
Clinical outcomes of rotator cuff repair in athletes
Introduction
Rotator cuff (RC) pathology is a common source of pain and disability in the athlete, across all ages, sports, and levels of competition (1). Degenerative tears are more common in the elderly and in those participating in overhead sports (2,3). Traumatic tears occur more frequently in contact athletes; and although RC pathology is uncommon in adolescent athletes, tears are usually of traumatic etiology (4,5). RC injuries may have a profound impact on an athlete’s career, and may limit the player’s ability to return to sport (RTS), or affect performance if a return to competitive sports is accomplished (6). Consequently, there has been continued focus on which surgical techniques may improve outcomes and RTS, particularly in the overhead and professional athlete populations (7). Although conservative management is usually performed initially for these injuries, many athletes may ultimately require surgical treatment (8). As both surgical technique and understanding of RC pathology in athletes have evolved in the past two decades, many have attempted to identify the ideal treatment strategy. Nonetheless, no one particular form of treatment has demonstrated clear superiority; and although many athletes may be successfully treated with surgical repair, overall outcomes and RTS may be unreliable in select populations (9,10).
Anatomy & pathophysiology
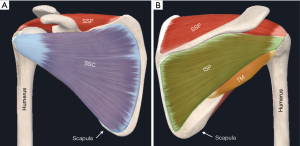
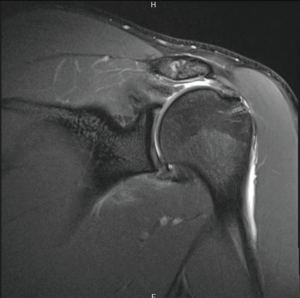
The RC is a complex structure that overlies the glenohumeral joint (GH) capsule and is comprised of four scapulohumeral muscles including the supraspinatus, infraspinatus, teres minor, and subscapularis (Figure 1). Collectively, these muscles form a musculotendinous cuff around the GH joint that provides dynamic stabilization and compresses the relatively large humeral head against the small, shallow glenoid via tonic contraction, achieving a stable arc of motion throughout the multidirectional movement of the shoulder (11-13).
Functionally, the RC muscles work together as a unit to maintain coordinated, joint-reacted forces that stabilize the GH joint during active range of motion (ROM) (14). The supraspinatus primarily abducts the humerus, the subscapularis provides internal rotation of the humerus, and the infraspinatus and teres minor externally rotate the humerus in the adducted and abducted positions, respectively. Any injury which disrupts the cuff’s pivotal contributions to normal shoulder stability and biomechanics, may result in instability, pain, weakness, and potentially abnormal glenohumeral translation.
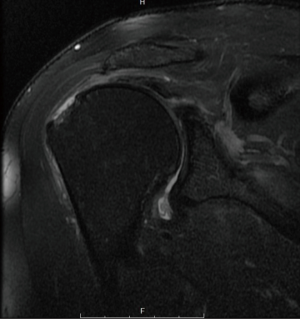
RC injuries may present along a continuum, ranging in severity from contusion or tendinopathy, to partial, or complete tear (Figure 2) (15). The etiology of RC injury varies based on age and sport type. Overhead athletes are susceptible to chronic repetitive microtrauma, often leading to partial thickness tears (16,17). In a study of asymptomatic Major League Baseball (MLB) pitchers, a significant correlation between innings pitched and the presence of RC tears (RCTs) was observed, suggesting that tears in these athletes are likely a consequence of chronic strain on the RC tendons (18). Contact athletes are also at risk of suffering RC injury, usually of traumatic rather than attritional nature. In reports of RCTs in American football players (8,19-22); tears present as mild contusions to partial and full thickness tears, and usually occur after a direct blow to the shoulder or a fall (8,21).
Epidemiology
The epidemiology of RCTs has not been well defined; however, prevalence has been reported to be around 10% in patients <20 years old, and up to 62% in patients >80 years old, indicative of the fact that RC pathology increases with age (23). Athletes may be at a particularly increased risk of RC injury, specifically those who play either overhead or collision sports. Chalmers et al. (24) reported that out of 581 shoulder surgeries in professional baseball players, roughly 32% were cuff injuries; 87% of these patients were diagnosed with an articular sided injury. Cohen et al. (4) assessed injury records of a professional football team over a period of 7 seasons, and found that nearly 50% of shoulder injuries involved RC contusions.
Although RCTs are more common with advancing age, these injuries can occur in younger patients due to traumatic injury and overuse. Weiss et al. reported 1.4% of patients seen for shoulder pain at two pediatric institutions were diagnosed with RCTs (25). Although rare in occurrence, these may be provoked by particularly injury-prone activity, such as pitching, playing on multiple teams during multiple seasons, or playing through pain (25).
Classification & associated pathology
Atraumatic tears
Atraumatic, degenerative tears of the RC are common and prevalence increases with age (23,26,27). Several studies on the natural history of RCTs have led to improved understanding of pathophysiology of degenerative tear formation (28). Teunis et al. (23) found that the overall prevalence of RC pathology ranged from 9.7% of patients aged 20 or younger, to as high as 62% in patients 80 years and older. Furthermore, Yamaguchi et al. (26) found that patients over the age of 65 years had a 50% likelihood of bilateral tears. The pathophysiology of atraumatic, degenerative RCTs is perceived to be a combination of “wear and tear” and inherent degenerative processes (23).
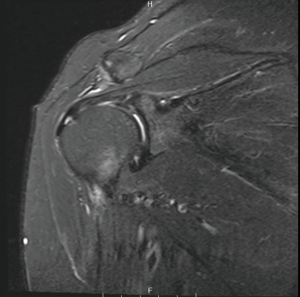
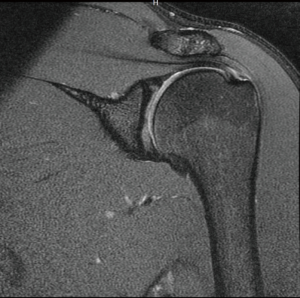
In athletes, atraumatic RCTs are common in overhead sports such as baseball, attributable to repetitive overuse and supraphysiological tendon strain during the throwing motion (29,30). In an MRI study of asymptomatic throwers, Connor et al. (31) found RCTs in 40%. RCTs in overhead athletes are thought to be attributable to tensile overload of the cuff, internal impingement (Figure 3), or subacromial impingement (Figure 4) (32). Internal impingement was first described by Walch et al. (33), as a pattern of cuff injury associated with the late cocking and early acceleration phases of throwing, when the undersurface of the supraspinatus tendon impinges between the greater tuberosity and the posterosuperior glenoid rim (33) (Figure 3). Microtrauma from repetitive internal impingement is associated with partial-thickness RCTs (PTRCTs), generally on the articular surface of the cuff (29). This is in contrast to subacromial impingement, which usually results in bursal-sided RCTs.
Most degenerative tears are asymptomatic. However, if these RCTs become symptomatic, an early course of 2–3 months of non-operative management is usually recommended (29,34-36). This involves activity modification, cryotherapy, anti-inflammatory medication, and physical therapy (29,35). The latter is likely the most important part of non-operative treatment. Posterior capsular stretches should be emphasized to maximize ROM, address scapular dyskinesis, and strengthen of the RC and periscapular muscles (29,32,35,37).
Traumatic tears
Compared to degenerative tears, traumatic RCTs are less common in the general population (21). Patients sustaining traumatic RCTs are usually male and of younger age (38). Mall et al. (38), reported the average age for patients with traumatic RCTs was nearly 10 years younger (54.7) than the average age of those with atraumatic tears in various other publications (36,39,40). Additionally, traumatic tears tend to be larger, with over 50% of RCTs demonstrating two tendon involvement (38), and only 22% of patients having RCTs classified as small (<3 cm). Hantes et al. (41) reported 88.5% of patients had massive or large tears in their traumatic cohort. The most common injury mechanism observed is a fall onto the outstretched arm (38,42-45), often associated with a forceful external rotation (43,44). This mechanism is frequently observed in anterior glenohumeral dislocations. Although RCTs are an uncommon result of GH dislocations in the young patient population, when traumatic tears do occur, it may be in association with a GH dislocation (38,45,46) (Figure 5). When a traumatic tear of the RC is sustained, early surgical treatment is usually preferred (41,42,47,48). Bassett and Cofield (42) demonstrated early repair within 3 weeks of injury leads to superior functional outcomes when compared with delayed repair. This is in concordance with the studies performed by Lähteenmäki et al. (48) and Hantes et al. (41), who reported excellent and good results for the early surgical management of traumatic cuff tears in 92% and 87%, respectively. In comparison to atraumatic, degenerative tears, early treatment of traumatic cuff tears may have the advantage of uncompromised biology, with less tendon retraction and no fatty degeneration of the muscle.
Associated conditions: GIRD, SLAP, internal impingement, scapular dyskinesia
There are various associated conditions that coexist with RCTs in athletes, some of which may in fact be causal. In 1992 Walch et al. (33) in his landmark article proposed the mechanism of internal impingement for the genesis of RCTs. When the arm was abducted to 90 degrees and fully externally rotated, impingement was arthroscopically observed between the undersurface of the infra- and supraspinatus tendon and the posterosuperior border of the glenoid. This arm position correlates with the typical late cocking or early acceleration phase of throwing. Jobe (49) hypothesized that internal impingement might be aggravated due to repetitive stretching of the anterior capsule and ligamentous structures. In contrast, Halbrecht et al. (50) exemplified that anterior instability leads to decreased internal impingement. Current understanding is that internal impingement is associated with posterior capsule contraction, rather than anterior capsular laxity (35). Posteroinferior capsular contracture is a commonly observed phenomenon in the throwers shoulder, and may lead to glenohumeral internal rotation deficit (GIRD), defined as decrease in internal rotation >20 degrees when compared to the contralateral shoulder (16,51). This adaptive process results from repetitive cocking during throwing motions. Although not always symptomatic, GIRD alters shoulder kinematics, leading to internal impingement and subsequent RCTs, as well as other concomitant pathologies (52,53). Another important concept that plays a role in symptomatic RCTs is SICK (scapular malposition, inferior medial border prominence, coracoid pain, and dyskinesis of scapular movement) syndrome (54). With the scapula resting in a protracted and upwardly tilted position, the glenoid face tilts anteriorly and superiorly (32), and the glenoid is brought towards the humeral head. This position of the humeral head relative to the scapula may increase the risk for posterosuperior RCTs via the mechanism of internal impingement.
Outcomes & tendency for progression after non-operative treatment
Symptomatic atraumatic RCTs usually undergo a course of non-operative treatment (29,34,35,55). In a large multicenter study, significant improvements of patient-reported outcomes were found at 6 and 12 weeks following the initiation of non-operative treatment in full-thickness RCTs (FTRCTs) (55). The authors concluded that nonoperative treatment with a specific physical therapy regimen is effective for 75% of patients with FTRCTs (55). Similar results for non-operative treatment of chronic FTRCTs were demonstrated by another working group (36); in patients who underwent a successful course of initial non-operative treatment, 75% remained asymptomatic at 5-year follow-up (36). Interestingly, delayed surgery after failed conservative treatment (between 3 months and 5 years) resulted in similar outcomes when compared to early surgical treatment (after failed initial non-operative management) (36). In a systematic review and meta-analysis of level I and II evidence comparing operative to non-operative management of FTRCTs, authors found statistically significant differences after 1 year in the Constant and VAS scores, favoring surgery (56). However, these differences were small, and did not approach clinical significance (56).
Although most symptomatic RCTs respond well to non-operative treatment, there is a risk for tear progression. In a study that evaluated the performance of MLB players after RCT and RC repair (RCR), the authors found that players who ultimately underwent surgical treatment had the tendency to experience a general decline in their performance leading up to their operation (6). Yamamoto et al. demonstrated tear progression in 47% of symptomatic RCTs during mean observational period of 19 months (57). Kim et al. found that 82.4% of symptomatic FTRCTs and 26.1% of PTRCTs propagated over a follow-up period from 6–100 months (58). They concluded that tears treated non-operatively should be monitored closely, especially FTRCTs.
Outcomes and return to play after repair
Surgical repair of RCTs in the athlete may be performed open, mini-open (arthroscopically assisted), or arthroscopically; although arthroscopic repair is now the predominant choice of treatment for posterosuperior RCTs (59). The ultimate modality of repair is dependent upon multiple patient-specific factors, such as age, sport, position, goals, and characteristics of the tear, as well as surgeon experience and preference (1). Although there is limited evidence supporting one approach over another (60,61), arthroscopic repair continues to increase in prevalence as techniques evolve. This is likely due to several proposed benefits, including improved visualization and mobilization of tears, decreased postoperative pain, accelerated recovery (62,63), and the avoidance of many of the complications associated with open surgery, including deltoid compromise and increased rates of nerve injury, infection, and joint stiffness (64,65).
Timing of RTS
It is important to note that RTS after surgery is a variable end-point, and also may not represent return to previous level of play (7). There has been an effort to utilize performance-based statistics to assess performance after surgery, particularly in throwers. However, there is considerable variability in how these statistics are applied and reported (7). Furthermore, there are a multitude of external factors to consider when evaluating RTS in the elite level athlete after surgery, including position, age, mental acuity, athlete goals, position in lineup, quality of competition, travelling schedule, and other injuries (7,66).
Timing of return to play may be forestalled by any combination of these influences, and the treating physician must counsel prospective patients accordingly. In 2019 a study by Kim et al. (67), found that return to previous level of functioning activity may take over a year after surgery. After surgery, patients required 14 months on average to recover their high-level sporting motion; patients with large tear size or re-tear were significantly delayed in RTS and restoration of motion. Similarly, in an evaluation of patients across a variety of types of shoulder surgery, Weber et al. (68) found a 13% average decline in level of sport at six months follow-up. Accordingly, the physician must regard RTS as a dynamic endpoint, dependent upon multiple factors and length of time after surgery. Furthermore, RTS may be affected upon method of repair. In a 2014 review, Millett and Warth concluded that proper recognition of tear pattern and appropriate selection of fixation construct may determine outcomes after RCR (69).
Return to play in recreational and competitive athletes
RTS after RCR has been consistently demonstrated to be higher in recreational (34) versus professional athletes (9,70,71). While the vast majority of the recreational athletes have been shown to RTS after arthroscopic RCR, typically at the same pre-injury level and intensity (72), the same cannot be said for professional athletes (71).
In a 2016 systematic review and meta-analysis of the rate of RTS after surgical treatment of RCTs in 683 athletes, Klouche et al. (73) found an overall 84.7% RTS from four to seventeen months after surgery; 65.9% of patients returned at equivalent level of play, and subgroup analysis showed no significant difference between PT and FTRCTs. However, while 81.4% of recreational athletes returned to the preinjury level of sport, only 49.9% of professional and competitive athletes returned to prior level.
In a 2020 systematic review of RTS between recreational and competitive athletes, Altintas et al. (9) reported that overall, most athletes (70.2%) were able to return to preinjury level of play after arthroscopic RCR. However, recreational sports were associated with much higher rate of return to preinjury level (73.3%), whereas competitive (61.5%) and overhead sports (38%) were associated with significantly lower return to preinjury level. Exactly why all athletes are unable to return to preinjury level of performance remains uncertain and is likely multifactorial in nature. Identified risk factors for RTS at a lower level include overhead sport, delayed RTS, (74) and professional status (75,76).
Contact athletes
Contact athletes have generally displayed a high level of RTS after RCR (21,71). Although most RCTs may eventually require surgical repair in this population (8), RTS remains high after RCR. In a survey of NFL team physicians, 51 FTRCTs were identified across a 10-year study period, 92% ultimately requiring surgical repair (8). Rates of RTS after RCR in contact athletes have been demonstrated to be over 90% in several studies including professional athletes (21,34,71). Tambe et al. (77) reported on arthroscopic RCR in 11 professional rugby players, with all patients returning to previous level of sport at an average of 4.8 months postoperatively.
The concern for poor outcome or failure to RTS in contact athletes may be more related to unaddressed instability or repeat traumatic event (19,78,79).
Overhead athletes, throwers, and golfers
Outcomes after RCR in overhead athletes are significantly poorer and RTS remains unpredictable when compared to other athlete populations. There is a genuine possibility that an injury requiring surgery may prevent return to competitive play (29,80). In a 2018 review including 314 athletes analyzing the impact of RC surgery on postoperative sporting performance, Reuter et al. (71) reported that only 48% of professional overhead athletes return to their prior level of competition after arthroscopic surgery.
These differences are most-pronounced in the throwing population (81), while other groups may see more encouraging results after surgery. In recreational level golfers, RCR has been shown to allow for a high level of return to pain-free golfing at equivalent level of play; with a 90% RTS and no difference in drive distance or handicap in a study of 30 patients by Vives et al. (82). In a group of 12 climbers, Simon et al. (83) documented a 100% RTS, with 11 of 12 returning to high level rock climbing. In 51 nonprofessional tennis players undergoing RCR, Sonnery-Cottet et al. (74) reported a 78.4% RTS at a mean 9.8 months after surgery, with 77.5% returning to preinjury level. In a group of 8 female professional tennis players, Young et al. (84) performed arthroscopic RCR or labral repair and reported an 88% RTS, but only 25% of players regained their pre-injury singles ranking. In a 2016 retrospective study of 76 patients, Antoni et al. (72) demonstrated 88.6% RTS after RCR in shoulder dependent athletes: 91.7% in golfers, 88.9% in tennis players, and 76.9% in swimmers.
Although positive outcomes have been shown to be significantly more difficult to obtain in throwers, some studies have demonstrated superb results after FTRCR. In 21 amateur overhead-throwers, Liem et al. (75) reported a RTS of equal intensity and duration of all patients at a mean of 6.3 months after repair. Patients in this study estimated their postoperative condition to be significantly improved compared to their preoperative conditions. Subsequently, these results have been difficult to reproduce. In a 2019 review of 581 professional baseball players, Chalmers et al. (24) reported a RTS after shoulder surgery of 63%; however of those who returned, 86% did achieve an equal or higher level of play. Mazoue and Andrews (76) reported that after repair of FTRCTs in 16 MLB players, only 8% of pitchers were able to RTS; of position players with FTRCTs in the dominant and nondominant shoulder, 50% and 100% were able to RTS, respectively. Return to preinjury level of play after repair of FTRCTs in professional baseball athletes remains unpredictable, and accordingly, patients must be counselled that these can potentially be career-ending injuries (76,81,85,86).
Partial-thickness tear (PTRCTs) repair versus debridement
In the available literature there has been no consensus on the best surgical technique for optimal outcomes in the treatment of symptomatic PTRCTs (87). In a review of 314 patients treated surgically for RCTs, Reuter et al. (71) reported comparable RTS in professional overhead athletes after either arthroscopic debridement (53.7%) or repair (47.5%). The most common form of treatment for PTRCT in the elite-level thrower remains debridement; concern persists that repair may result in over-constraint and poor RTS (29). Consistent with this, Chalmers et al. (24) recently reported a 84% of debridement vs. 18% rate of repair in 581 professional baseball players. In 2019, Erickson et al. (10) analyzed RC surgery of 151 professional baseball athletes, noting debridement represents the vast majority of cases at 86%. RTS following both debridement and repair were low, at 50.8% and 33.3% respectively; and in players who returned, performance declined. For professional throwers undergoing PTRCT debridement, RTS at prior level of play has been shown to be between 45–76% (88-90). Reynolds et al. (90) performed debridement alone of PTRCTs in 82 professional baseball pitchers, with the majority (76%) returning to competitive pitching and reporting good to excellent outcomes at an average of 10.7 months. However, returning to their previous elite level of play remained a challenge, as only 55% returned at the same level or higher, 65% reported decreased pitch control, and 71% returned with decreased pitch velocity.
PTRCT repair in overhead athletes has also shown variable results, ranging from 33% to 89% RTS at prior level (35,91-93). Conway (93) reported an 89% return to same or higher level of play following a PTRCR in a sample of 14 high-level baseball players. These results may be compared with those of Dines et al. (94), who demonstrated that arthroscopic repair with a lateralized footprint technique in 6 MLB baseball players allowed 83% RTS at mean follow-up of 5.5 years; however, mean performance was uniformly diminished. Innings pitched decreased from 1,807 to 184 and few resumed pitching at the same level; postoperative pitching statistics also declined. In a 2019 study of a general population of 72 athletes treated with arthroscopic in situ repair for PTRCTs, Rossi et al. (95) demonstrated excellent functional outcomes, with a RTS in the vast majority of patients (87%), with most returning to pre-injury level (80%). Average RTS was 5.6 months; both articular- and bursal-sided tears demonstrated equally favorable results. During long-term follow-up of 62 patients (minimum of 8 years), the same group reported excellent functional outcomes in over 80%, with no patients requiring revision surgery (96).
In the treatment of 43 athletes under age 40, more than half of which were collegiate or professional, Payne et al. (89) assessed outcomes after PTRCT treatment. In patients with acute, traumatic injuries, all were treated with subacromial decompression (SAD) and debridement, and 86% had satisfactory postoperative results and 64% returned to preinjury sports. In overhead athletes with insidious, atraumatic shoulder pain treated with debridement outcomes were poorer, with only 66% satisfactory results and 45% RTS. Within this group, the authors noted an association of poor outcomes after debridement alone in those with increased glenohumeral translation or posterior labral tears. In those without instability, pain relief was excellent, however RTS remained under 50%.
Adolescent athletes
Although RCTs are rare in this population, adolescent athletes have generally displayed very favorable outcomes and high RTS after RCR (5,25,97). Amongst other factors, this may be due to age and healing capacity, traumatic etiology of injury, or lack of co-existent pathology (98,99). Due to the rarity of injury, reports have generally been limited to small case series. In a more recent 2018 retrospective series of 28 patients with PT and FTRCTs, Azzam et al. (5) demonstrated excellent outcomes after repair at midterm follow-up, with 93% RTS of all athletes at similar level or higher. This comes with a caveat however, as 57% of the overhead athlete subgroup were forced to switch positions. The difficulty of RTS in throwers has been well documented in the literature, and seems to remain applicable in the adolescent population (100).
Elderly athletes
Studies in elderly athletes have been limited, but in a 2015 study, Bhatia et al. (2) were able to demonstrate successful outcomes after RCR. In a group of 49 shoulders over age 70, the authors found arthroscopic RCR to be highly effective in reducing pain and improving function, with 77% of patients returning to their sport at an equivalent level of intensity.
Postoperative rehabilitation
Postoperative rehabilitation is an important component after RC surgery; goals are minimization of pain, restoration of ROM, and reinstatement of previous levels of functionality. Many studies have recently focused on the association of duration of post-operative immobilization with ROM progression (101-104). Early immobilization has been associated with superior bone-tendon healing in the immediate post-operative period (105) and has not been shown to negatively impact the integrity of the remodeled tendon (106). Conversely, delaying motion may delay functional recovery, due to increased stiffness and muscle atrophy (107-110). Houck et al. (111) performed a systematic review of 7 overlapping meta-analyses directly comparing early passive motion (EPM), motion beginning within 1 week post-surgery, and delayed motion (immobilization for a minimum of 4–6 weeks). Results were inconclusive in regard to superiority; however, many of the studies noted improved ROM but higher re-tear rate with early motion, and better healing with delayed motion. Importantly, several studies concluded that tear size played an important factor in protocol determination and success. Littlewood et al. (104) conducted a systematic review that included 7 studies which evaluated early versus delayed rehabilitation. In opposition to the findings of Houck et al., they concluded that studies in which patients were diagnosed with small-to-medium-sized tears had comparable outcomes to studies in which patients were diagnosed with medium-to-large-sized tears, challenging the concept that larger tears may require a more delayed and/or conservative approach.
Ultimately, strong scientific evidence supporting a definitive postoperative rehabilitation protocol is lacking; thus, the authors recommend a comprehensive approach that takes into consideration athlete goals, surgical findings, tissue quality, tear size, and post-surgery risks—including stiffness and re-tear rate. It is important to avoid over tensioning the repair during the immediate post-operative period (112). The authors opt for immobilization for 6 weeks with early passive ROM beginning immediately after surgery. At 6 weeks, full passive motion is allowed and active-assisted motion is initiated. This is progressed until the patient can perform active assisted motion without pain, then active motion is gradually progressed. Usually between 8–10 weeks strengthening begins. Generally, between 14- and 16-week patients are allowed full RTS without restriction.
Conclusions
In summary, outcomes after surgical treatment of RC pathology in athletes remain unpredictable. Recreational athletes, adolescent athletes, and those involved in contact sports are more likely to RTS at the preinjury level of play; whereas the rate of RTS and post-operative performance in professional and overhead athletes have been disappointing. In the treatment of partial thickness tears, there has been no consensus on debridement versus repair; both forms of treatment have shown comparable rates of RTS, although debridement remains vastly more common, particularly in the throwing population. Future areas of research should include increased validation and consistency of performance metric reporting, as there has been considerable inconsistency on the general outcome of successful RTS.
Acknowledgments
Research performed at the Steadman Philippon Research Institute, Vail, CO.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Adnan Saithna) for the series “Current and Emerging Concepts in the Management of Rotator Cuff Tears” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (http://dx.doi.org/10.21037/aoj-20-40). The series “Current and Emerging Concepts in the Management of Rotator Cuff Tears” was commissioned by the editorial office without any funding or sponsorship. PCN reports personal fees from Arthrex, outside the submitted work. The position of PCN at the Steadman Philippon Research Institute is supported by Arthrex. PJM reports grants, personal fees and other from Arthrex, Inc., other from Smith & Nephew, other from Siemens, other from Össur, personal fees from Medibridge, personal fees from Springer Publishing, other from VuMedi, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Weiss LJ, Wang D, Hendel M, et al. Management of Rotator Cuff Injuries in the Elite Athlete. Curr Rev Musculoskelet Med 2018;11:102-12. [Crossref] [PubMed]
- Bhatia S, Greenspoon JA, Horan MP, et al. Two-Year Outcomes After Arthroscopic Rotator Cuff Repair in Recreational Athletes Older Than 70 Years. Am J Sports Med 2015;43:1737-42. [Crossref] [PubMed]
- Camp CL, Dines JS, van der List JP, et al. Summative Report on Time Out of Play for Major and Minor League Baseball: An Analysis of 49,955 Injuries From 2011 Through 2016. Am J Sports Med 2018;46:1727-32. [Crossref] [PubMed]
- Cohen SB, Towers JD, Bradley JP. Rotator cuff contusions of the shoulder in professional football players: epidemiology and magnetic resonance imaging findings. Am J Sports Med 2007;35:442-7. [Crossref] [PubMed]
- Azzam MG, Dugas JR, Andrews JR, et al. Rotator Cuff Repair in Adolescent Athletes. Am J Sports Med 2018;46:1084-90. [Crossref] [PubMed]
- Namdari S, Baldwin K, Ahn A, et al. Performance after rotator cuff tear and operative treatment: a case-control study of major league baseball pitchers. J Athl Train 2011;46:296-302. [Crossref] [PubMed]
- van der List JP, Camp CL, Sinatro AL, et al. Systematic Review of Outcomes Reporting in Professional Baseball: A Call for Increased Validation and Consistency. Am J Sports Med 2018;46:487-96. [Crossref] [PubMed]
- Foulk DA, Darmelio MP, Rettig AC, et al. Full-thickness rotator-cuff tears in professional football players. Am J Orthop (Belle Mead NJ) 2002;31:622-4; discussion 624.
- Altintas B, Anderson N, Dornan GJ, et al. Return to Sport After Arthroscopic Rotator Cuff Repair: Is There a Difference Between the Recreational and the Competitive Athlete? Am J Sports Med 2020;48:252-61. [Crossref] [PubMed]
- Erickson BJ, Chalmers PN, D'Angelo J, et al. Performance and return to sport following rotator cuff surgery in professional baseball players. J Shoulder Elbow Surg 2019;28:2326-33. [Crossref] [PubMed]
- Karduna AR, Williams GR, Williams JL, et al. Kinematics of the glenohumeral joint: influences of muscle forces, ligamentous constraints, and articular geometry. J Orthop Res 1996;14:986-93. [Crossref] [PubMed]
- Halder AM, Zhao KD, Odriscoll SW, et al. Dynamic contributions to superior shoulder stability. J Orthop Res 2001;19:206-12. [Crossref] [PubMed]
- Lee SB, Kim KJ, O'Driscoll SW, et al. Dynamic glenohumeral stability provided by the rotator cuff muscles in the mid-range and end-range of motion. A study in cadavera. J Bone Joint Surg Am 2000;82:849-57. [Crossref] [PubMed]
- Parsons IM, Apreleva M, Fu FH, et al. The effect of rotator cuff tears on reaction forces at the glenohumeral joint. J Orthop Res 2002;20:439-46. [Crossref] [PubMed]
- Kuhn JE. Current concepts: rotator cuff pathology in athletes--a source of pain or adaptive pathology? Curr Sports Med Rep 2013;12:311-5. [Crossref] [PubMed]
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part I: pathoanatomy and biomechanics. Arthroscopy 2003;19:404-20. [Crossref] [PubMed]
- Matava MJ, Purcell DB, Rudzki JR. Partial-thickness rotator cuff tears. Am J Sports Med 2005;33:1405-17. [Crossref] [PubMed]
- Lesniak BP, Baraga MG, Jose J, et al. Glenohumeral findings on magnetic resonance imaging correlate with innings pitched in asymptomatic pitchers. Am J Sports Med 2013;41:2022-7. [Crossref] [PubMed]
- Mueller M, Hoy G, Branson R. Management of In-Season Concurrent Rotator Cuff Tear With Shoulder Instability in Professional Contact Football Athletes; Respect the Career Goals! Asian J Sports Med 2016;7:e28377 [Crossref] [PubMed]
- Wang D, Weiss LJ, Abrams M, et al. Athletes With Musculoskeletal Injuries Identified at the NFL Scouting Combine and Prediction of Outcomes in the NFL: A Systematic Review. Orthop J Sports Med 2018;6:2325967118813083 [Crossref] [PubMed]
- Blevins FT, Hayes WM, Warren RF. Rotator cuff injury in contact athletes. Am J Sports Med 1996;24:263-7. [Crossref] [PubMed]
- Kaplan LD, Flanigan DC, Norwig J, et al. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med 2005;33:1142-6. [Crossref] [PubMed]
- Teunis T, Lubberts B, Reilly BT, et al. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg 2014;23:1913-21. [Crossref] [PubMed]
- Chalmers PN, Erickson BJ, D'Angelo J, et al. Epidemiology of Shoulder Surgery Among Professional Baseball Players. Am J Sports Med 2019;47:1068-73. [Crossref] [PubMed]
- Weiss JM, Arkader A, Wells LM, et al. Rotator cuff injuries in adolescent athletes. J Pediatr Orthop B 2013;22:133-7. [Crossref] [PubMed]
- Yamaguchi K, Ditsios K, Middleton WD, et al. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am 2006;88:1699-704. [Crossref] [PubMed]
- Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116-20. [Crossref] [PubMed]
- Codding JL, Keener JD. Natural History of Degenerative Rotator Cuff Tears. Curr Rev Musculoskelet Med 2018;11:77-85. [Crossref] [PubMed]
- Liu JN, Garcia GH, Gowd AK, et al. Treatment of Partial Thickness Rotator Cuff Tears in Overhead Athletes. Curr Rev Musculoskelet Med 2018;11:55-62. [Crossref] [PubMed]
- McFarland EG, Wasik M. Epidemiology of collegiate baseball injuries. Clin J Sport Med 1998;8:10-3. [Crossref] [PubMed]
- Connor PM, Banks DM, Tyson AB, et al. Magnetic resonance imaging of the asymptomatic shoulder of overhead athletes: a 5-year follow-up study. Am J Sports Med 2003;31:724-7. [Crossref] [PubMed]
- Economopoulos KJ, Brockmeier SF. Rotator cuff tears in overhead athletes. Clin Sports Med 2012;31:675-92. [Crossref] [PubMed]
- Walch G, Boileau P, Noel E, et al. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: An arthroscopic study. J Shoulder Elbow Surg 1992;1:238-45. [Crossref] [PubMed]
- Plate JF, Haubruck P, Walters J, et al. Rotator cuff injuries in professional and recreational athletes. J Surg Orthop Adv 2013;22:134-42. [Crossref] [PubMed]
- Shaffer B, Huttman D. Rotator cuff tears in the throwing athlete. Sports Med Arthrosc Rev 2014;22:101-9. [Crossref] [PubMed]
- Boorman RS, More KD, Hollinshead RM, et al. What happens to patients when we do not repair their cuff tears? Five-year rotator cuff quality-of-life index outcomes following nonoperative treatment of patients with full-thickness rotator cuff tears. J Shoulder Elbow Surg 2018;27:444-8. [Crossref] [PubMed]
- Kirchhoff C, Imhoff AB. Posterosuperior and anterosuperior impingement of the shoulder in overhead athletes-evolving concepts. Int Orthop 2010;34:1049-58. [Crossref] [PubMed]
- Mall NA, Lee AS, Chahal J, et al. An evidenced-based examination of the epidemiology and outcomes of traumatic rotator cuff tears. Arthroscopy 2013;29:366-76. [Crossref] [PubMed]
- Harris JD, Pedroza A, Jones GL, et al. Predictors of pain and function in patients with symptomatic, atraumatic full-thickness rotator cuff tears: a time-zero analysis of a prospective patient cohort enrolled in a structured physical therapy program. Am J Sports Med 2012;40:359-66. [Crossref] [PubMed]
- Moosmayer S, Lund G, Seljom U, et al. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: A randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br 2010;92:83-91. [Crossref] [PubMed]
- Hantes ME, Karidakis GK, Vlychou M, et al. A comparison of early versus delayed repair of traumatic rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 2011;19:1766-70. [Crossref] [PubMed]
- Bassett RW, Cofield RH. Acute tears of the rotator cuff. The timing of surgical repair. Clin Orthop Relat Res 1983;18-24. [PubMed]
- Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am 1996;78:1015-23. [Crossref] [PubMed]
- Ide J, Tokiyoshi A, Hirose J, et al. Arthroscopic repair of traumatic combined rotator cuff tears involving the subscapularis tendon. J Bone Joint Surg Am 2007;89:2378-88. [Crossref] [PubMed]
- Björnsson HC, Norlin R, Johansson K, et al. The influence of age, delay of repair, and tendon involvement in acute rotator cuff tears: structural and clinical outcomes after repair of 42 shoulders. Acta Orthop 2011;82:187-92. [Crossref] [PubMed]
- Namdari S, Henn RF 3rd, Green A. Traumatic anterosuperior rotator cuff tears: the outcome of open surgical repair. J Bone Joint Surg Am 2008;90:1906-13. [Crossref] [PubMed]
- Petersen SA, Murphy TP. The timing of rotator cuff repair for the restoration of function. J Shoulder Elbow Surg 2011;20:62-8. [Crossref] [PubMed]
- Lähteenmäki HE, Virolainen P, Hiltunen A, et al. Results of early operative treatment of rotator cuff tears with acute symptoms. J Shoulder Elbow Surg 2006;15:148-53. [Crossref] [PubMed]
- Jobe CM. Posterior superior glenoid impingement: expanded spectrum. Arthroscopy 1995;11:530-6. [Crossref] [PubMed]
- Halbrecht JL, Tirman P, Atkin D. Internal impingement of the shoulder: comparison of findings between the throwing and nonthrowing shoulders of college baseball players. Arthroscopy 1999;15:253-8. [Crossref] [PubMed]
- Kibler WB, Kuhn JE, Wilk K, et al. The disabled throwing shoulder: spectrum of pathology-10-year update. Arthroscopy 2013;29:141-61.e26. [Crossref] [PubMed]
- Manske R, Wilk KE, Davies G, et al. Glenohumeral motion deficits: friend or foe? Int J Sports Phys Ther 2013;8:537-53. [PubMed]
- Rose MB, Noonan T. Glenohumeral internal rotation deficit in throwing athletes: current perspectives. Open Access J Sports Med 2018;9:69-78. [Crossref] [PubMed]
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy 2003;19:641-61. [Crossref] [PubMed]
- Kuhn JE, Dunn WR, Sanders R, et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg 2013;22:1371-9. [Crossref] [PubMed]
- Piper CC, Hughes AJ, Ma Y, et al. Operative versus nonoperative treatment for the management of full-thickness rotator cuff tears: a systematic review and meta-analysis. J Shoulder Elbow Surg 2018;27:572-6. [Crossref] [PubMed]
- Yamamoto N, Mineta M, Kawakami J, et al. Risk Factors for Tear Progression in Symptomatic Rotator Cuff Tears: A Prospective Study of 174 Shoulders. Am J Sports Med 2017;45:2524-31. [Crossref] [PubMed]
- Kim YS, Kim SE, Bae SH, et al. Tear progression of symptomatic full-thickness and partial-thickness rotator cuff tears as measured by repeated MRI. Knee Surg Sports Traumatol Arthrosc 2017;25:2073-80. [Crossref] [PubMed]
- Dodson CC, Brockmeier SF, Altchek DW. Partial-Thickness Rotator Cuff Tears in Throwing Athletes. Operative Techniques in Sports Medicine 2007;15:124-31. [Crossref]
- Ji X, Bi C, Wang F, et al. Arthroscopic versus mini-open rotator cuff repair: an up-to-date meta-analysis of randomized controlled trials. Arthroscopy 2015;31:118-24. [Crossref] [PubMed]
- Bayle X, Pham TT, Faruch M, et al. No difference in outcome for open versus arthroscopic rotator cuff repair: a prospective comparative trial. Arch Orthop Trauma Surg 2017;137:1707-12. [Crossref] [PubMed]
- Gartsman GM, Khan M, Hammerman SM. Arthroscopic repair of full-thickness tears of the rotator cuff. J Bone Joint Surg Am 1998;80:832-40. [Crossref] [PubMed]
- Tauro JC. Arthroscopic rotator cuff repair: analysis of technique and results at 2- and 3-year follow-up. Arthroscopy 1998;14:45-51. [Crossref] [PubMed]
- Buess E, Steuber KU, Waibl B. Open versus arthroscopic rotator cuff repair: a comparative view of 96 cases. Arthroscopy 2005;21:597-604. [Crossref] [PubMed]
- Baker DK, Perez JL, Watson SL, et al. Arthroscopic vs. open rotator cuff repair: which has a better impact profile? J Shoulder Elbow Surg 2017;26:e155 [Crossref]
- Merolla G, Paladini P, Porcellini G. Assessment of return to play in professional overhead athletes subjected to arthroscopic repair of rotator cuff tears and associated labral injuries using the Italian version of the Kerlan-Jobe Orthopedic Clinic Shoulder and Elbow score. Musculoskelet Surg 2018;102:29-34. [Crossref] [PubMed]
- Kim HJ, Kim JY, Rhee YG. When Do Patients Return to Previous Daily Activity After Arthroscopic Rotator Cuff Repair? Clin Orthop Relat Res 2019;477:403-13. [Crossref] [PubMed]
- Weber A, Paraparan R, Lam PH, et al. Return to Sport at 6 Months After Shoulder Surgery. Orthop J Sports Med 2019;7:2325967119834077 [Crossref] [PubMed]
- Millett PJ, Warth RJ. Posterosuperior rotator cuff tears: classification, pattern recognition, and treatment. J Am Acad Orthop Surg 2014;22:521-34. [Crossref] [PubMed]
- Harris JD, Frank JM, Jordan MA, et al. Return to sport following shoulder surgery in the elite pitcher: a systematic review. Sports Health 2013;5:367-76. [Crossref] [PubMed]
- Reuter S, Imhoff AB, Martetschlager F. Impact of rotator cuff surgery on postoperative sporting activity. J Sports Med Phys Fitness 2018;58:480-8. [PubMed]
- Antoni M, Klouche S, Mas V, et al. Return to recreational sport and clinical outcomes with at least 2years follow-up after arthroscopic repair of rotator cuff tears. Orthop Traumatol Surg Res 2016;102:563-7. [Crossref] [PubMed]
- Klouche S, Lefevre N, Herman S, et al. Return to Sport After Rotator Cuff Tear Repair: A Systematic Review and Meta-analysis. Am J Sports Med 2016;44:1877-87. [Crossref] [PubMed]
- Sonnery-Cottet B, Edwards TB, Noel E, et al. Rotator cuff tears in middle-aged tennis players: results of surgical treatment. Am J Sports Med 2002;30:558-64. [Crossref] [PubMed]
- Liem D, Lichtenberg S, Magosch P, et al. Arthroscopic rotator cuff repair in overhead-throwing athletes. Am J Sports Med 2008;36:1317-22. [Crossref] [PubMed]
- Mazoué CG, Andrews JR. Repair of full-thickness rotator cuff tears in professional baseball players. Am J Sports Med 2006;34:182-9. [Crossref] [PubMed]
- Tambe A, Badge R, Funk L. Arthroscopic rotator cuff repair in elite rugby players. Int J Shoulder Surg 2009;3:8-12. [Crossref] [PubMed]
- Hart D, Funk L. Serious shoulder injuries in professional soccer: return to participation after surgery. Knee Surg Sports Traumatol Arthrosc 2015;23:2123-9. [Crossref] [PubMed]
- Gibbs DB, Lynch TS, Nuber ED, et al. Common Shoulder Injuries in American Football Athletes. Curr Sports Med Rep 2015;14:413-9. [Crossref] [PubMed]
- Dugas JR, Mathis TP. Partial Rotator Cuff Tears in Throwing Athletes. Operative Techniques in Sports Medicine 2016;24:196-202. [Crossref]
- Thorsness R, Alland JA, McCulloch CB, et al. Return to Play After Shoulder Surgery in Throwers. Clin Sports Med 2016;35:563-75. [Crossref] [PubMed]
- Vives MJ, Miller LS, Rubenstein DL, et al. Repair of rotator cuff tears in golfers. Arthroscopy 2001;17:165-72. [Crossref] [PubMed]
- Simon M, Popp D, Lutter C, et al. Functional and Sports-Specific Outcome After Surgical Repair of Rotator Cuff Tears in Rock Climbers. Wilderness Environ Med 2017;28:342-7. [Crossref] [PubMed]
- Young SW, Dakic J, Stroia K, et al. Arthroscopic Shoulder Surgery in Female Professional Tennis Players: Ability and Timing to Return to Play. Clin J Sport Med 2017;27:357-60. [Crossref] [PubMed]
- Tibone JE, Elrod B, Jobe FW, et al. Surgical treatment of tears of the rotator cuff in athletes. J Bone Joint Surg Am 1986;68:887-91. [Crossref] [PubMed]
- Park MC, Elattrache NS. Treating full-thickness cuff tears in the athlete: advances in arthroscopic techniques. Clin Sports Med 2008;27:719-29. [Crossref] [PubMed]
- Bollier M, Shea K. Systematic review: what surgical technique provides the best outcome for symptomatic partial articular-sided rotator cuff tears? Iowa Orthop J 2012;32:164-72. [PubMed]
- Andrews JR, Broussard TS, Carson WG. Arthroscopy of the shoulder in the management of partial tears of the rotator cuff: a preliminary report. Arthroscopy 1985;1:117-22. [Crossref] [PubMed]
- Payne LZ, Altchek DW, Craig EV, et al. Arthroscopic treatment of partial rotator cuff tears in young athletes. A preliminary report. Am J Sports Med 1997;25:299-305. [Crossref] [PubMed]
- Reynolds SB, Dugas JR, Cain EL, et al. Debridement of small partial-thickness rotator cuff tears in elite overhead throwers. Clin Orthop Relat Res 2008;466:614-21. [Crossref] [PubMed]
- Ide J, Maeda S, Takagi K. Arthroscopic transtendon repair of partial-thickness articular-side tears of the rotator cuff: anatomical and clinical study. Am J Sports Med 2005;33:1672-9. [Crossref] [PubMed]
- Van Kleunen JP, Tucker SA, Field LD, et al. Return to High-Level Throwing After Combination Infraspinatus Repair, SLAP Repair, and Release of Glenohumeral Internal Rotation Deficit. Am J Sports Med 2012;40:2536-41. [Crossref] [PubMed]
- Conway JE. Arthroscopic repair of partial-thickness rotator cuff tears and SLAP lesions in professional baseball players. Orthop Clin North Am 2001;32:443-56. [Crossref] [PubMed]
- Dines JS, Jones K, Maher P, et al. Arthroscopic Management of Full-Thickness Rotator Cuff Tears in Major League Baseball Pitchers: The Lateralized Footprint Repair Technique. Am J Orthop (Belle Mead NJ) 2016;45:128-33. [PubMed]
- Rossi LA, Atala N, Bertona A, et al. Return to Sports After in Situ Arthroscopic Repair of Partial Rotator Cuff Tears. Arthroscopy 2019;35:32-7. [Crossref] [PubMed]
- Rossi LA, Atala NA, Bertona A, et al. Long-Term Outcomes After In Situ Arthroscopic Repair of Partial Rotator Cuff Tears. Arthroscopy 2019;35:698-702. [Crossref] [PubMed]
- Turman KA, Anderson MW, Miller MD. Massive rotator cuff tear in an adolescent athlete: a case report. Sports Health 2010;2:51-5. [Crossref] [PubMed]
- Alley MC, Banerjee S, Papaliodis D, et al. Transosseous Physeal-Sparing Rotator Cuff Repair in an Adolescent Football Player. Orthopedics 2016;39:e353-8. [Crossref] [PubMed]
- Eisner EA, Roocroft JH, Moor MA, et al. Partial rotator cuff tears in adolescents: factors affecting outcomes. J Pediatr Orthop 2013;33:2-7. [Crossref] [PubMed]
- Lazarides AL, Alentorn-Geli E, Choi JH, et al. Rotator cuff tears in young patients: a different disease than rotator cuff tears in elderly patients. J Shoulder Elbow Surg 2015;24:1834-43. [Crossref] [PubMed]
- Kluczynski MA, Isenburg MM, Marzo JM, et al. Does Early Versus Delayed Active Range of Motion Affect Rotator Cuff Healing After Surgical Repair? A Systematic Review and Meta-analysis. Am J Sports Med 2016;44:785-91. [Crossref] [PubMed]
- Jancuska J, Matthews J, Miller T, et al. A Systematic Summary of Systematic Reviews on the Topic of the Rotator Cuff. Orthop J Sports Med 2018;6:2325967118797891 [Crossref] [PubMed]
- Mazuquin BF, Wright AC, Russell S, et al. Effectiveness of early compared with conservative rehabilitation for patients having rotator cuff repair surgery: an overview of systematic reviews. Br J Sports Med 2018;52:111-21. [Crossref] [PubMed]
- Littlewood C, Bateman M, Clark D, et al. Rehabilitation following rotator cuff repair: a systematic review. Shoulder Elbow 2015;7:115-24. [Crossref] [PubMed]
- Zhang S, Li H, Tao H, et al. Delayed early passive motion is harmless to shoulder rotator cuff healing in a rabbit model. Am J Sports Med 2013;41:1885-92. [Crossref] [PubMed]
- Uezono K, Ide J, Tokunaga T, et al. Effect of Postoperative Passive Motion on Rotator Cuff Reconstruction With Acellular Dermal Matrix Grafts in a Rat Model. Am J Sports Med 2014;42:1930-8. [Crossref] [PubMed]
- Keener JD. Revision rotator cuff repair. Clin Sports Med 2012;31:713-25. [Crossref] [PubMed]
- Koo SS, Burkhart SS. Rehabilitation following arthroscopic rotator cuff repair. Clin Sports Med 2010;29:203-11. vii. [Crossref] [PubMed]
- Tauro JC. Stiffness and rotator cuff tears: incidence, arthroscopic findings, and treatment results. Arthroscopy 2006;22:581-6. [Crossref] [PubMed]
- Brislin KJ, Field LD, Savoie FH 3rd. Complications after arthroscopic rotator cuff repair. Arthroscopy 2007;23:124-8. [Crossref] [PubMed]
- Houck DA, Kraeutler MJ, Schuette HB, et al. Early Versus Delayed Motion After Rotator Cuff Repair: A Systematic Review of Overlapping Meta-analyses. Am J Sports Med 2017;45:2911-5. [Crossref] [PubMed]
- Rossi LA, Chahla J, Verma NN, et al. Rotator Cuff Retears. JBJS Rev 2020;8:e0039 [Crossref] [PubMed]
Cite this article as: Seiter M, Nolte PC, Elrick BP, Millett PJ. Clinical outcomes of rotator cuff repair in athletes. Ann Joint 2020;5:43.


