Magnesium and osteoarthritis: from a new perspective
Introduction
Osteoarthritis (OA) is a multi-factor induced musculoskeletal disorder with low self-repairing ability due to its dense extracellular matrix (ECM) with sparsely distributing blood vessels, nerves, stem cells and highly specialized cells called chondrocytes. Among all the risk factors related to OA, such as local risk factors (muscle weakness, excess physical activities, joint injury, mal-alignment of joint, leg length inequality etc.), modifiable systemic risk factors (obesity, unhealthy diets), non-modifiable systemic risk factors (age, gender, ethnicity, genetics), age is one of the strongest predictors of OA (1,2).
In China, the largest developing country with a population of 1.3 billion in the world, had already entered into the aged society since 2010 with 25.3% of the population comprised individuals aged 50 years or older (3). Based on the uniformed inclusion criteria and quantitative index, which including 6,218 questionnaires and 5,334 sample X-ray films, the prevalence rate of primary OA was 48.7% (1,086/2,230) in 50–59 years, 62.2% (754/1,213) in 60–69 years and was 62.1% (391/630) in 70 years and over in China 2010 (4). It can be foreseen that the prevalence of age-related OA will be fast growing in the near future in China, and the efficacious preventing and treatment ways for OA would be in great demanding in the next decades. It urges us to understand the mechanism of age-related OA which is still poorly understood. Disturbed biomechanical practices and weak muscle strength, with biological changes such as enduring inflammation, as well as chondrocytes malfunction and inferior self-renewing capability of cartilage progenitor cells are likely combined contributing factors in age-related OA (5). Nevertheless, very few insights had been put into the tissue mineral changes in cartilage metabolism. For example, calcium (Ca), magnesium (Mg), sodium (Na), potassium (K), selenium (Se), zinc (Zn), copper (Cu), and iron (Fe) are well contained in the joint tissue and play respective roles in cartilage normal function and progress of OA and rheumatoid arthritis (RA) (6,7). Mg is an important element which had been overlooked in the musculoskeletal disorders for a long time until the significant osteogenic effect of Mg is reported in recent years (8-10).
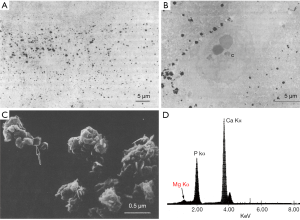
In articular cartilage, it is distributing with some tiny minerals in this non-mineralized hard tissue. Mg is considered existing in the hyaline cartilage matrix as Mg-substituted tricalcium phosphate (TCP) commonly named whitlockite [(Ca,Mg)3(PO4)2)] (11-13). These cuboid crystals have been described in both normal and pathologic articular cartilage tissues determined by electron and X-ray diffraction. Its frequent existence in cartilage tissue bring questions about Mg’s role in cartilage generation, physiological cartilage metabolism and pathogenicity in OA cartilage (14).
It was reported that Mg-deficiency in young rodents elicited an apparent decrease in the number and the size of the proximal tibial articular chondrocytes with a statistically significant decrease in the width of the articular cartilage (15). It also showed a lack of the orderly chondrocyte columns arrangement, a reduction in the proteoglycans amount and a statistically significant decrease of width in growth plate of the proximal tibia, as well as a highly significant decrease of the trabecular bone volume and a statistically significant decrease of the osteoblastic surface in the proximal metaphysis of the tibia (15). Some other studies had been found that Mg deficiency in immature dogs/rats led to significant cartilage lesions with distinct alterations in ultrastructure and chondrocytic fibronectin staining (16-18). Histomorphometry demonstrated significantly decreased distal femur articular cartilage chondrocyte density and decreased tibia growth plate width in experimental animals compared to controls, ECM of both articular cartilage and growth plates in experimental animals contained reduced amounts of proteoglycans and reduced levels of SOX9 in rats following a 6-month dietary Mg restriction (19). Within a relative short time of Mg intake restriction (28 days), cartilage lesion was observed in juvenile rats rather than in aged rats (20,21). In human beings, several epidemiological studies reported that serum Mg (Mg intake) was inversely and significantly associated with radiographic knee OA, joint space narrowing (JSN) and RA (22-25). All the studies strongly indicate a potential role of Mg in the genesis and prevention of OA.
Here we details the topic about the pivotal role of Mg in pathogenesis and prevention of OA by reviewing the main published Mg-related studies in OA, RA, cartilage and bone metabolism.
Existence of Mg in the cartilage tissue
Ca phosphate crystals, including hydroxyapatite, carbonated apatites, octacalcium phosphate and Mg-substituted whitlockite have been reported in human articular cartilage and synovial fluid (11,26-28). In contrast to Mg-substituted whitlockite, the other Ca containing crystals with high Ca/P ratio in cartilage and periarticular tissue was strongly associated with osteoarthritic reaction and degenerative joint disease (11,14). For instance, articular deposition of basic Ca phosphate [(BCP), a term restricted to various mixtures of carbonate substituted apatite, octacalcium phosphate, and TCP] is associated with an exaggerated form of OA (14,29,30). In addition, Ca pyrophosphate dihydrate (CPPD) crystal deposition disease affects articular cartilage and is a frequent concomitant of severe OA (30). These crystals stimulate synthesis and secretion of cytokines and proteases by phagocytic cells like synovial lining cells and chondrocytes. They also induce mitogenesis in synovial lining cells, thereby increasing the number of cells able to secrete cytokines and proteases in response to crystals shed into the joint fluid (14).
The Ca moiety in BCP and CPPD crystals appears to play the important roles in eliciting biologic responses by phagocytic cells. Particulates that do not contain Ca do not stimulate mitogenesis after phagocytosis (14). Whitlockite appears to share some of the same biologic properties, such as enhancing mitogenesis and synthesis and secretion of matrix metalloprotease 1 and 3 (MMP1 and MMP3) of phagocytic cells in response to these crystals (14). However, the biologic responses to whitlockite are attenuated compared with Ca-containing crystals that are devoid of Mg. Mitogenesis and proteases synthesis induced by whitlockite, which has approximately 9.2% atomic substitution of Mg for Ca, is less than that induced by the Mg-free β-TCP (14).
Potential explanations for the reduced mitogenesis and proteases synthesis of phagocytic cells in response to the whitlockite crystals may be due to the interference of Mg with the early and rapid cytosolic influx of Ca by lessening crystal-membrane interactions, or interference with mitogen-activated protein (MAP) kinase induction and MAP kinase cascade (14). However, the postulation has not been proven by detailed research experiments yet. What have been known by now is that Mg ions have direct inhibiting effect on aberrant mineralization of Ca rich crystals (Figure 1).
Redeeming effect of Mg2+ on chondrotoxicity caused by chondrocalcinosis
Researchers have explored the role of the Mg ions in biomineralization for decades. In 1984, Nancollas (31) found that Mg2+ appreciably retard the OCP growth rate and strongly inhibit thermodynamically stable hydroxyapatite crystallization (32,33). They further proved that Mg2+ at concentrations ranging from 0.0099 to 0.99 mM reduce the hydroxyapatite growth rate by 51% and 93% (32). After finding that inhibitory effect of Mg2+ is enhanced by synergization with CO3 anions, Cao proposed that Mg2+ induce a significant inhibitory effect on the larger crystal growth of hydroxyapatite by forming a surface complex at the active growth site of newly formed small hydroxyapatite crystals and bonding to small crystals to prevent unceasing precipitation of Ca-P (34,35). It has been suggested that Mg2+ kinetically hinders nucleation and subsequent growth of hydroxyapatite by competing for structural sites with chemically similar but larger Ca2+ (31,36).
Mg deficiency in cartilage tissue would lead to the Ca-rich BCP, CPPD and finally hydroxyapatite crystallization, which is characterized as articular chondrocalcinosis commonly occur in elderly people with OA (37,38).
Typical observations of Mg deficiency induced cartilage lesion includes (I) bundle-shaped, electron-dense aggregates on the surface and in the cytoplasm of chondrocytes; (II) detachment of the cell membrane from the matrix and necrotic chondrocytes; (III) reduction of the ECM; and (IV) swelling of cell organelles such as mitochondria (16-18). These electron-dense, bundle-like aggregates occurring physiologically in the pericellular spaces from proliferating chondrocytes is prone to be the Ca containing BCP and CPPD crystals (18). The synovial lining cells producing inflammation factors such as tumor necrosis factor α (TNF-α) which is known to induce interleukin 1 (IL-1) and their synergistic effects have been described in the cartilage tissue with Mg deficiency may be caused by the BCP and CPPD crystals (39,40). The released cytokines cause the impairment of proteoglycan synthesis, chondrocytes injury and breakdown of cartilaginous matrix by induction of MMPs. In accordance with this mechanism, increased plasma levels of IL-1 and TNF-α are also observed in Mg-deficient rats compared to controls (39,40). In Mg deficient state, after triggering the inflammatory response cascades, elevation of TNF-α would promote the release of IL-6 and interferons, synthesis of nitric oxide (NO), substance P (SP) and IL-4. Immune cells and synovial cells would be activated and stimulate the production of prostaglandins and several cytokines which synergetically involved in inflammation (31,37).
The character of tissue lesion of Mg-deficiency induced cartilage is similar with that after cartilage toxicant quinolone treatment in rats (18). It is also reported that quinolone-induced chondrotoxicity is possibly associated with the Mg-chelating properties of quinolones. Mg2+ can bind to the drugs of quinolone class, thus reducing the concentration of biologically active ionized Mg2+ in the cartilage tissue (18). It indicates that Mg2+ concentration disturbance in local cartilage tissue could be one of the chief pathogenic causes in the arthropathy process.
Mg is the fourth abundant cation in the body and the second most common intracellular cation after potassium. It plays important roles in animals as a central ion of adenosine triphosphatase (ATPase) and making it pivotal for numerous physiological functions (41,42). Mg2+ is required for a very wide range of cellular reactions, including all phosphoryl transfers related to DNA and protein synthesis. The increase in cytosolic free Mg2+ which initiated by the binding of growth factors to their receptors in the cell membrane leads to up regulation of Mg− adenosine triphosphate (ATP) 2− which accounts for the downstream protein synthesis of the phosphatidylinositol (PI) 3-kinase cascade, promotes cell mitosis and proliferation (43). The importance of cytosolic Mg2+ for cell proliferation is explained via the membrane, cytosolic Mg2+, mitosis model (MMM) (44,45). However, cytosolic Mg2+ affects chondrocytes and cartilage progenitors not only on the cell proliferation and viability, but also on their chondrogenic differentiation.
Profitable effect of Mg2+ on chondrocytes viability and chondrogenic differentiation
The addition of magnesium sulfate (MgSO4) along with local anesthetic agents was found resulted in greater human chondrocytes viability than when cells are treated with a local anesthetic alone (46). In another study, chondrocytes were cultivated in the presence of quinolones and in Mg-free medium show severe alterations in cytoskeleton and decreased ability to adhere to the culture dish (32). With Mg2+ supplementation, the number of attached cells increased to 40–70% that of control cells in Mg-free medium (32). Human chondrocytes viability is greater in the presence of Mg2+ than selected local anaesthetics, this effect possibly is due to the antagonizing character of Mg2+ to chondrocyte NMDA-receptor which mediating cytosolic Ca2+ evoking (33,47). In studies of Dou et al., after incubating pure metal Mg microspheres with chondrocytes, glycosaminoglycans (GAG) content, collagen type I/II/X and aggrecan were significantly increased in chondrocytes under proper concentration of Mg2+ conditions (48). Meanwhile, AH Martínez-Sánchez found that Mg extracts could induce human umbilical cord perivascular cells (HUCPCs) which exhibiting a high mesenchymal stem cell potential, differentiate into chondrocytes with type II collagen (COL2A1), aggrecan, SOX9 up regulated, and synthesis of cartilage-like ECM (49).
In our study, high concentration of Mg ions (from 2 to 10 mM) promotes osteogenic and chondrogenic but rather than adipogenic differentiation of tendon-derived stem cells (TDSCs) and bone marrow stem cells (BMSCs) in respective inducing medium in vitro. This phenomenon is jointly corporate with high cellular ATP production. To be noticed, the stem cell didn’t undergo differentiation in simple Mg containing medium (without the inducing ingredients in the medium). Our findings are in accordance with other groups in certain extent (50-52). For example, Feyerabend et al. found Mg concentrations up to 10 mM lead to an increase of the proliferation rate, higher degree of chondrocyte differentiation with increased GAG production, the absence of collagen type I (COL1A1) gene expression and higher melanoma inhibitory activity (MIA) expression (51). Yoshizawa et al. also found that osteogenic differentiation of BMSCs is enhanced at 5 and 10 mM MgSO4, and collagen type X mRNA (COL10A1, an ECM protein deposit during bone healing and hypertrophic process in chondrocytes) expression is increased at 10 mM MgSO4 in both medium with and without osteogenic factors (53). It also found that Mg2+ profoundly enhances alkaline phosphatase (ALP) gene expression and osteogenic differentiation activity in hBMSCs even at a relatively low concentration (2.5 mM) (54). In Zheng’s group, Mg ions were found to enhance the proliferation and redifferentiation of chondrocytes and the osteogenic differentiation of osteoblasts at specific concentrations, respectively (52). These studies show that besides its favorable effect to chondrocyte viability, Mg2+ also performs the promoting effect on stem cells differentiation. Overall, the predominant action of cellular Mg is related to ATP utilization, and thus it exists in all cells primarily as Mg-ATP (55). Through interaction with universally required ATP in cell, Mg may influence most life metabolic processes including cartilage and bone modeling (56).
All the effects of Mg ions on stem cells, chondrocytes, osteoblast, osteoclasts and other lining cells such as fibroblasts and T cells may share a common mechanism based on cytosolic Mg2+ actions. We notice that along with Mg2+ entering into the cytoplasm, cellular ATP content is augmenting in our recent study (57). After incubating with high concentration Mg2+, stem cells enhance its adhesion to the substrate with focal adhesion kinase (FAK) phosphorylated in first 24 hours. Then in the following 1 to 2 weeks, stem cells are programmed into chondrogenic and osteogenic differentiation. In contrast to Ca2+, which is responsible for fast cellular reactions, Mg shows gradually and very well controlled, long-term influence on many cellular reactions (51).
Being different from biochemical molecular which inducing chondrogenic and osteogenic differentiation on stem cells, the influence of Mg2+ on cell metabolic pattern and cell stiffness may dictate the fate of stem cell in more basic or downstream way (58,59). Mg2+ has the intrinsic capability to co-regulate cell energy metabolism, cytoskeleton arrangement, protein synthesis and, indirectly, the onset of DNA synthesis. So we postulate that the mechanism of chondrogenic effect of Mg2+ on cartilage progenitor cells and chondrocytes may be dependent on the inner pathway related to ATP production and/or cytoskeleton arrangement in these cells.
Intracellular functions of Mg ions
The pathway of Mg2+ transmembrane shipping into chondrocytes is not clear yet. Nonetheless, Mg2+ transport from extracellular fluid to cytoplasm had been deeply studied in the past two decades. Genetic screenings on human diseases and microarray-based expression studies have resulted in the identification of numerous Mg2+ transporting proteins. In eukaryocytes, membrane Mg channels are a broad range of transmembrane proteins with similar structures and amino sequences. They are generally encoded as SLC41A1, SLC41A2, Mrs2, ACDP2, Paracellin-1, Claudin 16, TUSC3, MagT1, TRPM6, and TRPM7 genes, which have same role in prokaryotic cells (60,61). Among them, TRPM7 is ubiquitously expressed in all tissues, and it is proved to combine with TRPM6 to form a TRPM6/TRPM7 heteo-oligomerization and create Mg transmembrane conduction in distal convoluted tubule (62). Channel MagT1 is also expressed in all tissues and is considered responsible for mammalian cell Mg2+ uptake (61,63).
Under resting conditions, Mg2+ slowly moves across the cell membrane with a turnover of several hours. Yet, increasing or decreasing the extracelluar Mg2+ will change significantly total intracellular Mg2+ content (64). In general, intracellular Mg primarily fulfills various intracellular physiological functions as a cofactor of DNA, RNA, ATP, and almost all 600 enzymes (55,65). Mg has two general types of interaction with an enzyme: (I) binding to an enzyme substrate in the reaction of kinases with Mg-ATP, thereby forming a complex with the enzyme; and (II) binding directly to the enzyme, thereby altering its structure and/or serving as catalytic player.
Mg2+ affects mitochondria activities
In a typical mammalian cell, 90% of total cytosolic Mg2+ is bound to ATP in the cytosol or sequestered within nuclei, mitochondria and endoplasmic reticulum (ER) (65). Numerous experimental and clinical data have suggested that Mg2+ deficiency can induce elevation of intracellular Ca2+ concentrations, formation of oxygen radicals such as reactive oxide species (ROS), proinflammatory agents and changes in membrane permeability and transport processes in cells (66,67). It was found that cardiomyocytes are exposed to hypoxia for 1 hour and reoxygenation for 2 hours, and ROS level is increased 100–130% during reoxygenation alone. Yet the ROS level is further down regulated to 60% by increasing extracellular Mg2+ concentration to 5 mM at reoxygenation (68).
Mitochondria is a major source of intracellular Mg2+, half of the mitochondria Mg2+ is localized in the mitochondria matrix, 40% of which is present in the intermembrane space and the remaining 10% are equally bound at the outer and inner membrane level (~5% each) (65). A change in external Mg2+ modulates the rate of oxidative phosphorylation (OxPhos) and respiratory rate in mitochondria through modulation in the activities of the succinate and glutamate dehydrogenases in intact rat heart mitochondria (69). The myocardial protective effect of Mg2+ is mainly by inhibiting intracellular Ca2+ overload through blocking L-type Ca2+ channel, and recovering mitochondrial membrane potential by opening the mitochondrial KATP channel during hypoxia (70).
In studies of stem cells, endogenous ROS generated from the mitochondrial electron transport chain (ETC) complex III is required to initiate directed adipogenesis of MSCs (71). Unlike adipogenesis, osteogenesis cannot tolerate ROS. In fact, antioxidant enzymes such as superoxide dismutase and catalase are simultaneously up regulated with OxPhos in osteoblasts to prevent ROS accumulation (58,72). In contrast to adipogenesis and osteogenesis, MSCs undergoing chondrogenesis have significantly reduced O2 consumption and OxPhos, indicating a shift towards increased glycolysis. Furthermore, hypoxia inhibits MSCs osteogenesis, whereas chondrogenesis is unaffected (73,74).
Taken together, these studies indicate that subtle manipulation of oxidative consumption and energy productive ways by intracellular Mg2+ directly influence the differentiation of MSCs either into osteoblasts, adipocytes or chondroblasts. Actually, Mg2+ is found regulating proliferation and differentiation in stem cells by altering mitochondria function in latest study (75,76). However, the detailed effect of Mg ions on cell energy metabolism and its consequences in stem cell fate need to be explored in future studies.
Mg affects cytoskeleton arrangement
Besides biochemical signals regulating MSCs commitment, biomechanical signals directly and indirectly played important roles in regulating a stem cell fate (77).
Cytoskeletal contractility by actin-actomyosin system is an important mechanical regulator of directing stem cell differentiation. Inhibiting the cytoskeletal contractility by reducing Rho-associated kinase (ROCK), nonmuscle myosin II and FAK activities lead to adipogenesis (77). The chndrogenic and osteogenic differentiation of MSCs probably correlates with the FAK activity and the cytoskeletal contractility. The contractile cytoskeleton consists of actin, myosin, microtubules and intermediate filaments (78). Remodeling of the actin cytoskeleton through actin dynamics is involved in a number of biological processes (79). The cellular contractility induces downstream events including the recruitment of adhesion molecules and kinases such as the mechanosensitive FAK, zyxin and talin, subsequently triggering the activation of Rho GTPases (80). In eukaryotic cells, the lipid membrane is connected to the actin cortex via the family of members of the ezrin-radixin-moesin (ERM) linker proteins, including ezrin, radixin and moesin (81).
MSCs exhibit inherent plasticity in terms of their ability to differentiate into different lineage including chondrocytes and osteoblasts (82,83). MSCs are softer in quiescent state than in differentiated state which is likely to influence cellular functions including mechano-transduction and migration (83). The increased stiffness of differentiated cells is resulted from the increased membrane-cortex adhesion, and the differentiated cells exhibited greater F-actin density and slower actin remodeling (83). Polymerization of actin is regulated by a series of kinases, such as GTPase RhoA, ROCK, and LIM kinases, which phosphorylates the actin depolymerizing protein cofilin and stabilizes actin filaments (84). Stabilizing polymerized actin filaments increases hMSCs viability and osteoblast and chondroblast differentiation (85). Activation of actin depolymerization and consequently reducing the cell tension by cytochalasin D or inhibition of ROCK activity mimics the phenotype of poor spread cells, resulting in adipogenesis (85). This effect of cytochalasin D is due to its promotion of ATPase activity in cells, which is contrary to effect of Mg2+ in our studies for dorsal root ganglia neurons (57).
ATP hydrolysis occurs on F-actin in two subsequent reactions, cleavage of ATP followed by the slower release of Pi. ATP is hydrolyzed (at the rate of 1/3.3 s−1) following the elongation of filaments at the growing end of filaments, whereas the Pi release is 100 times slower (86). As a result, newly polymerized filaments consist of stable ADP-Pi actin (F-ADP-Pi), whereas the older filaments contain mainly ADP actin (F-ADP), which disassembles more rapidly (86). Actin dynamics also depends on the identity of the bound divalent cation, physiologically Mg2+, associated with the bound nucleotide (87). Effect of Mg2+ on actin polymerization is not studied thoroughly yet, however, the action between Mg2+ and non-muscle myosin is well studied.
Previous studies with motor proteins such as myosin traditionally focus on Mg2+ as a cofactor in ATP binding, hydrolysis, and product release in the force-generating mechanochemical cycle (88). In recent studies, Mg2+ inhibit class I, II, V myosins and class VII myosins in a Mg2+ dependent manner (0.3–9.0 mM free Mg2+) in both ATPase and motility assays (88-90). The results demonstrate that Mg2+ alters key steps in mechanochemical cycle by coupling the nucleotide and actin-binding regions. It alters the structural transition that limits ADP dissociation from actomyosin. Because the ADP release step is rate-limiting in myosin, increasing free Mg2+ concentration slows the myosin ATPase activity as well as sliding velocity. The mechanism of altering detachment is likely due to Mg2+ exchange in the active site, although it is unclear how Mg2+ impacts attachment. Higher concentrations of free Mg ions stabilize the tension-bearing actin myosin ADP state and shift the system from the production of rapid movement toward the generation of tension.
The total tension present in the plasma membrane (i.e., the “apparent” membrane tension) has a minor contribution from the surface tension of the lipid bilayer and a substantial contribution from the molecular contacts that afford adhesion to the underlying actin cytoskeleton (88). To prevent large changes in tension is the inner request of stem cells in quiescent state, and the plasma membrane must maintain continuous interactions with the cytoskeleton (80). In this process, MSCs are particularly susceptible to membrane blebbing, membrane-cytoskeleton structure is highly dynamic and continuously remodeling in undifferentiated MSCs (83). The increased tension indicates the increased critical pressure for membrane-actin cortex detachment or bond strength in MSCs following differentiation. Meanwhile, this “blebability” is reduced during chondrogenic differentiation with significant increases in instantaneous and equilibrium moduli (83).
Under quantitative confocal microscopy, the differentiated cells have longer recovery times indicative of a more stable actin cortex with slower turnover compared to hMSCs in review of actin organization and dynamics (91). This is in agreement with the observations of increased membrane-cortex adhesion which in turn influences cell mechanics by reducing bleb formation (83). Here we point out the reduced membrane bleb formation along with chondrogenic and osteogenic effect of Mg2+ on MSCs is a probable mechanism of Mg2+ suppression to osteoclasts whose function are mainly dependent formation of blebbing and vesicles (92,93).
Interaction between extracellular Mg2+ and integrins
Cells adhere to the underlying ECM substrate by employing membrane-bound integrins. A large complex network of adhesion molecules has been shown crucial for stem cells and force-mediated differentiation, some of the important structural proteins in cell adhesion include integrin, talin, vinculin and FAK (80). Integrin structurally contains three distinct divalent cation-binding sites. Two binding sites where integrin interacts with its ligand are occupied by Mg2+, presence of Mg2+ is essential for integrin-ligand binding and their presence is required for cell adhesion (59,94).
From in vitro investigations on chondrocytes, it is known that several integrins are present on chondrocytes and that the cell-matrix interaction is mediated by integrin receptors of the β1 subfamily (18). These receptors recently be demonstrated to be exist in human cartilage, and they are reduced in rat chondrocytes after ofloxacin treatment (95). Because binding of integrins and its receptors require divalent cations, particularly Mg2+, integrins’ function could be impaired in Mg deficiency or by Mg2+-chelating agents such as quinolones in cartilage tissue (95,96). So it had been speculated that impairment of cell-matrix interaction through integrins activation is one of the possible mechanism in Mg-deficiency induced arthropathy.
Mg2+ is involved in direct activation and the regulation of signal cascades of integrins (97,98). In chondrocytes, at least eight different types of integrins are expressed and play the important roles in differentiation and the interaction of chondrocytes with the ECM (99). Mg2+ is found increased adhesion of hMSCs to collagen, and this effect is inhibited by neutralizing antibodies for integrin α3 and β1. In this study, Mg2+ also promotes synthesis of cartilage matrix during in vitro chondrogenesis of synovial MSCs, however, the chondrogenic differentiation effect of Mg2+ is diminished by neutralizing antibodies for integrin β1 but not for integrin α3 (100). It was also reported that high concentration of Mg2+ promotes proliferation of human bone marrow-derived stromal cells (hBMSCs) via integrins α2 and α3, but not β1 (54). It is fascinating that whether intracellular Mg2+ or extracellular Mg2+ which directly binding to cell membrane integrin domain which protruding out of the cytoplasm (101), is enrolled in the differed differentiation pathway in stem cells. In further studies, it is pivotal to explore the effect between intracellular/extracellular Mg2+ and integrin regulation to understand the role of Mg2+ on chondrogenic differentiation (51).
Mg in treatment of OA and future direction
Based on its chondrocyte benevolent effects of Mg2+, Mg salts have been studied in the OA treatment in recent years, actually only in the bench now and still far from the bed. CH. Lee et al. firstly intra-articularly injected MgSO4 in the OA Wistar rats caused by intra-articular injection of collagenase (500 U) in the knee, and Mg2+ significantly reduced the severity of cartilage degradation in the OA knee (102). OA rats receiving intra-articular MgSO4 injections showed a significantly lower degree of cartilage degeneration than the rats receiving saline injections, synovitis phenomenon was also suppressed after MgSO4 treatment (102). Mechanical allodynia and thermal hyperalgesia showed significant improvement in the OA + MgSO4 group as compared to the OA group (102). It had been considered that the inflamed state of arthritic knees is characterized by the presence of neural transmitters such as SP and glutamate in the inflamed region and synovial fluid (103). These neural transmitters in the knee joint result in thermal hyperalgesia and mechanical allodynia, which conducted through N-methyl-D-aspartic acid (NMDA) receptor on synoviocytes and chondrocytes (104). Mg2+ acts as an antagonist at the glutamate subtype of NMDA receptors and blocks NMDA-induced currents in a voltage-dependent manner by blocking receptor channel effects (105,106). Dietary restriction of Mg intake lowers the mechanical nociceptive thresholds in rats, which can be reversed by the NMDA receptor antagonist, MK-801 (102). Local intra-articular administration of MgSO4 modulates chondrocyte metabolism through inhibition of cell NMDA receptor phosphorylation and apoptosis, attenuates the development of OA and concomitantly reduces nociception (102). Even in normal rat knee joint, intra-articular injection of MgCl2 solution had no significant adverse effect of inflammation and cartilage degeneration compared to saline injection (107).
Mg2+ is a potential therapeutic agent in the treatment of the OA. Further research is needed not only to better define the administration mode of Mg2+ on OA but also to clarify the role of Mg2+ as a NMDA antagonist in OA treatment. In our recent published work, Mg2+ significantly promotes replasticity in sensory neurons, and increases up regulation of neural transmitters (e,g., calcitonin gene-related peptide) which facilitates osteogenesis and bone fracture healing (57). It reminds us that the biological effects of Mg2+ are multi-systems and far-ranging to neuron, myocyte, osteoblast, osteoclast, fibroblast, chondrocyte, epithelial cell, progenitor cell and stem cell. In cartilage, there is few sensory nerves and neural peptides, the direct effect of Mg2+ on chondrocytes and progenitor cells should be well studied.
At the present, drug treatments for OA are pain alleviating and/or antagonizing to inflammation factors (e.g., TNF-α, IL-1β/6/8), most of conservative treatments cannot even slow the progression of OA. At the later stage of OA, patients usually have to receive total knee/hip replacement surgery. So both clinicians and researchers are trying to find the efficacious treatment to prevent the progression and cure the OA in the early stage. It was found that MSCs are recruited and aggregated into the damaged tissue site and differentiate into chondrocytes in the beginning of OA (108,109). However, the stem cells gradually lost their differential capability during the persisting inflammation (110). As we review above, Mg ions can promote the chondrogenic differentiation on MSCs. Meanwhile, Mg ions also perform its significant inhibiting effect on the inflammation activities to osteoclasts (93). Our previous study showed that the expression of nucleostemin (a stem cell nucleus marker which is well maintained in quiescence and mitosis and down-regulated in differentiation) in cartilage was decreased after Mg treatment in rat OA model. It indicates Mg2+ may well keep the viability and differential potent of cartilage stem cells. That makes Mg a new prospective drug in the conservative treatment for OA through locally administrating Mg ions in the lesioned cartilage.
The fascinating effect of Mg in musculoskeletal system enlightens us to explore the existence of stem cells or chondrocyte progenitors in cartilage tissue, and search for the cause accounting for the losing capability of these cells in cartilage repair. Thoroughly understanding the mechanism of Mg ions’ curing effect on OA would inspire the new findings for cartilage self-repairing processing, and design feasible ways to treat early OA.
Acknowledgments
Funding: Dr. Yifeng Zhang was supported by The Central University Basic Scientific Research Funding (technological innovation project) (021414380113) and science and technology projects of Jiangsu province (natural science funds—the youth science fund—BK20160633).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2016.11.04). QJ serves as an Editor-in-Chief of Annals of Joint from Mar 2016 to Feb 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Johnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol 2014;28:5-15. [Crossref] [PubMed]
- Sandell LJ. Etiology of osteoarthritis: genetics and synovial joint development. Nat Rev Rheumatol 2012;8:77-89. [PubMed]
- Tang X, Wang S, Zhan S, et al. The Prevalence of Symptomatic Knee Osteoarthritis in China: Results From the China Health and Retirement Longitudinal Study. Arthritis Rheumatol 2016;68:648-53. [Crossref] [PubMed]
- Xue Q, Wang K, Pei F, et al. The survey of the prevalence of primary osteoarthritis in the population aged 40 years and over in China. Chin J Orthop 2015;35:1206-12.
- Loeser RF. Age-related changes in the musculoskeletal system and the development of osteoarthritis. Clin Geriatr Med 2010;26:371-86. [Crossref] [PubMed]
- Brodziak-Dopierała B, Kwapuliński J, Sobczyk K, et al. Distribution of magnesium, calcium, sodium and potassium in tissues of the hip joint. Magnes Res 2013;26:125-31. [PubMed]
- Yazar M, Sarban S, Kocyigit A, et al. Synovial fluid and plasma selenium, copper, zinc, and iron concentrations in patients with rheumatoid arthritis and osteoarthritis. Biol Trace Elem Res 2005;106:123-32. [Crossref] [PubMed]
- Wu L, Feyerabend F, Schilling AF, et al. Effects of extracellular magnesium extract on the proliferation and differentiation of human osteoblasts and osteoclasts in coculture. Acta Biomater 2015;27:294-304. [Crossref] [PubMed]
- Orchard TS, Larson JC, Alghothani N, et al. Magnesium intake, bone mineral density, and fractures: results from the Women's Health Initiative Observational Study. Am J Clin Nutr 2014;99:926-33. [Crossref] [PubMed]
- Aydin H, Deyneli O, Yavuz D, et al. Short-term oral magnesium supplementation suppresses bone turnover in postmenopausal osteoporotic women. Biol Trace Elem Res 2010;133:136-43. [Crossref] [PubMed]
- Scotchford CA, Vickers M, Ali SY. The isolation and characterization of magnesium whitlockite crystals from human articular cartilage. Osteoarthritis Cartilage 1995;3:79-94. [Crossref] [PubMed]
- Scotchford CA, Ali SY. Association of magnesium whitlockite crystals with lipid components of the extracellular matrix in human articular cartilage. Osteoarthritis Cartilage 1997;5:107-19. [Crossref] [PubMed]
- Scotchford CA, Ali SY. Magnesium whitlockite deposition in articular cartilage: a study of 80 specimens from 70 patients. Ann Rheum Dis 1995;54:339-44. [Crossref] [PubMed]
- Ryan LM, Cheung HS, LeGeros RZ, et al. Cellular responses to whitlockite. Calcif Tissue Int 1999;65:374-7. [Crossref] [PubMed]
- Khalaf G. Effect Of Magnesium Deficiency On The Articular Cartilage, The Growth Plate And The Trabecular Bone In Young Male Albino Rats Histological And Histochemical Study. The Egyptian Journal Of Histology 2006;29:205-12.
- Vormann J, Förster C, Zippel U, et al. Effects of magnesium deficiency on magnesium and calcium content in bone and cartilage in developing rats in correlation to chondrotoxicity. Calcif Tissue Int 1997;61:230-8. [Crossref] [PubMed]
- Stahlmann R, Kühner S, Shakibaei M, et al. Effects of magnesium deficiency on joint cartilage in immature beagle dogs: immunohistochemistry, electron microscopy, and mineral concentrations. Arch Toxicol 2000;73:573-80. [Crossref] [PubMed]
- Shakibaei M, Kociok K, Förster C, et al. Comparative evaluation of ultrastructural changes in articular cartilage of ofloxacin-treated and magnesium-deficient immature rats. Toxicol Pathol 1996;24:580-7. [Crossref] [PubMed]
- Gruber HE, Ingram J, Norton HJ, et al. Alterations in growth plate and articular cartilage morphology are associated with reduced SOX9 localization in the magnesium-deficient rat. Biotech Histochem 2004;79:45-52. [Crossref] [PubMed]
- Förster C, Schwabe R, Lozo E, et al. Quinolone-induced arthropathy: exposure of magnesium-deficient aged rats or immature rats, mineral concentrations in target tissues and pharmacokinetics. Arch Toxicol 1997;72:26-32. [Crossref] [PubMed]
- Förster C, Rücker M, Shakibaei M, et al. Effects of fluoroquinolones and magnesium deficiency in murine limb bud cultures. Arch Toxicol 1998;72:411-9. [Crossref] [PubMed]
- Qin B, Shi X, Samai PS, et al. Association of dietary magnesium intake with radiographic knee osteoarthritis: results from a population-based study. Arthritis Care Res (Hoboken) 2012;64:1306-11. [Crossref] [PubMed]
- Afridi HI, Kazi TG, Kazi N, et al. Evaluation of calcium, magnesium, potassium, and sodium in biological samples (scalp hair, serum, blood, and urine) of Pakistani referents and arthritis patients of different age groups. Clin Lab 2012;58:7-18. [PubMed]
- Zeng C, Li H, Wei J, et al. Association between Dietary Magnesium Intake and Radiographic Knee Osteoarthritis. PLoS One 2015;10:e0127666 [Crossref] [PubMed]
- Zeng C, Wei J, Li H, et al. Relationship between Serum Magnesium Concentration and Radiographic Knee Osteoarthritis. J Rheumatol 2015;42:1231-6. [Crossref] [PubMed]
- Dieppe PA, Crocker P, Huskisson EC, et al. Apatite deposition disease. A new arthropathy. Lancet 1976;1:266-9. [Crossref] [PubMed]
- Schumacher HR, Miller JL, Ludivico C, et al. Erosive arthritis associated with apatite crystal deposition. Arthritis Rheum 1981;24:31-7. [Crossref] [PubMed]
- McCarty DJ, Lehr JR, Halverson PB. Crystal populations in human synovial fluid. Identification of apatite, octacalcium phosphate, and tricalcium phosphate. Arthritis Rheum 1983;26:1220-4. [Crossref] [PubMed]
- Guggenbuhl P. Basic calcium phosphate crystal deposition disease. Rev Prat 2015;65:681. [PubMed]
- Halverson PB, McCarty DJ. Patterns of radiographic abnormalities associated with basic calcium phosphate and calcium pyrophosphate dihydrate crystal deposition in the knee. Ann Rheum Dis 1986;45:603-5. [Crossref] [PubMed]
- Salimi MH, Heughebaert JC, Nancollas GH. Crystal growth of calcium phosphates in the presence of magnesium ions. Langmuir 1985;1:119-22. [Crossref]
- Egerbacher M, Wolfesberger B, Gabler C. In vitro evidence for effects of magnesium supplementation on quinolone-treated horse and dog chondrocytes. Vet Pathol 2001;38:143-8. [Crossref] [PubMed]
- Baker JF, Byrne D, Walsh PM, et al. Local anaesthetic toxicity to human chondrocytes is reduced by addition of magnesium. Orthopaedic Proceedings 2012;94-B:050.
- Cao X, Harris WG, Josan MS, et al. Inhibition of calcium phosphate precipitation under environmentally-relevant conditions. Sci Total Environ 2007;383:205-15. [Crossref] [PubMed]
- Cao X, Harris W. Carbonate and magnesium interactive effect on calcium phosphate precipitation. Environ Sci Technol 2008;42:436-42. [Crossref] [PubMed]
- Xu N, Yin H, Chen Z, et al. Mechanisms of phosphate retention by calcite: effects of magnesium and pH. J Soils Sediments 2014;14:495-503. [Crossref]
- Wilkins E, Dieppe P, Maddison P, et al. Osteoarthritis and articular chondrocalcinosis in the elderly. Ann Rheum Dis 1983;42:280-4. [Crossref] [PubMed]
- Loeser RF. Aging and osteoarthritis: the role of chondrocyte senescence and aging changes in the cartilage matrix. Osteoarthritis Cartilage 2009;17:971-9. [Crossref] [PubMed]
- Günther T, Schümann K, Vormann J. Tumor necrosis factor-Â, prostanoids and immunoglobulins in magnesium deficiency. Magnes Bull 1995;17:109-14.
- Weglicki WB, Stafford RE, Dickens BF, et al. Inhibition of tumor necrosis factor-alpha by thalidomide in magnesium deficiency. Mol Cell Biochem 1993;129:195-200. [Crossref] [PubMed]
- Maguire ME, Cowan JA. Magnesium chemistry and biochemistry. Biometals 2002;15:203-10. [Crossref] [PubMed]
- Musso CG. Magnesium metabolism in health and disease. Int Urol Nephrol 2009;41:357-62. [Crossref] [PubMed]
- Rubin H. Central roles of Mg2+ and MgATP2- in the regulation of protein synthesis and cell proliferation: significance for neoplastic transformation. Adv Cancer Res 2005;93:1-58. [Crossref] [PubMed]
- Rubin H. Magnesium: The missing element in molecular views of cell proliferation control. Bioessays 2005;27:311-20. [Crossref] [PubMed]
- Rubin H. The logic of the Membrane, Magnesium, Mitosis (MMM) model for the regulation of animal cell proliferation. Arch Biochem Biophys 2007;458:16-23. [Crossref] [PubMed]
- Baker JF, Byrne DP, Walsh PM, et al. Human chondrocyte viability after treatment with local anesthetic and/or magnesium: results from an in vitro study. Arthroscopy 2011;27:213-7. [Crossref] [PubMed]
- Baker JF, Walsh PM, Byrne DP, et al. In vitro assessment of human chondrocyte viability after treatment with local anaesthetic, magnesium sulphate or normal saline. Knee Surg Sports Traumatol Arthrosc 2011;19:1043-6. [Crossref] [PubMed]
- Dou Y, Li N, Zheng Y, et al. Effects of fluctuant magnesium concentration on phenotype of the primary chondrocytes. J Biomed Mater Res A 2014;102:4455-63. [PubMed]
- Martínez-Sánchez AH, Feyerabend F, Luthringer B, et al. Effect of magnesium extracts on the chondrogenic differentiation of HUCPV cells. Eur Cell Mater 2014;28:69.
- Luthringer BJ, Willumeit-Römer R. Effects of magnesium degradation products on mesenchymal stem cell fate and osteoblastogenesis. Gene 2016;575:9-20. [Crossref] [PubMed]
- Feyerabend F, Witte F, Kammal M, et al. Unphysiologically high magnesium concentrations support chondrocyte proliferation and redifferentiation. Tissue Eng 2006;12:3545-56. [Crossref] [PubMed]
- Dou Y, Mujeebb A, Zheng Y, et al. Optimization of dual effects of Mg–1Ca alloys on the behavior of chondrocytes and osteoblasts in vitro. Progress in Natural Science: Materials International 2014;24:433-40. [Crossref]
- Yoshizawa S, Brown A, Barchowsky A, et al. Magnesium ion stimulation of bone marrow stromal cells enhances osteogenic activity, simulating the effect of magnesium alloy degradation. Acta Biomater 2014;10:2834-42. [Crossref] [PubMed]
- Leem YH, Lee KS, Kim JH, et al. Magnesium ions facilitate integrin alpha 2- and alpha 3-mediated proliferation and enhance alkaline phosphatase expression and activity in hBMSCs. J Tissue Eng Regen Med 2016;10:E527-E536. [Crossref] [PubMed]
- Romani AM, Scarpa A. Regulation of cellular magnesium. Front Biosci 2000;5:D720-34. [Crossref] [PubMed]
- Moe SM. Disorders involving calcium, phosphorus, and magnesium. Prim Care 2008;35:215-37. v-vi. [Crossref] [PubMed]
- Zhang Y, Xu J, Ruan YC, et al. Implant-derived magnesium induces local neuronal production of CGRP to improve bone-fracture healing in rats. Nat Med 2016;22:1160-1169. [Crossref] [PubMed]
- Shyh-Chang N, Daley GQ, Cantley LC. Stem cell metabolism in tissue development and aging. Development 2013;140:2535-47. [Crossref] [PubMed]
- Chen S, Lewallen M, Xie T. Adhesion in the stem cell niche: biological roles and regulation. Development 2013;140:255-65. [Crossref] [PubMed]
- Schmitz C, Deason F, Perraud AL. Molecular components of vertebrate Mg2+-homeostasis regulation. Magnes Res 2007;20:6-18. [PubMed]
- Zhou H, Clapham DE. Mammalian MagT1 and TUSC3 are required for cellular magnesium uptake and vertebrate embryonic development. Proc Natl Acad Sci U S A 2009;106:15750-5. [Crossref] [PubMed]
- Chubanov V, Waldegger S, Mederos y Schnitzler M, et al. Disruption of TRPM6/TRPM7 complex formation by a mutation in the TRPM6 gene causes hypomagnesemia with secondary hypocalcemia. Proc Natl Acad Sci U S A 2004;101:2894-9. [Crossref] [PubMed]
- Wolf FI, Trapani V. MagT1: a highly specific magnesium channel with important roles beyond cellular magnesium homeostasis. Magnes Res 2011;24:S86-91. [PubMed]
- Romani A. Regulation of magnesium homeostasis and transport in mammalian cells. Arch Biochem Biophys 2007;458:90-102. [Crossref] [PubMed]
- Romani AM. Cellular magnesium homeostasis. Arch Biochem Biophys 2011;512:1-23. [Crossref] [PubMed]
- Rock E, Astier C, Lab C, et al. Magnesium deficiency in rats induces a rise in plasma nitric oxide. Magnes Res 1995;8:237-42. [PubMed]
- Kumar BP, Shivakumar K. Depressed antioxidant defense in rat heart in experimental magnesium deficiency. Implications for the pathogenesis of myocardial lesions. Biol Trace Elem Res 1997;60:139-44. [Crossref] [PubMed]
- Sharikabad MN, Ostbye KM, Lyberg T, et al. Effect of extracellular Mg(2+) on ROS and Ca(2+) accumulation during reoxygenation of rat cardiomyocytes. Am J Physiol Heart Circ Physiol 2001;280:H344-53. [PubMed]
- Chakraborti S, Chakraborti T, Mandal M, et al. Protective role of magnesium in cardiovascular diseases: a review. Mol Cell Biochem 2002;238:163-79. [Crossref] [PubMed]
- Sharikabad MN, Ostbye KM, Brørs O. Increased [Mg2+]o reduces Ca2+ influx and disruption of mitochondrial membrane potential during reoxygenation. Am J Physiol Heart Circ Physiol 2001;281:H2113-23. [PubMed]
- Tormos KV, Anso E, Hamanaka RB, et al. Mitochondrial complex III ROS regulate adipocyte differentiation. Cell Metab 2011;14:537-44. [Crossref] [PubMed]
- Chen CT, Shih YR, Kuo TK, et al. Coordinated changes of mitochondrial biogenesis and antioxidant enzymes during osteogenic differentiation of human mesenchymal stem cells. Stem Cells 2008;26:960-8. [Crossref] [PubMed]
- Pattappa G, Heywood HK, de Bruijn JD, et al. The metabolism of human mesenchymal stem cells during proliferation and differentiation. J Cell Physiol 2011;226:2562-70. [Crossref] [PubMed]
- Pattappa G, Thorpe SD, Jegard NC, et al. Continuous and uninterrupted oxygen tension influences the colony formation and oxidative metabolism of human mesenchymal stem cells. Tissue Eng Part C Methods 2013;19:68-79. [Crossref] [PubMed]
- Jia S, Mou C, Ma Y, et al. Magnesium regulates neural stem cell proliferation in the mouse hippocampus by altering mitochondrial function. Cell Biol Int 2016;40:465-71. [Crossref] [PubMed]
- Yue J, Jin S, Li Y, et al. Magnesium inhibits the calcification of the extracellular matrix in tendon-derived stem cells via the ATP-P2R and mitochondrial pathways. Biochem Biophys Res Commun 2016;478:314-22. [Crossref] [PubMed]
- Wang YK, Chen CS. Cell adhesion and mechanical stimulation in the regulation of mesenchymal stem cell differentiation. J Cell Mol Med 2013;17:823-32. [Crossref] [PubMed]
- Yang GN, Kopecki Z, Cowin AJ. Role of Actin Cytoskeleton in the Regulation of Epithelial Cutaneous Stem Cells. Stem Cells Dev 2016;25:749-59. [Crossref] [PubMed]
- Titushkin I, Cho M. Modulation of cellular mechanics during osteogenic differentiation of human mesenchymal stem cells. Biophys J 2007;93:3693-702. [Crossref] [PubMed]
- Yim EK, Sheetz MP. Force-dependent cell signaling in stem cell differentiation. Stem Cell Res Ther 2012;3:41. [Crossref] [PubMed]
- Charras GT, Hu CK, Coughlin M, et al. Reassembly of contractile actin cortex in cell blebs. J Cell Biol 2006;175:477-90. [Crossref] [PubMed]
- Yu H, Tay CY, Leong WS, et al. Mechanical behavior of human mesenchymal stem cells during adipogenic and osteogenic differentiation. Biochem Biophys Res Commun 2010;393:150-5. [Crossref] [PubMed]
- Sliogeryte K, Thorpe SD, Lee DA, et al. Stem cell differentiation increases membrane-actin adhesion regulating cell blebability, migration and mechanics. Sci Rep 2014;4:7307. [Crossref] [PubMed]
- Ono S. Mechanism of depolymerization and severing of actin filaments and its significance in cytoskeletal dynamics. Int Rev Cytol 2007;258:1-82. [Crossref] [PubMed]
- Chen L, Shi K, Frary CE, et al. Inhibiting actin depolymerization enhances osteoblast differentiation and bone formation in human stromal stem cells. Stem Cell Res 2015;15:281-9. [Crossref] [PubMed]
- Murakami K, Yasunaga T, Noguchi TQ, et al. Structural basis for actin assembly, activation of ATP hydrolysis, and delayed phosphate release. Cell 2010;143:275-87. [Crossref] [PubMed]
- Pollard TD, Cooper JA. Actin, a central player in cell shape and movement. Science 2009;326:1208-12. [Crossref] [PubMed]
- Swenson AM, Trivedi DV, Rauscher AA, et al. Magnesium modulates actin binding and ADP release in myosin motors. J Biol Chem 2014;289:23977-91. [Crossref] [PubMed]
- Fujita-Becker S, Dürrwang U, Erent M, et al. Changes in Mg2+ ion concentration and heavy chain phosphorylation regulate the motor activity of a class I myosin. J Biol Chem 2005;280:6064-71. [Crossref] [PubMed]
- Trivedi DV, Muretta JM, Swenson AM, et al. Magnesium impacts myosin V motor activity by altering key conformational changes in the mechanochemical cycle. Biochemistry 2013;52:4710-22. [Crossref] [PubMed]
- González-Cruz RD, Fonseca VC, Darling EM. Cellular mechanical properties reflect the differentiation potential of adipose-derived mesenchymal stem cells. Proc Natl Acad Sci U S A 2012;109:E1523-9. [Crossref] [PubMed]
- Wu L, Luthringer BJ, Feyerabend F, et al. Effects of extracellular magnesium on the differentiation and function of human osteoclasts. Acta Biomater 2014;10:2843-54. [Crossref] [PubMed]
- Zhai Z, Qu X, Li H, et al. The effect of metallic magnesium degradation products on osteoclast-induced osteolysis and attenuation of NF-κB and NFATc1 signaling. Biomaterials 2014;35:6299-310. [Crossref] [PubMed]
- Mould AP, Garratt AN, Puzon-McLaughlin W, et al. Regulation of integrin function: evidence that bivalent-cation-induced conformational changes lead to the unmasking of ligand-binding sites within integrin alpha5 beta1. Biochem J 1998;331:821-8. [Crossref] [PubMed]
- Förster C, Kociok K, Shakibaei M, et al. Integrins on joint cartilage chondrocytes and alterations by ofloxacin or magnesium deficiency in immature rats. Arch Toxicol 1996;70:261-70. [Crossref] [PubMed]
- Egerbacher M, Wolfesberger B, Walter I, et al. Integrins mediate the effects of quinolones and magnesium deficiency on cultured rat chondrocytes. Eur J Cell Biol 1999;78:391-7. [Crossref] [PubMed]
- Grzesiak JJ, Davis GE, Kirchhofer D, et al. Regulation of alpha 2 beta 1-mediated fibroblast migration on type I collagen by shifts in the concentrations of extracellular Mg2+ and Ca2+. J Cell Biol 1992;117:1109-17. [Crossref] [PubMed]
- Yoshinaga IG, Dekker SK, Mihm MC Jr, et al. Differential effect of magnesium and calcium on integrin-mediated melanoma cell migration on type IV collagen and fibronectin. Melanoma Res 1994;4:371-8. [Crossref] [PubMed]
- Loeser RF. Integrins and cell signaling in chondrocytes. Biorheology 2002;39:119-24. [PubMed]
- Shimaya M, Muneta T, Ichinose S, et al. Magnesium enhances adherence and cartilage formation of synovial mesenchymal stem cells through integrins. Osteoarthritis Cartilage 2010;18:1300-9. [Crossref] [PubMed]
- Zhang K, Chen J. The regulation of integrin function by divalent cations. Cell Adh Migr 2012;6:20-9. [Crossref] [PubMed]
- Lee CH, Wen ZH, Chang YC, et al. Intra-articular magnesium sulfate (MgSO4) reduces experimental osteoarthritis and nociception: association with attenuation of N-methyl-D-aspartate (NMDA) receptor subunit 1 phosphorylation and apoptosis in rat chondrocytes. Osteoarthritis Cartilage 2009;17:1485-93. [Crossref] [PubMed]
- Ramage L, Martel MA, Hardingham GE, et al. NMDA receptor expression and activity in osteoarthritic human articular chondrocytes. Osteoarthritis Cartilage 2008;16:1576-84. [Crossref] [PubMed]
- Lawand NB, Willis WD, Westlund KN. Excitatory amino acid receptor involvement in peripheral nociceptive transmission in rats. Eur J Pharmacol 1997;324:169-77. [Crossref] [PubMed]
- Anand A. Role of magnesium in alleviating pain: newer insights. J Pain Symptom Manage 2000;20:1-2. [Crossref] [PubMed]
- Srebro DP, Vučković SM, Savić Vujović KR, et al. TRPA1, NMDA receptors and nitric oxide mediate mechanical hyperalgesia induced by local injection of magnesium sulfate into the rat hind paw. Physiol Behav 2015;139:267-73. [Crossref] [PubMed]
- Ansam Aly, Farouk S, Abdelatti RM. The Effect of Intra-Articular Magnesium on the Articular Cartilage and Synovium in the Rat Knee Joint. Australian Journal of Basic & Applied Sciences 2014;6:572.
- Jiang Y, Tuan RS. Origin and function of cartilage stem/progenitor cells in osteoarthritis. Nat Rev Rheumatol 2015;11:206-12. [Crossref] [PubMed]
- Barry F, Murphy M. Mesenchymal stem cells in joint disease and repair. Nat Rev Rheumatol 2013;9:584-94. [Crossref] [PubMed]
- Alsalameh S, Amin R, Gemba T, et al. Identification of mesenchymal progenitor cells in normal and osteoarthritic human articular cartilage. Arthritis Rheum 2004;50:1522-32. [Crossref] [PubMed]
Cite this article as: Zhang Y, Xu J, Qin L, Jiang Q. Magnesium and osteoarthritis: from a new perspective. Ann Joint 2016;1:29.