: Considerations for Practice, Research, and Policy. Brief Treatment & Crisis Intervention 2004;4.
- Colom F. Keeping therapies simple: psychoeducation in the prevention of relapse in affective disorders. Br J Psychiatry 2011;198:338-40. [Crossref] [PubMed]
- Colom F, Vieta E. Psychoeducation manual for bipolar disorder. Cambridge University Press, 2006.
- Hayes R, Gantt A. Patient psychoeducation: the therapeutic use of knowledge for the mentally ill. Soc Work Health Care 1992;17:53-67. [Crossref] [PubMed]
- LeFort SM, Gray-Donald K, Rowat KM, et al. Randomized controlled trial of a community-based psychoeducation program for the self-management of chronic pain. Pain 1998;74:297-306. [Crossref] [PubMed]
- McGillion M, Watt-Watson J, Kim J, et al. A systematic review of psychoeducational intervention trials for the management of chronic stable angina. J Nurs Manag 2004;12:174-82. [Crossref] [PubMed]
- Anderson CM, Reiss DJ, Hogarty GE. Schizophrenia and the family: A practitioner's guide to psychoeducation and management. Guilford Press, 1986.
- Lukens EP, Thorning H, Herman DB. Family psychoeducation in schizophrenia: Emerging themes and challenges. Journal of Psychiatric Practice 1999;5:314-25. [Crossref]
- McFarlane WR, Dixon L, Lukens E, et al. Family psychoeducation and schizophrenia: a review of the literature. J Marital Fam Ther 2003;29:223-45. [Crossref] [PubMed]
- Penninx BW, van Tilburg T, Kriegsman DM, et al. Social network, social support, and loneliness in older persons with different chronic diseases. J Aging Health 1999;11:151-68. [Crossref] [PubMed]
- McGillion M, Watt-Watson J, LeFort S, et al. Positive shifts in the perceived meaning of cardiac pain following a psychoeducation program for chronic stable angina. Can J Nurs Res 2007;39:48-65. [PubMed]
- Willhelm AR, Andretta I, Ungaretti MS. Importance of relaxation techniques in cognitive therapy for anxiety. Contextos Clínicos 2015;8:79.
- van Dixhoorn JJ, Duivenvoorden HJ. Effect of relaxation therapy on cardiac events after myocardial infarction: a 5-year follow-up study. J Cardiopulm Rehabil 1999;19:178-85. [Crossref] [PubMed]
- Ghafari S, Ahmadi F, Nabavi M, et al. Effectiveness of applying progressive muscle relaxation technique on quality of life of patients with multiple sclerosis. J Clin Nurs 2009;18:2171-9. [Crossref] [PubMed]
- Payne RA, Donaghy M. Relaxation techniques E-book: a practical handbook for the health care professional. Elsevier Health Sciences, 2010.
- Bhasin MK, Dusek JA, Chang B-H, et al. Relaxation response induces temporal transcriptome changes in energy metabolism, insulin secretion and inflammatory pathways. PLoS One 2013;8:e62817 [Crossref] [PubMed]
- Dusek JA, Chang BH, Zaki J, et al. Association between oxygen consumption and nitric oxide production during the relaxation response. Med Sci Monit 2006;12:CR1-10. [PubMed]
- Wallace RK, Benson H, Wilson AF. A wakeful hypometabolic physiologic state. Am J Physiol 1971;221:795-9. [Crossref] [PubMed]
- Lazar SW, Bush G, Gollub RL, et al. Functional brain mapping of the relaxation response and meditation. Neuroreport 2000;11:1581-5. [Crossref] [PubMed]
- Tsai SL. Audio-visual relaxation training for anxiety, sleep, and relaxation among Chinese adults with cardiac disease. Res Nurs Health 2004;27:458-68. [Crossref] [PubMed]
- McDonald S, Hetrick S, Green S. Pre-operative education for hip or knee replacement. Cochrane Database Syst Rev 2004;CD003526 [PubMed]
- Chang BH, Dusek JA, Benson H. Psychobiological changes from relaxation response elicitation: long-term practitioners vs. novices. Psychosomatics 2011;52:550-9. [Crossref] [PubMed]
- Benson H, Proctor W. Relaxation revolution: The science and genetics of mind body healing. Simon and Schuster, 2011.
- Lindquist R, Tracy MF, Snyder M. Complementary & alternative therapies in nursing. Springer Publishing Company, 2018.
- Foji S, Tadayonfar MA, Mohsenpour M, et al. The study of the effect of guided imagery on pain, anxiety and some other hemodynamic factors in patients undergoing coronary angiography. Complement Ther Clin Pract 2015;21:119-23. [Crossref] [PubMed]
- Liu Y, Petrini MA. Effects of music therapy on pain, anxiety, and vital signs in patients after thoracic surgery. Complement Ther Med 2015;23:714-8. [Crossref] [PubMed]
- Nelson K, Adamek M, Kleiber C. Relaxation training and postoperative music therapy for adolescents undergoing spinal fusion surgery. Pain Manag Nurs 2017;18:16-23. [Crossref] [PubMed]
- Felix MMDS, Ferreira MBG, da Cruz LF, et al. Relaxation therapy with guided imagery for postoperative pain management: an integrative review. Pain Manag Nurs 2019;20:3-9. [Crossref] [PubMed]
Cite this article as: Wei S, Li L, Yang X, Li X, Jiang Q. Psychological interventions in the pain management after hip and knee arthroplasty: a mini review. Ann Joint 2020;5:13.


