
Elbow contracture release
Introduction
The elbow joint encloses 3 different articulations, with distinguished functions. Flexion and extension occur through the ulnohumeral and radiocapitellar joints, while forearm pronation and supination occur through the proximal radioulnar articulation. To perform most daily activities, an arc of elbow motion of 100o (30o of extension to 130o of flexion) as well as an arc of forearm rotation of 100o (from 50o of pronation to 50o of supination) are required. Therefore, any limitation in elbow arc range of motion may result in a severely compromised arm.
There are several causes for elbow stiffness, which can be broadly classified into intrinsic and extrinsic causes. Intrinsic stiffness may be the result of posttraumatic arthritis, osteochondritis dissecans, primary osteoarthritis or inflammatory arthropathy (1,2). Extrinsic stiffness usually results from posttraumatic extra-articular soft tissue contracture (involving the capsule, collateral ligaments, surrounding tendons or even the skin), while common intrinsic causes include intra-articular loose bodies or articular incongruency. Elbow stiffness is often the result of a combination of both extrinsic and intrinsic components.
It is known that the elbow joint is highly predisposed to elbow stiffness. Although the main reason for this propensity for stiffness has not been fully elucidated, many theories have been suggested. The numerous separate articulations in one synovial joint, the high congruity between the humeral articular surface and the ulnar articular surface, and the proximity of the capsule to adjacent superficial structures such as the overlying ligaments and muscles are some of the proposed theories (3). The critical role of the joint capsule and its alternations in development of elbow stiffness has also been highlighted by many authors (4). While the capsule is normally thin and highly distensible allowing for an extensive range of motion, in cases of posttraumatic elbow stiffness the capsule usually becomes extremely thick. From the molecular standpoint, certain changes have been noted in stiff elbows, including a decrease in type III collagen synthesis, while an overexpression of cytokines and growth factors (transforming growth factor-b1, connective tissue growth factor) lead to marked myofibroblasts proliferation (5-7).
Evaluation
A thorough history is an integral part of the overall evaluation and should always address any previous elbow injury. In patients with posttraumatic elbow stiffness, surgeons should obtain a detailed history focused on the mechanism of injury and the initial treatment (8). Information about the characteristics of stiffness such as the time of initial presentation and progression must be cautiously recorded. In addition, the presence of any associated symptoms including pain, weakness, sensory deficits or any history of infection should also be noted. Any other medical conditions that may predispose to stiffness (e.g., neurological conditions or congenital syndromes) need to be recognized (8,9).
Physical examination of the elbow starts with inspection for the presence of surgical incisions, deformities, burns or any other scars due to previous trauma. Active and passive range of motion in terms of flexion-extension and pronation-supination should be carefully assessed and documented. The character of endpoint of motion and any crepitus should be recorded as well. Pain at the mid-range of elbow motion usually indicates advanced arthritis with articular incongruity and cartilage damage, whereas pain at the extremes of motion indicates impingement of osteophytes between the olecranon or the coronoid process with the distal humerus (10-12).
Tenderness or warmth, similar to painful stiffness, may indicate inflammation or active infection. To rule out infection, further assessment is indicated with measurement of inflammatory markers (erythrocyte sedimentation rate and C-reactive protein level). In patients with evidences of active infection, the elbow joint should be aspirated and synovial fluid sent for further analysis. A neurological examination must always be performed with special attention to ulnar nerve function. Electromyography and nerve conduction studies may be necessary to evaluate the extent of neural damage.
Plain radiographs including anteroposterior, lateral and oblique views are the first imaging studies for a patient with a stiff elbow. The primary bone landmarks (ulnohumeral joint, coronoid process, radial head, capitellum, radiocapitellar joint, olecranon tip, coronoid/olecranon fossae and trochlear ridge) and the overall congruity of the elbow joint are evaluated, along with signs of arthritic changes or the presence of any implants. At the early stages of primary osteoarthritis, radiographs typically show osteophyte formation around the tip of the olecranon or the coronoid process. In later stages, the radiocapitellar joint (radial head and radial fossa) and the proximal radioulnar joint are usually affected. The joint space in the ulnohumeral and radiocapitellar articulations is usually preserved and asymmetric joint narrowing is seen only in advanced stages. In cases of severe primary arthritis, subchondral sclerosis and bone cysts may also be present. The location and size of osteophytes correlates with the severity of symptoms and the presence of neurological deficits. A large medial osteophyte is associated with an increased risk for cubital tunnel syndrome. Computer tomography (CT) with three-dimensional reconstruction is also very useful and can provide valuable information regarding the location of osteophytes, as well as the presence of heterotopic ossification (13). Magnetic resonance imaging may be used to evaluate integrity of collateral ligaments.
Treatment
The goal of treatment of elbow stiffness is to restore pain free functional elbow motion. Nonoperative treatment should be considered in patients with mild elbow contractures with a duration less than 6 months. Physical therapy with passive and active exercises, dynamic and static progressive splints and continuous passive motion have been used with satisfactory results (14,15).
Patients who fail to achieve functional elbow motion with conservative treatment are candidates for operative treatment. Various surgical approaches for elbow contracture release have been described in the literature, including open or arthroscopic release, ulnohumeral arthroplasty. Each technique has its own advantages and disadvantages. The decision for the approach is based on the surgeons’ preference, taking into consideration several factors such as the extent of contracture, location of lesions, presence of hardware, previous incisions and ulnar nerve symptoms.
Regardless of the surgical technique that is used, attention should be paid to the ulnar nerve. In patients with preoperative symptoms of ulnar neuropathy at the elbow, positive Tinel test or posteromedial heterotopic ossification, an ulnar nerve release is indicated. Prophylactic release of the ulnar nerve may be advisable in patients with <100o of preoperative elbow flexion (extension contractures) (16).
Surgical treatment of elbow stiffness should address any contracture around the joint that prevents elbow flexion-extension and forearm supination-pronation. In order to restore elbow flexion, the contracted structures on the posterior aspect of the elbow such as the posterior capsule and the distal part of triceps must be released. Moreover, any mechanical block that prevents full elbow flexion including osteophytes over the coronoid process, bony overgrowth in the anterior distal humeral fossae, and anterior loose bodies should be removed. Conversely, limitation in elbow extension is usually caused by a contracted anterior capsule or by osteophytes on the tip of the olecranon that cause impingement with the humeral olecranon fossa. Any hardware that interferes with the range of motion should also be removed. Finally, periarticular heterotopic ossification and calcified collateral ligaments must be addressed accordingly. Posttraumatic ligament calcification represents a different type of calcification than heterotopic ossification (17). In most cases, sole resection of the calcified posterior band of the medial collateral ligament (MCL) without release of the anterior band is sufficient for restoration of range of motion. However, in more severe cases with ankylosis and extensive calcification of the collateral ligaments, these ligaments may require complete resection. When marked elbow instability is noted intraoperatively after resection of the collateral ligaments, reconstruction of the collateral ligaments may be warranted.
Arthroscopic release
Elbow contractures can be managed with arthroscopic release allowing visualization of the anterior and posterior compartment of the elbow joint. Ideal indications include cases with limited bony impingement or when stiffness is secondary to capsular tightness. Elbow contractures with extensive heterotopic ossification, severe arthritis, or marked muscular contracture are usually difficult to be addressed arthroscopically. Elbow arthroscopy is relatively contraindicated when there is a history of elbow trauma or ulnar nerve transposition due to the altered anatomy of the elbow.
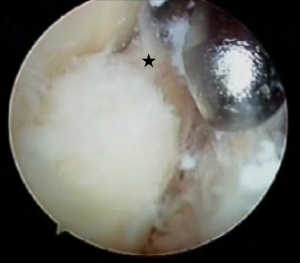
The patient can be placed in a prone, supine or lateral position for arthroscopy of the elbow. Bony and soft tissue landmarks and the location of the ulnar nerve are marked before the procedure begins. The elbow joint is initially distended with saline solution that is injected through the lateral soft spot. Through distension, the neurovascular structures are also moved further away from the portal sites. The anterolateral, anteromedial or any accessories portals are established. The order of the portals depends of the preference of the surgeon and the pathology to be addressed. With the aid of an arthroscopic grasper and a shaver, any loose bodies in the anterior compartment of the elbow are removed, while thick synovial or fibrotic tissue can be debrided. Usually a small burr is used to remove any osteophytes from the radial head or the coronoid fossa (Figure 1). Then the capsule can be released starting from lateral to medial. Accessory portals and additional use of retractors are recommended in many cases in order to improve visualization, facilitate the capsular release and protect the neurovascular structures.
The posterior compartment of the joint is addressed after completion of the anterior compartment. Many portals can be used for visualization of the posterior elbow compartment including a direct posterior, posterolateral and direct lateral or midlateral portal. First, any fibrotic and synovial tissue from the posterior compartment is resected, while loose bodies are removed to allow better visualization of the posterior joint. On the medial side of the joint, during debridement of the posteromedial gutter attention is paid to avoid injury of the ulnar nerve, which may be protected by a retractor. A burr or small osteotome is used for resection of osteophytes around the olecranon and the olecranon fossa.
Arthroscopic elbow contracture release seems to be a valid technique for restoration of a functional range of motion with satisfactory results by many authors (18,19). However, this is a demanding procedure requiring a high level of arthroscopic skill to avoid nerve injury. The use of retractors for improved visualization is suggested for prevention of neurovascular iatrogenic injury.
Open release
Several approaches including an anterior, posterior, lateral and medial approach have been proposed. The most commonly used approaches that provide access to both anterior and posterior sides of the elbow with successful results are the lateral and medial approach. Although a single approach is usually sufficient for a complete elbow release, a dual procedure, combining a medial and a lateral approach, can be performed to address all relevant pathology.
Lateral approach
The lateral approach is indicated for release of elbow contracture with anterior and/or posterior capsule and articular involvement (20-22). It allows exposure of the anterior and posterior compartments, however, a significant drawback of this approach is the inaccessibility of the ulnar nerve. For the lateral approach, a 10 cm skin incision is made along the course of the lateral supracondylar ridge of the humerus proximally up to the radial head distally. Deep dissection uses the interval between the lateral supracondylar ridge and the brachioradialis (BR) and extensor carpi radialis longus (ECRL) proximally and the anconeus and the extensor carpi ulnaris (ECU) distally. During the lateral approach, attention must be paid to protect and preserve the lateral collateral ligament complex, which is located posterior to the extensor carpi radialis brevis (ECRB) (23,24). The anterior capsule is exposed, retracting anteriorly the BR and the ECRL, while the radial head is exposed between the anconeus and the ECU. Then, the anterior capsule is released from lateral to medial with care to avoid neurovascular injury to the radial or median nerve and the brachial artery. The radiocapitellar joint must be cautiously evaluated for any loose bodies or proliferative synovitis. Any loose bodies or osteophytes from the coronoid or the distal humerus must be removed. In cases of limited supination-pronation, the proximal radioulnar joint should be also evaluated for spurs or incongruity, while adhesions between radial head and annular ligament should be released. In cases of osteoarthritis, if the radial head excision is indicated this can be performed through the same incision.
In elbow contracture cases with posterior pathology and not full extension, an additional release of the posterior compartment of the elbow is needed through the lateral approach. The triceps is detached from the posterior humeral cortex and the posterior capsule is exposed and released. Any loose bodies in the olecranon fossa or olecranon osteophytes can then be resected. The completion of the debridement of the anterior and posterior part of the joint is followed by the manipulation of the elbow with a short lever arm to lyse any remaining adhesions and achieve more motion.
Several authors reported an average elbow arc improvement of 40o to 70o after elbow contracture release with the lateral approach (20-22,24,25). Studies have described better improvement of elbow extension than elbow flexion with this technique.
Medial approach
The medial approach can be used for the surgical treatment of patients with elbow contracture involving pathology of the medial aspect, such as contracted posteromedial ulnohumeral joint capsule, heterotopic bone or ulnar nerve involvement (21,26). This approach allows easy access to the anterior and posterior part of elbow joint and release of the ulnar nerve. A disadvantage of the medial approach though is that the lateral side of the elbow is not accessed, thus the commonly present lateral pathology cannot be addressed.
The skin incision for the medial approach starts 5 cm proximal to the elbow at the level of medial intermuscular septum, curves posterior to the medial epicondyle and ends 5 cm distally in the proximal forearm. Following skin incision, subcutaneous dissection is carried out carefully to avoid any damage to the sensory branches of the medial antebrachial cutaneous nerve that are located superficial to the forearm fascia. Full thickness adipocutaneous flaps are developed and elevated for adequate exposure of the flexors-pronator origin. The ulnar nerve is released along its course from the medial intermuscular septum proximal to its insertion between the two heads of flexor capris ulnaris distally and is usually transposed anteriorly. In case of previous ulnar nerve decompression, exposure of the nerve should begin proximal to the operated area. The anterior capsule is exposed using the interval between the pronator teres and the flexor carpi radialis. The anterior capsule, which in some cases may be extremely thick, is carefully excised from medial to lateral protecting the neurovascular bundles. Once the anterior articular surface is clearly visible, anterior osteophytes from the coronoid process can be debrided and any loose bodies can be removed. On the posterior elbow, the distal humerus is exposed by mobilizing and raising the triceps off the humerus. Once the posterior capsule is fully exposed it is released, providing access to the olecranon fossa of the distal humerus. Any fibrous tissue, osteophytes or loose bodies around the olecranon fossa, and the tip of the olecranon can be excised.
During the dissection of the medial approach, care is taken to protect and preserve the anterior oblique band of the MCL to avoid postoperative instability. After completion of the posterior, medial and anterior release, the elbow is manipulated in a similar fashion to the lateral approach. Successful results with an average improvement of 40o–65o of elbow arc have been reported using the medial approach (20,26).
Anterior approach
Elbow extension can be restored through the anterior approach, which was first described by Urbaniak et al. (27). This approach is recommended when there is solely flexion contracture, elbow flexion is full and the posterior compartment of the joint has no signs of pathology. Better results are achieved with this approach when it is used in patients without articular (intrinsic) involvement. Through a lazy-s incision along the elbow flexion crease, 2 intervals are created to protect the neurovascular structures. The medial interval is developed between the common flexor origin and biceps tendon, and the lateral interval between the biceps and BR muscle. Attention must be paid to protect all of the adjacent neurovascular structures, including the medial and lateral antebrachial cutaneous nerves, the median, radial, and musculocutaneous nerve, as well as the brachial artery. Following the development of the intervals, dissection between the brachialis and the anterior capsule is performed, medially to laterally. At this point the anterior capsule is fully exposed and released. Additional removal of any ectopic bone in the anterior part of the elbow is also performed.
Posterior approach
Medial and lateral releases can be performed with the posterior approach, through two windows lateral and medial of the triceps tendon. First, a midline posterior skin incision is made and two full thickness fasciocutaneous flaps (medially and laterally) are developed. On the medial side, the ulnar nerve is released followed by anterior transposition. The triceps tendon can then be managed with various techniques such as reflection (Bryan-Morrey approach), split (Campell), or preservation (paratricipital approach Alonso-Llames). This approach can be also used for the interposition arthroplasty.
Ulnohumeral arthroplasty or Outerbridge - Kashiwagi procedure
The ulnohumeral arthroplasty or Outerbridge - Kashiwagi procedure, can be used in patients with mild or moderate elbow osteoarthritis or posttraumatic arthritis with pain in terminal extension or flexion (or both). This surgical procedure is based on a posterior approach to the elbow and through a fenestration of the olecranon fossa, permits capsule release and removal of loose bodies and osteophytes from the posterior (olecranon or olecranon fossa) and anterior (coronoid process or coronoid fossa) compartment of the elbow. This technique can be performed either open or arthroscopically (28-32).
In the open technique, first the posterior aspect of the elbow joint is addressed through a straight posterior incision. Care is taken to identify and protect the ulnar nerve. The posterior compartment of the elbow is exposed, splitting longitudinally or reflecting the triceps tendon medially or laterally. Then a capsulotomy is performed and any loose bodies and osteophytes from the olecranon or olecranon fossa can be resected. Then the anterior elbow compartment is exposed through a hole that is drilled in the olecranon fossa (foraminectomy) with the use of a dowel. Attention should be paid to the proper placement of the foraminectomy of the olecranon fossa to avoid fracture of the humerus. With maximum elbow flexion, any loose bodies of the anterior compartment and any osteophytes from the coronoid process can be removed. An anterior capsular release can also be performed through the foraminectomy.
In the arthroscopic technique, the arthroscope is introduced through an anterolateral portal into the anterior compartment of the elbow and an anteromedial portal is established. With the use of an arthroscopic grasper and an arthroscopic shaver any loose bodies can be removed and debridement of the anterior aspect of the elbow can be performed. This is usually performed in combination with anterior capsule release. Then a standard posterolateral and posterior central portal are established. Through the posterior central portal, removal of loose bodies from the posterior aspect of the elbow and debridement of spurs from the olecranon fossa and can be performed. To fenestrate the olecranon fossa, a drill is inserted through the posterior central portal and a drill hole is created from posterior to anterior into the center of the olecranon fossa. Through the hole any osteophyte from the coronoid process can be removed using an arthroscopic burr with maximum elbow flexion.
A review of the literature shows satisfactory results in over 80% with open or arthroscopic technique (28-32). Comparative studies between the open and arthroscopic techniques demonstrated no statistically significant difference in overall effectiveness.
Our current technique
Our preferred technique for the management of elbow stiffness involves a combined approach, including a lateral and a minimal posterior triceps splitting approach (33). Initially, a limited lateral incision running over the supracondylar ridge proximally up to the radial head distally is performed. To expose the anterior capsule, the BR and ECRL are released off the anterior aspect of the supracondylar ridge. Dissection proceeds between the ECRB and ECRL distally, with care to avoid disruption of the lateral ulnar collateral ligament. The brachialis is retracted anteriorly and the capsule is fully exposed. The capsule is cautiously released from lateral to medial with care to avoid any neurovascular structures. Any osteophytes and loose bodies on the anterior aspect of the elbow joint and around the coronoid are debrided. Although not common, in cases of severe arthritis involving the radiocapitellar joint with painful forearm rotation, the radial head may be resected. On the posterior elbow, a midline incision is made with the elbow flexed in 45°. The posterior capsule is exposed through a longitudinal split of the triceps tendon. Once fully exposed, the posterior capsule is released and the posterior joint is accessed. Osteophytes around the olecranon are debrided, and any loose bodied on the posterior part of the joint are removed. If needed, the posterior band of the MCL can be addressed through the posterior incision. After completion of the anterior and posterior releases, careful manipulation of the elbow is carried out with a short lever arm to maximize the total range of flexion-extension. Postoperatively, a removable posterior long-arm splint is applied and elbow range of motion exercises are started within the first week.
This combined approach is simple and effective, as exposure of the posterior joint through the posterior approach is extremely advantageous considering release in this area is not adequate through the lateral approach. An average improvement of 55°–60° in the elbow range of motion was noted in our patients (33).
Rehabilitation
There is a wide variation among surgeons in the rehabilitation protocols following arthroscopic or open management of elbow stiffness. The aim of the rehabilitation protocol is mainly to maintain the range of motion that was achieved intraoperatively and address edema. Every program is initially based on passive and active stretching exercises of the elbow and forearm. This requires low levels of pain, therefore pain management is an extremely important part of the postoperative rehabilitation. In some cases, with suboptimal maintenance of the postoperative range of motion, a dynamic splint that passively extends or flexes the elbow can be used. If indicated, this dynamic splint is usually applied several times during the day and each session should last 15–20 minutes. Also, a turnbuckle splint may be used to control flexion or extension. In severe cases with inadequate elbow extension, a nocturnal static extension splint is recommended. Another modality that is commonly recommended by many authors is continuous passive motion. Although it can be useful in certain cases, great caution is warranted due to risk for neurologic injury or wound dehiscence (2,20,22,24). It must also be noted that there is no direct correlation between the achieved range of motion during continuous passive motion sessions and the actual elbow range of motion. Repetitive evaluation by the surgeon is necessary during the postoperative period, since the rehabilitation program must be individualized and can be modified according to each patient’s progress. Usually the postoperative rehabilitation program and dynamic splinting should last for at least 3 months.
Results
Many studies have shown that the arthroscopic and open surgical management for elbow stiffness provide a functional range of motion that is needed for the daily and working activities (18-33). However, no studies have shown advantages of the improvement in motion with the arthroscopic release when compared with open techniques (34). It is not clear if a previous elbow surgery is correlated with worse outcomes after surgical release for elbow stiffness (35-39). Although surgical release for extrinsic elbow stiffness in children and adolescent patients usually yield similar results as in adults, the results are not as consistent for patients 10–20 years when compared to older patients (40). Additionally, the range of motion that is achieved intraoperatively in these young patients is usually decreased by 25% during the following months (40). Although the cause for this loss is not fully elucidated, it has been suggested that less strict compliance with the postoperative protocol and a more active healing process in younger patients may explain the tendency for recurrent contracture. Along with improvement in range of motion, which is the main purpose of surgery, patients commonly reported a marked improvement in pain, which is of great significance as pain level is one of the most integral parts for evaluation of the overall health status and for functional scores (41).
Conclusions
Elbow contracture release represents a challenging clinical problem. The main goal of surgical elbow contracture release is to provide a functional arc of elbow motion. The surgical management of a stiff elbow must be individualized, taking into consideration many factors including the cause for stiffness, the patient’s age, the presence of heterotopic ossification, the extent of articular wear and functional demands. Various procedures with arthroscopic and open techniques have been described with satisfactory outcomes. However, to determine the relative risks, benefits and outcomes of each technique, further study is necessary with prospective comparison trials.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Spencer P. Lake) for the series “Emerging Trends in Elbow Injury, Pathology and Treatment” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-19-180). The series “Emerging Trends in Elbow Injury, Pathology and Treatment” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Aldridge JM III, Atkins TA, Gunneson EE, et al. Anterior release of the elbow for extension loss. J Bone Joint Surg Am 2004;86:1955-60. [Crossref] [PubMed]
- Morrey BF. The posttraumatic stiff elbow. Clin Orthop Relat Res 2005.26-35. [Crossref] [PubMed]
- Cohen MS. Open capsular release for softtissue contracture of the elbow. In: Yamaguchi K, King GJW, McKee M, et al. editors. Advanced Reconstruction: Elbow. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2007:195-204.
- O’Driscoll SW, Morrey BF, An KN. Intraarticular pressure and capacity of the elbow. Arthroscopy 1990;6:100-3. [Crossref] [PubMed]
- Hildebrand KA, Zhang M, Van Snellenberg W, et al. Myofibroblast numbers are elevated in human elbow capsules after trauma. Clin Orthop Relat Res 2004.189-97. [Crossref] [PubMed]
- Cohen MS, Schimmel DR, Masuda K, et al. Structural and biochemical evaluation of the elbow capsule after trauma. J Shoulder Elbow Surg 2007;16:484-90. [Crossref] [PubMed]
- Hildebrand KA, Zhang M, Hart DA. Myofibroblast upregulators are elevated in joint capsules in posttraumatic contractures. Clin Orthop Relat Res 2007.85-91. [Crossref] [PubMed]
- O’Driscoll SW. Clinical assessment and open and arthroscopic surgical treatment of the stiff elbow. In: Jupiter JB, editor. The stiff elbow. 1st ed. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2006:9-19.
- Morrey BF. The stiff elbow with articular involvement. In: Jupiter JB, editor. The stiff elbow. 1st ed. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2006:21-30.
- Viola RW, Hastings H 2nd. Treatment of ectopic ossification about the elbow. Clin Orthop Relat Res 2000.65-86. [Crossref] [PubMed]
- Schneeberger AG, Adams R, Morrey BF. Semiconstrained total elbow replacement for the treatment of post-traumatic osteoarthrosis. J Bone Joint Surg Am 1997;79:1211-22. [Crossref] [PubMed]
- Chammas M. Post-traumatic osteoarthritis of the elbow. Orthop Traumatol Surg Res 2014;100:S15-24. [Crossref] [PubMed]
- Zubler V, Saupe N, Jost B, et al. Elbow stiffness: Effectiveness of conventional radiography and CT to explain osseous causes. AJR Am J Roentgenol 2010;194:W515-20. [Crossref] [PubMed]
- Shewring DJ, Beaudet M, Carvell JE. Reversed dynamic slings: results of use in the treatment of post-traumatic flexion contractures of the elbow. Injury 1991;22:400-2. [Crossref] [PubMed]
- Green DP, McCoy H. Turnbuckle orthotic correction of elbow-flexion contractures after acute injuries. J Bone Joint Surg Am 1979;61:1092-5. [Crossref] [PubMed]
- Williams BG, Sotereanos DG, Baratz ME, et al. The contracted elbow: is ulnar nerve release necessary? J Shoulder Elbow Surg 2012;21:1632-6. [Crossref] [PubMed]
- Cohen MS. Heterotopic ossification of the elbow. In: Jupiter J, editor. The Stiff Elbow. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2006:31-40.
- Adams JE, Wolff LH III, Merten SM, et al. Osteoarthritis of the elbow: Results of arthroscopic osteophyte resection and capsulectomy. J Shoulder Elbow Surg 2008;17:126-31. [Crossref] [PubMed]
- Cohen AP, Redden JF, Stanley D. Treatment of osteoarthritis of the elbow: A comparison of open and arthroscopic debridement. Arthroscopy 2000;16:701-6. [Crossref] [PubMed]
- Mansat P, Morrey BF. The column procedure: A limited lateral approach for extrinsic contracture of the elbow. J Bone Joint Surg Am 1998;80:1603-15. [Crossref] [PubMed]
- Vardakas DG, Varitimidis SE, Goebel F, et al. Evaluating and treating the stiff elbow. Hand Clin 2002;18:77-85. [Crossref] [PubMed]
- Husband JB, Hastings H II. The lateral approach for operative release of posttraumatic contracture of the elbow. J Bone Joint Surg Am 1990;72:1353-8. [Crossref] [PubMed]
- Cohen MS, Bruno RJ. The collateral ligaments of the elbow: Anatomy and clinical correlation. Clin Orthop Relat Res 2001.123-30. [Crossref] [PubMed]
- Cohen MS, Hastings H II. Post-traumatic contracture of the elbow: Operative release using a lateral collateral ligament sparing approach. J Bone Joint Surg Br 1998;80:805-12. [Crossref] [PubMed]
- Kraushaar BS, Nirschl RP, Cox W. A modified lateral approach for release of posttraumatic elbow flexion contracture. J Shoulder Elbow Surg 1999;8:476-80. [Crossref] [PubMed]
- Weiss AP, Sachar K. Soft tissue contractures about the elbow. Hand Clin 1994;10:439-51. [PubMed]
- Urbaniak JR, Hansen PE, Beissinger SF, et al. Correction of post-traumatic flexion contracture of the elbow by anterior capsulotomy. J Bone Joint Surg Am 1985;67:1160-4. [Crossref] [PubMed]
- Sarris I, Riano FA, Goebel F, et al. Ulnohumeral arthroplasty: results in primary degenerative arthritis of the elbow. Clin Orthop Relat Res 2004.190-3. [Crossref] [PubMed]
- Minami M, Kato S, Kashiwagi D. Outerbridge-Kashiwagi’s method for arthroplasty of osteoarthritis of the elbow: 44 elbows followed from 8-16 years. J Orthop Sci 1996;1:11-6. [Crossref]
- Papatheodorou LK, Payatakes AH, Giannoulis FS, et al. Ulnohumeral (Outerbridge-Kashiwagi) Arthroplasty. In: Wiesel SW, Ramsey M, Wiesel B, et al. editors. Operative Techniques in Orthopaedic Surgery, 2 edition. Wolters Kluwer, Lippincott Williams & Wilkins. 2015:3933-9.
- Antuña SA, Morrey BF, Adams RA, et al. Ulnohumeral arthroplasty for primary degenerative arthritis of the elbow: Long-term outcome and complications. J Bone Joint Surg Am 2002;84:2168-73. [Crossref] [PubMed]
- Krishnan SG, Harkins DC, Pennington SD, et al. Arthroscopic ulnohumeral arthroplasty for degenerative arthritis of the elbow in patients under fifty years of age. J Shoulder Elbow Surg 2007;16:443-8. [Crossref] [PubMed]
- Kruse KK, Papatheodorou LK, Weiser RW, et al. Release of the stiff elbow with mini-open technique. J Shoulder Elbow Surg 2016;25:355-61. [Crossref] [PubMed]
- Kodde IF, Van Rijn J, Van den Bekerom MP, et al. Surgical treatment of post-traumatic elbow stiffness: A systematic review. J Shoulder Elbow Surg 2013;22:574-80. [Crossref] [PubMed]
- Koh KH, Lim TK, Lee HI, et al. Surgical treatment of elbow stiffness caused by post-traumatic heterotopic ossification. J Shoulder Elbow Surg 2013;22:1128-34. [Crossref] [PubMed]
- Baldwin K, Hosalkar HS, Donegan DJ, et al. Surgical resection of heterotopic bone about the elbow: An institutional experience with traumatic and neurologic etiologies. J Hand Surg Am 2011;36:798-803. [Crossref] [PubMed]
- Brouwer KM, Lindenhovius AL, de Witte PB, et al. Resection of heterotopic ossification of the elbow: A comparison of ankylosis and partial restriction. J Hand Surg Am 2010;35:1115-9. [Crossref] [PubMed]
- Cikes A, Jolles BM, Farron A. Open elbow arthrolysis for posttraumatic elbow stiffness. J Orthop Trauma 2006;20:405-9. [Crossref] [PubMed]
- Wada T, Ishii S, Usui M, et al. The medial approach for operative release of post-traumatic contracture of the elbow. J Bone Joint Surg Br 2000;82:68-73. [Crossref] [PubMed]
- Stans AA, Maritz NG, O’Driscoll SW, et al. Operative treatment of elbow contracture in patients twenty-one years of age or younger. J Bone Joint Surg Am 2002;84:382-7. [Crossref] [PubMed]
- Lindenhovius AL, Doornberg JN, Ring D, et al. Health status after open elbow contracture release. J Bone Joint Surg Am 2010;92:2187-95. [Crossref] [PubMed]
Cite this article as: Papadopoulos D, Papatheodorou LK, Sotereanos DG. Elbow contracture release. Ann Joint 2021;6:7.


