Risk of endoprosthetic infection and impact of health-related quality of life in patients with osteosarcoma and giant cell tumor of bone; a retrospective case-control study
Introduction
Endoprosthetic reconstruction is a common method used in orthopedic oncology following resection of bone sarcomas to for limb salvage with the intention of preserving function and patient quality of life. As survival rates continue to improve for patients with primary bone sarcomas, implant failure is a major threat to limb salvage and quality of life. Endoprosthetic or prosthetic joint infections (PJI) continue to be the most common mode of failure, with rates between 0–22% recorded in the literature within the first two years depending on the reconstruction method (1-5).
Prosthetic joint infections often present with pain and can prevent patients from engaging in work or other instrumental activities of daily living, which can negatively influence patients’ health-related quality of life (HR-QoL) (6-8). The additional treatments necessary to control the infection and subsequent rehabilitation can have lasting effects for the patient well beyond the course of infection. Patients who experience acute or chronic infection also incur increased healthcare costs and may lose wages due to reduced function and longer hospital stays, increasing financial burden on both the individual and the system (9). The impact of infection and resulting sequelae can be determined by measuring HR-QoL as reported by the patient. Measuring HR-QoL is crucial in values-based, patient centered care. Discrepancies between patient and physician reporting of functional outcomes have been observed, which can affect the patient-physician relationship, therefore, understanding how a medical condition or treatment course affects patients’ perception of their daily lives enables physicians to manage expectations of outcomes and counsel patients more appropriately (10).
While there is a considerable body of literature reporting on the incidence of prosthetic joint infection and efficacy of various treatment approaches both in primary arthroplasty and tumor endoprostheses, there is very little regarding the effect of infection and subsequent treatments on HR-QoL among oncologic patients following limb salvage surgery. With this in mind, our primary aim is to evaluate the functional and HR-QoL outcomes in oncologic patients who underwent two-stage revision for an infected Compress® (Zimmer-Biomet Inc., Warsaw, ID, USA) endoprosthetic implant for in the distal femur and determine whether or treatment for an infection negatively impacts HR-QoL compared to matched controls who did not experience an infection.
Treatments for prosthetic joint infections include oral or intravenous antibiotics coupled with irrigation and debridement (I&D), single stage or two-staged revision, or ultimately, amputation. While two-stage revisions have been cited to have the highest success rate in controlling repeat infection, two-stage revisions often result in muscle atrophy and bone loss (2,5). This can lead to further functional decline, requiring intensified rehabilitation and sometimes use of assistive devices. The treatment of infected Compress® endoprostheses at our institution has been a two-stage implant exchange with retention of the osseointegrated spindle. Our secondary aims are to evaluate our (I) overall infection rate among oncologic patients in whom the Compress® endoprosthesis was used to reconstruct the distal femur, (II) determine our infection eradication and limb salvage rates following treatment of endoprosthetic infection and (III) identify factors that may contribute to a patient’s risk of developing an infection.
Methods
Patient cohort
We performed a retrospective 2:1 case-control study using a sample of patients who underwent limb-salvage reconstruction for an oncologic indication with the Compress® endoprosthesis at the distal femur. This study was approved by the Institutional Review Board at UCSF (10-02939).
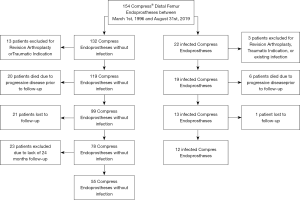
Patient demographic, oncologic, and surgical history, including presence or absence of infection and treatment outcomes, were retrieved from REDCap™, an electronic database maintained by the UCSF Orthopedic Oncology Group research team. Patients were imputed into the database if they were treated at UCSF March 1st, 1996 and August 31st, 2019 with the Compress® (Zimmer-Biomet Inc.) endoprosthesis for reconstruction of major skeletal defects. Two patients were treated at Kaiser Permanente by the senior partner prior to moving to UCSF (RJO) and subsequently followed at UCSF, the remaining patients were surgically treated at UCSF. Patients with a diagnosis of distal femur osteosarcoma or giant cell tumor of bone treated with this implant were included in the study. Patients were also included in the study if the distal femur Compress® endoprosthesis was used to revise a previous treatment of a distal femur giant cell tumor of bone or osteosarcoma. Patients that underwent Compress® reconstruction for a different oncologic indication or a non-oncologic indication such as trauma or failed arthroplasty were excluded. Patients with an infection were included if there was a minimum two-year follow-up following diagnosis of an infection or until amputation. Patients without an infection were included if there was a minimum two-year follow-up from initial implantation. Patients were excluded from this study if they expired prior to follow up or were unresponsive after three phone attempts. Figure 1 demonstrates the inclusion and exclusion of the cohort.
We identified 154 patients who received a Compress® endoprosthesis at the distal femur within this time frame. Sixteen total patients were excluded for a non-oncologic indication. Six patients in the infection cohort and 21 patients in the control cohort died due to progressive disease prior to follow-up for this study. One patient in the case group and 21 patients in the control group were lost to clinical follow-up, defined as less than two-year of follow-up. This left 12 patients with a history of a PJI and 55 without with minimum two-year follow-up and eligible for this study.
Prosthetic joint infections were identified through retrospective chart review and deemed septic if the patient presented with one or more positive laboratory tests (elevated CRP, positive culture on knee aspiration) or clinical symptoms (pain, weakness) that required any combination of debridement, antibiotic therapy, staged revision, or amputation. To categorize the time at which infection occurred, we followed the system established by Fitzgerald et al., which has been well-utilized in other literature (11,12). Class I infections occurred within the first three months after index surgery with the Compress® (Zimmer-Biomet Inc.) endoprosthesis for reconstruction of major skeletal defects (early), Class II infections between three months and 24 months of implantation (delayed), and Class III infections occurred beyond 24 months from surgery (late). Outcomes were then reported as either functional limb salvage without lifetime suppressive antibiotic therapy, limb salvage with lifetime suppression, or above-knee amputation.
Twelve patients with a documented infected Compress® endoprosthesis met inclusion and exclusion criteria. Fifty-five patients without infection with adequate follow-up were considered potential controls. Control patients were matched by the year of index surgery (±2 years), then by diagnosis (Osteosarcoma or Giant Cell Tumor), then, if possible, age at index surgery (±5 years). If there were multiple suitable matches in the Control group, patients were randomly assigned.
Questionnaires
Patients were contacted by phone and asked if they were interested in completing the HR-QoL questionnaires and participating in this study. Following verbal consent, participants were sent an electronic informed consent form using DocuSign®. After gaining written consent, patients were then were sent the TESS and EQ-5D-VAS questionnaires by mail or email to complete privately.
The EQ-5D-VAS (EuroQoL Group) is a quantitative tool to measure of HR-QoL, reflecting the patient’s evaluation of their health status. It addresses five dimensions of HR-QoL: mobility, self-care, usual activities, pain, and mental health. The patient chooses one statement that they identify most with for each domain, with self-assessments ranging from significant difficulty to no difficulty within each dimension. Each statement is assigned a value on a three-point scale, three representing “no difficulty at all” and one representing “significant difficulty”. The EQ-5D-VAS includes a summative visual analogue scale, prompting the patient to choose a point on a line scale, zero indicating the worst overall health they can be in today, and 100 indicating the best.
The Toronto Extremity Salvage Score (TESS, University of Toronto) measures the degree of disability or impairment perceived by the patient in completing activities of daily living, using definitions established by the World Health Organization. There is a survey for either the upper or lower extremity; we chose to use the lower extremity as limb salvage was only performed at the distal femur in this study. There are 28 questions for the lower extremity; items are rated on a five-point scale, ranging from “Not at all difficult” to “Impossible to do”. If the activity is not applicable to the patient, the patient can select “Not applicable to me” and the score is not considered. A five reflects no difficulty at all, while a zero indicates the task is impossible to do. A higher score suggests the patient does not believe they experience any disability.
Surgical procedure
The Compress® Compliant Pre-Stress implant takes advantage of Wolff’s Law to promote osseointegration at the bone-implant interface, thus providing an alternative to traditional intramedullary stems used to anchor large implants. The surgical technique has been previously described in detail (13). Most cases used a large, 800-pound force spindle; a 600-pound spindle was recommended by the manufacturer for younger patients receiving an expandable implant, or for patients with thin cortices. The distal femoral component was paired with a rotating platform, hinged total knee replacement [the Orthopaedic Salvage System (OSS™), Zimmer-Biomet Inc.] with a short non-modular cemented tibial baseplate.
Prevention and treatment of infection
Prior to each surgery, the patient’s entire hindquarter was prepped and draped in routine sterile fashion; the skin was also covered with Ioban to decrease the risk of infection. Body exhaust suits were used for the same purpose. Preoperative intravenous antibiotics, predominantly Cefazolin (Ancef), were administered, followed by a postoperative antibiotic course typically until the patient’s drains were removed.
If an infection was suspected and confirmed, standard course of treatment involved a two-stage implant exchange. Stage one involved an extensive debridement with removal of all modular components; the spindle was retained if there was good osseointegration noted intraoperatively. Following explantation, an antibiotic cement coated distal femur was implanted. Patients were then started on broad spectrum antibiotics, which were narrowed once culture speciation was available. Patients were treated with six weeks of IV antibiotics. Once the ESR, CRP and WBC levels normalized patients were re-implanted with a new distal femur implant and bearings. If infectious labs had not normalized patients underwent a subsequent debridement and course of IV antibiotics. In conjunction with the infectious disease team, individuals in whom infectious markers did not reach normal levels following two debridements were placed on lifelong suppressive oral antibiotics after reimplantation.
Statistical analysis
Demographic and surgical variables were compared between the cases and controls using odds ratio for binary variables and the Wilcoxon rank sum test was used to compare ordinal variables.
Results
Infection
Overall, a deep endoprosthetic infection was diagnosed in 22 patients (14.3%) (Figure 1). Of the 22, three patients were not included in analysis because they underwent limb salvage surgery for trauma or revisional arthroplasty making the rate of infection for patients treated for a primary or revision oncologic indication 13.7%. The time course of infection was not determined for one patient due to incomplete chart history. Of 18 patients with documented infection, one infection occurred within three months of index surgery, eight infections were diagnosed between three and 24 months after index surgery, and nine were beyond 24 months of index surgery.
The overall demographic and culture data of the 18 reported infections in oncologic patients is shown in Table 1. The average follow-up was 99 months for these patients (range, 38–203 months). Patients 14–18 died due to progressive disease prior to follow-up for this study and were excluded from HR-QoL analyses and the case-control analysis.
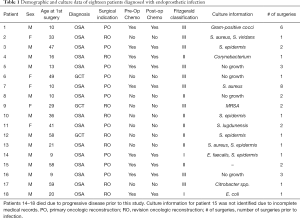
Full table
Table 2 demonstrates the various treatments for the 18 patients. Six patients (33.3%) did not respond to an initial one or two-stage exchange and IV antibiotics, requiring subsequent surgical debridement and repeated implant exchanges. Ultimately, six cases (33.3%) resulted in above the knee amputations, four of which were due to persistent infection, one where the patient had no detectable infection but was not interested in lifetime suppression with antibiotics, and one due to recurrence of disease diagnosed at the time of infection. Patient #2 completed a course of oral and IV antibiotics, but treatment was unsuccessful; patient presented six weeks later with reinfection and opted for an amputation. Patient #3 was previously treated with IV antibiotics for a superficial abscess but did not complete the course. Three months later, the patient presented with signs of prosthetic joint infection, and opted for an amputation rather than a two-stage exchange and IV antibiotics.
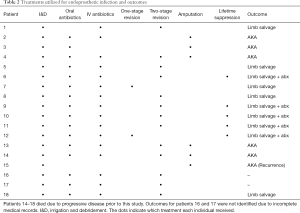
Full table
Case-control results
Twelve patients with adequate follow-up met the inclusion criteria to be considered infection cases. Of the available 55 surviving patients with an in situ distal femur Compress® endoprosthesis, 24 were matched to the cases (Figure 1). Table 3 shows the demographic and surgical variables for patients with distal femur Compress® infections and controls.
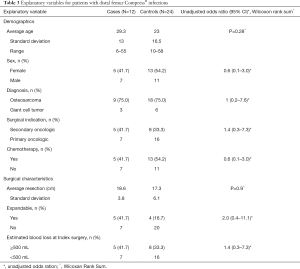
Full table
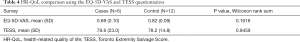
With regards to the HR-QoL data, three patients were not able to be contacted and three patients provided verbal and/or written consent but did not complete their surveys, resulting in a 50% response rate. In our control group, eight patients could not be reached and four patients provided verbal and/or written consent, but did not complete the surveys, resulting in a 50% response rate as well. There was no significant difference between the EQ-5D-VAS and TESS scores between the two groups (Table 4).
Full table
Conclusions
Patients diagnosed with osteosarcoma or giant cell tumor of the distal femur are routinely candidates for limb salvage surgery due to effective chemotherapy regimens and better cross-sectional imaging. As these diseases predominantly present in early to middle adulthood, patients often lead active lifestyles and we can expect them to live beyond the life of the implant. Successful limb salvage depends on durable implants. As implant quality continues to improve, aseptic loosening is no longer the main mode of implant failure; infection is now the most common cause of implant failure and late amputation (1-5,14).
We attempted to assess our rate of infection at the distal femur using the Compress® endoprosthesis for limb salvage reconstruction among patients with osteosarcoma and giant cell tumor of bone, quantify our rate of infection eradication and limb salvage rate following a two-stage implant exchange with osseointegrated spindle retention and IV antibiotics, explore risk factors for infection and evaluate the HR-QoL in patients treated for an infection compared to a similar non-infected limb salvage cohort.
Our overall infection rate was 14.2% at the distal femur. This is similar to other studies reported in the literature. Racano et al. performed a systematic review that included 48 papers and found an average infection rate of 10% for lower extremity endoprostheses including the proximal femur, distal femur and proximal tibia (15). Our infection rate is slightly higher than their reported average, however 50% of our infections occurred after two years. Our infection and control cohorts had an average follow-up of over eight and 10 years respectively. This study highlights the significant lifelong risk of a prosthetic joint infection in the oncologic population and demonstrates that the rate of infection increases with longer follow-up. Studies with an average two-year follow-up may have an artificially low infection rate.
In general, gram-positive cocci species, specifically coagulase-negative Staphylococci and S. aureus were the most common etiological agents, which is in agreement with other reports (2,5,16,17). Fifty percent of the infections occurred late and were considered Class III infections. As discussed by Fitzgerald et al., Class I infections are generally acute and are of nosocomial origin; common etiological agents are S. aureus and S. epidermis. Class II infections are considered delayed, with S. epidermis most commonly noted, suggesting contamination by native bacteria of the skin. Class III infections are late and generally present in an acute manner; occurring more than 24 months after surgery, but patients report an acute onset of symptoms of the affected joint. Class III infections are often acquired through the blood, either through injury or another procedure (18,19). This reiterates the importance of informing patients about the continued risk of infection, and to report any change in status of their limb, especially warmth and swelling, to their orthopedic oncologist.
We were unable to find significant predictors of an endoprosthetic infection with our available data. Data on BMI was not found for many of the patients treated prior to 2012 when the current electronic medical record was adopted and therefore was not included in our analysis. The infected cohort had a slightly higher number of males, more secondary oncologic indications, fewer number of patients having received chemotherapy and an increased proportion of expandable endoprostheses, however, the 95% CI of the odds ratios crossed one, making these differences non-significant. Similarly, while a higher proportion of cases had >500 mL blood loss this did not approach significance. Of the variables assessed, whether or not an expandable was used came the closest to significance. Given that the expandable Compress® implant requires an open approach for lengthening this could be explained by multiple procedures increasing the risk of infection. Interestingly, whether or not a patient received chemotherapy did not appear to increase the odds of an infection, in fact a higher proportion in the control group received chemotherapy. This could be explained, however, by the fact that secondary oncology procedures, which occurred after any chemotherapy or for giant cell tumor of bone, made up a larger proportion of the infection cohort. It can be assumed that an increased number of surgeries prior to implantation of the Compress® would increase the risk of an infection. This did not bear out with the secondary oncologic group showing an OR of 1.4 (95% CI, 0.3–7.3).
Thirty-three percent of the infected cohort resulted in an amputation. One patient chose an amputation instead of attempt at continued limb salvage with a two-stage exchange upon the identification of an infection. Another patient experienced an infection around the same time as a local recurrence was diagnosed and underwent amputation for oncologic control. Therefore, four patients of the 14 patients with known outcomes (28.5%) who attempted continued limb salvage with a one or two-stage exchange and spindle retention failed treatment and went on to an above the knee amputation. The failure rate of implant exchange with spindle retention is comparable to what has been reported in the literature for complete two-stage exchange, with no retention of osseointegrated or well-fixed components. Other studies that evaluated the outcomes after two-stage exchange for oncologic implants found that 37–60% of patients who underwent two-stage exchange eventually opted for amputation due to infection (12,20,21). There is also a wide range of reinfection associated with two-stage exchange reported in the literature, ranging from 9–41%, and some reported no statistical significance between one-stage and two-stage exchanges in preventing re-infection (2,22-24). This highlights the importance of determining various patient risk factors that may make one-stage or two-stage more successful in treating the infection.
Our primary aim was to assess the effect of a prosthetic joint infection on a patient’s long-term HR-QoL. Unfortunately, due to poor survey response and difficulty reaching patients for consent we only had six individuals in the infected cohort and 12 patients in the control cohort return the surveys. This limits our ability to draw any conclusions on the effect of undergoing an implant exchange for infection on function and HR-QoL. From the few responses we did have we did not see a difference in EQ-5D-VAS or the TESS. This remains an important unanswered question with potential to guide our future treatment. Considering three possible outcomes of infection: eradication and limb salvage, life-long antibiotic suppression and limb salvage, and amputation; differences in satisfaction, function and HR-QoL between these three groups would be important to understand in order to counsel patients at the time of infection.
We performed a retrospective case control study of our osteosarcoma and giant cell tumor limb salvage patients and found that a one or two-stage implant exchange with retention of an osseointegrated spindle has similar limb salvage rates compared to a two-stage exchange with removal of all endoprosthetic components. We found that HR-QoL scores were similar among a small group of patients with successful infection treatment (i.e., continued limb salvage patients) and individuals who never experienced infection. While we were not able to detect whether or not there is a transient decrease in HR-QoL during treatment for infection these data are encouraging that treatment for an implant infection may not negatively impact long term HR-QoL, however, we had very low numbers complete the surveys and larger, prospective studies need to investigate this further. Interestingly 50% of the cohort experienced a late infection. More work needs to be done to elucidate the mechanism of late infections so as to set up preventative strategies.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Kurt R. Weiss and Mitchell S. Fourman) for the series “Osteosarcoma” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2020.02.03). The series “Osteosarcoma” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board at UCSF (10-02939) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ghert M, Deheshi B, Holt G, et al. Prophylactic antibiotic regimens in tumour surgery (PARITY): protocol for a multicentre randomised controlled study. BMJ Open 2012;2:e002197 [Crossref] [PubMed]
- Hardes J, Gebert C, Schwappach A, et al. Characteristics and outcome of infections associated with tumor endoprostheses. Arch Orthop Trauma Surg. 2006;126:289-96. [Crossref] [PubMed]
- Lentino JR. Prosthetic Joint Infections: Bane of Orthopedists, Challenge for Infectious Disease Specialists. Clin Infect Dis 2003;36:1157-61. [Crossref] [PubMed]
- Shehadeh A, Noveau J, Malawer M, et al. Late complications and survival of endoprosthetic reconstruction after resection of bone tumors. Clin Orthop Relat Res 2010;468:2885-95. [Crossref] [PubMed]
- Zajonz D, Zieme A, Prietzel T, et al. Periprosthetic joint infections in modular endoprostheses of the lower extremities: a retrospective observational study in 101 patients. Patient Saf Surg 2016;10:6. [Crossref] [PubMed]
- Allami M, Yavari A, Karimi A, et al. Health-related quality of life and the ability to perform activities of daily living: a cross-sectional study on 1079 war veterans with ankle-foot disorders. Mil Med Res 2017;4:37. [PubMed]
- Andersson LB, Marcusson J, Wressle E. Health-related quality of life and activities of daily living in 85-year-olds in Sweden. Health Soc Care Community 2014;22:368-74. [Crossref] [PubMed]
- Ran L, Jiang X, Li B, et al. Association among activities of daily living, instrumental activities of daily living and health-related quality of life in elderly Yi ethnic minority. BMC Geriatr 2017;17:74. [Crossref] [PubMed]
- Schrimpf C, Omar M, Schaper M, et al. A Retrospective Evaluation of Joint Endoprosthesis Infections and Depending Costs. J Surg Oper Care 2018;3:105.
- Janssen SJ, van Rein EA, Paulino Pereira NR, et al. The Discrepancy between Patient and Clinician Reported Function in Extremity Bone Metastases. Sarcoma 2016;2016:1014248 [Crossref] [PubMed]
- Barrett L, Atkins B. The clinical presentation of prosthetic joint infection. J Antimicrob Chemother 2014;69:i25-7. [Crossref] [PubMed]
- Jeys LM, Grimer RJ, Carter SR, et al. Periprosthetic infection in patients treated for an orthopaedic oncological condition. J Bone Joint Surg Am 2005;87:842-9. [Crossref] [PubMed]
- Goldman LH, Morse LJ, O’Donnell RJ, et al. How Often Does Spindle Failure Occur in Compressive Osseointegration Endoprostheses for Oncologic Reconstruction? Clin Orthop Relat Res 2016;474:1714-23. [Crossref] [PubMed]
- Henderson ER, Groundland JS, Pala E, et al. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am 2011;93:418-29. [Crossref] [PubMed]
- Racano A, Pazionis T, Farrokhyar F, et al. High infection rate outcomes in long-bone tumor surgery with endoprosthetic reconstruction in adults: a systematic review. Clin Orthop Relat Res 2013;471:2017-27. [Crossref] [PubMed]
- Nickinson RSJ, Board TN, Gambhir AK, et al. The microbiology of the infected knee arthroplasty. Int Orthop 2010;34:505-10. [Crossref] [PubMed]
- Runner RP, Mener A, Roberson JR, et al. Prosthetic Joint Infection Trends at a Dedicated Orthopaedics Specialty Hospital. Adv Orthop 2019;2019:4629503 [Crossref] [PubMed]
- Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev 2014;27:302-45. [Crossref] [PubMed]
- Anagnostakos K, Schmid NV, Kelm J, et al. Classification of hip joint infections. Int J Med Sci 2009;6:227-33. [Crossref] [PubMed]
- Sim IW, Tse LF, Ek ET, et al. Salvaging the limb salvage: Management of complications following endoprosthetic reconstruction for tumours around the knee. Eur J Surg Oncol 2007;33:796-802. [Crossref] [PubMed]
- Rougraff BT, Simon MA, Kneisl JS, et al. Limb salvage compared with amputation for osteosarcoma of the distal end of the femur. A long-term oncological, functional, and quality-of-life study. J Bone Joint Surg Am 1994;76:649-56. [Crossref] [PubMed]
- Castellani L, Daneman N, Mubareka S, et al. Factors Associated with Choice and Success of One- Versus Two-Stage Revision Arthroplasty for Infected Hip and Knee Prostheses. HSS J 2017;13:224-31. [Crossref] [PubMed]
- Masters JP, Smith NA, Foguet P, et al. A systematic review of the evidence for single stage and two stage revision of infected knee replacement. BMC Musculoskelet Disord 2013;14:222. [Crossref] [PubMed]
- Mortazavi SMJ, Vegari D, Ho A, et al. Two-stage exchange arthroplasty for infected total knee arthroplasty: predictors of failure. Clin Orthop Relat Res 2011;469:3049-54. [Crossref] [PubMed]
Cite this article as: Butte Z, Tanaka K, Andaya V, Zimel M, O’Donnell RJ, Wustrack R. Risk of endoprosthetic infection and impact of health-related quality of life in patients with osteosarcoma and giant cell tumor of bone; a retrospective case-control study. Ann Joint 2020;5:27.