
Revision of bilateral total hip arthroplasty for failed primary arthroplasty: a case report
Introduction
Total hip arthroplasty (THA) remains one of the commonest as well as most advanced surgical procedures performed since the 20th century (1). In recent years many patients have undergone this procedure with great success rate. Increased mobility and life expectancy has resulted in a surge in demand for this procedure (2). The increased demand also follows that the rate of revision THA will surge in the future.
Revision THA is a challenging task for the orthopedic surgeon, with several medical equipment requirements (3). The survival rate for the past 12 years is 60% to 81% for cementless revision THA (4). A study performed by Lie et al. considered 4,762 revisions THA, and showed that the 10-year risk for infection was 25.6%, with a higher risk when septic revisions are included (5). However a research done by Springer et al. showed that the 11-year survival rate of revision arthroplasty was 81% in infected cases. In the case of aseptic loosening, the 10-year survival rate of revision THA showed to be 81% (4). The reason for loosening remains unclear, but poor bone quality, excessive body weight, wear of the plastic liner between the ball and the metal cup, repetitive high impact activities etc., have been implicated for dislocation and infection (6).
Factors that determine hip revision prognosis may be divided into three categories: patient-related factors, implant-related factors and insufficient surgical technique related failures (7). Patient-related factors include co-morbidities like sickle-cell anemia (8), implant-related factors involve pre-prosthetic fractures (9) and insufficient surgical technique related failures comprise of recurrent dislocation, malpositioning of components and technical problems (10). The most common indications for revision THA include osteolysis, infection and aseptic loosening due to failure of bearing surfaces (11). In a Swedish study, 75% of patients that underwent revision THA suffered osteolysis as a complication (12). The femur and acetabulum components may be affected.
The purpose of this case report was to demonstrate complicated bilateral THA in young patients and how we manage them pre and postoperatively.
Case presentation
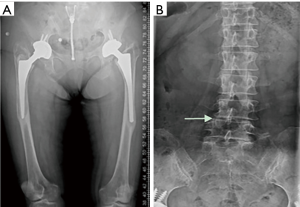
A 51-year-old female with a history of bilateral recurrent hip pain for more than ten years, aggravated for the past 1 year, presented to the outpatient department of Southeast University Affiliated to Zhongda Hospital, Nanjing, China, on February 2017. She had a history of hypertension for more than 10 years, with nephritis as co-morbidity. The hypertension was controlled with antihypertensive medications, while the nephritis was cured before her primary surgery. Her primary surgery was a THA performed in 2007 at a local hospital. It was indicated due to her bilateral femoral head avascular necrosis. Six years post-operatively, the patient had recurrent symptoms of right hip pain. Consequently, she underwent a second right THA at the same hospital. On further examination at our hospital, lumbar, pelvic and bilateral hip axial radiography showed: bilateral hip replacement variations; pelvic and bilateral hip degeneration; lumbar L4–5 vertebral body compression and osteoporosis (Figure 1). Her blood routine indicated normal ESR, CRP and white blood cell count. For further treatment, she was referred to the orthopedic department, where she was diagnosed with “Bilateral Total Hip arthroplasty and osteoporosis”. The primary indication for revision THA was stem aseptic loosening due to low quality implantation, which resulted in ‘osteolysis’. This inflammatory process typically occurs in artificial joint replacement procedures such as total hip replacement, total knee replacement and total shoulder replacement that lead to revision surgery. Consequently, the surgeon purposed her for Bilateral Revision Total Hip arthroplasty.
Preoperative assessment and planning
Before the operation, it is vital to elucidate the possible complications, selected treatment method, treatment alternatives as well as possible outcome, to the patient. The patient needs to understand that after this procedure, she may require crutches or walkers for some time. Preoperatively it is necessary to evaluate medical tests, as well as optimize the patient for surgery. These tests include blood routine, urine and stool tests, electrocardiograph (ECG), and chest X-ray. For this patient they were all normal, except for IL-6 which was significantly high. She also tested positive for Hepatitis B.
Due to long term stem loosening, proximal femur valgus deformity occurred. This is an indication for extended trochanteric osteotomy (ETO), to avoid femoral fracture and distal well-fix implant. Further use of ETO can improve acetabular exposure. The length of osteotomy and type of prosthetic stem were decided through preoperative anteroposterior and lateral radiograph, respectively. For this patient, cylindrical titanium full of porous coated prosthetic straight stem, was decided. A more quality acetabular cup was indicated, since good polyethylene will help improve the durability of the new joint for a relatively young patient like her. To minimize complications, the surgeon decided to operate unilateral revision hip arthroplasty.
Surgical procedure
The patient was placed in a left lateral decubitus position, and the right lower extremity was disinfected and draped with skin protective film. A skin incision was made on the previous scar, at the right hip posterolaterally to the revision THA. During the dissection to reach the hip, much fibrosis was visible adjacent to the hip joint. The normal anatomy was not clearly observed, so a careful dissection was carried out with the support of electrocautery. The surgeon paid careful attention to the neurovascular structures around the femur. The tissue around the subcutaneous and muscle fascia was removed as the joint cavity was approached. The previous femur prosthesis seemed loose, so was easily removable. To avoid bone loss or femur shaft fracture, the fibrosed tissue was carefully removed. Then the stem was gradually taken out with the help of sharp thin osteotomy. The acetabulum peripheral to soft tissue was exposed, and the scar was released. Furthermore, the surgeon removed the polyethylene liner, cup fixation screws and acetabular cup with the help of an extended blade, and took out the granulation tissue. After reaming the acetabular cavity, the new porous titanium cup was fixed with two screws. A proximal femur extended greater trochanter osteotomy (ETO) was performed. It had a length of 13 cm. A large amount of infected tissue was removed, and the medullary cavity was reamed for more than 6 cm. A new 22.5 cm long prosthetic stem was then implanted. To fix the greater trochanter fragment, hip prosthesis stabilization and reduction of the trochanter osteotomy, three titanium cable rings were used. To do a traction reduction of the hip joint and avoid dislocation, posterior capsule and external rotator flap was closed with a non-absorbable #1 suture. After pulsatile lavage, the drainage tube was placed and the soft tissue behind the joint was repaired. The surgical incision was sutured layer by layer. 4 Units of whole blood and 480 mL of fresh frozen plasma were transfused into the patient perioperatively, in order to stabilize her. Antibiotics were also administered to reduce risk of infection. After the surgery the patient was moved to the orthopedic department for further evaluation and treatment. Post-operative radiography was done, which showed no complication such as dislocation, fracture or inappropriate alignment.
Similarly, the same procedure was performed on the left side, with the patient lying on the right lateral decubitus position, and the left lower extremity disinfected. There was a difference in length of the proximal femur extended greater trochanter osteotomy (ETO), which was 14 cm. The size of prosthetic stem implant however, was the same (22.5 cm). The surgery was initially performed on the right side, and then on the left side with 15 days apart, which took about 6 hours 10 minutes and 5 hours 45 minutes respectively. General Anesthesia was used for these procedures.
Postoperative management
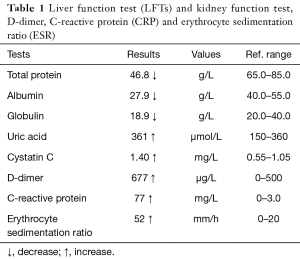
After the right revision surgery, the surgeon prescribed iron-rich foods and blood transfusion. This was indicated due to low hemoglobin levels and red blood cell count, so as to improve oxygen carrying capacity. Due to the surgery, the serum calcium level was low. Thus intravenous and oral calcium supplements were prescribed. Human serum albumin was advised for the low albumen level, and some electrolytes as well as other supportive treatments were given for pain and improved bone healing. On the third day, liver and renal function tests showed low total protein, albumin, globulin levels, and high uric acid and cystatin C (Table 1). D-dimer, erythrocyte sedimentation ratio and C-reactive protein were all increased (Table 1). Antibiotics were prescribed for the high CRP, which indicates the presence of infection.
Full table
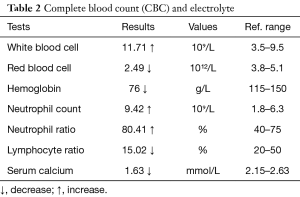
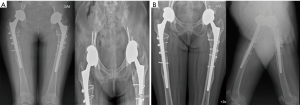
The patient was assisted to elevate the limb in order to reduce swelling, and perform non-weight-bearing limb activities to prevent thrombosis. Low-molecular-weight heparin and limb compression device were employed. The above measures were continued for more than one week. Eventually, the patient’s limb activity improved with complete recovery. Plain radiography was taken on the fourth postoperative day (Figure 2A,B). The surgeon then decided to operate a left revision THA.

After the left revision surgery, the patient’s blood routine showed: low red blood cell and hemoglobin counts, as well as low lymphocyte ratio. On the other hand, white blood cell and neutrophil ratio were high (Table 2). Due to low hemoglobin and red blood cell counts, iron supplements and blood transfusion were given. For pain, swelling and bone healing, supportive treatment and electrolytes were administered to improve nutrition. To prevent thrombosis, low molecular weight heparin was initiated. Oral calcium supplements were also prescribed for her low calcium levels (Table 2).
Full table
Plain radiography was taken on the fifth postoperative day (Figure 2C,D). Moreover, the patient’s CRP and ESR were high due to infection. The doctor then prescribed antibiotics for four weeks. However, two weeks after the antibiotic administration, the patient’s blood report showed normal inflammatory markers. This then informed the ruling out of postoperative infection.
On the eleventh postoperative day, radiography showed no complications (Figure 3). The surgeon then asked the patient to perform non-weight bearing limb activities, while continuing supportive and symptomatic treatments. Few days later, the patient’s condition greatly improved, and she was discharged from the hospital.
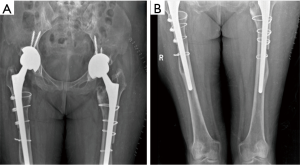
The patient maintained partial weight bearing activities for 4 weeks, and was able to return to her normal activities on the 6th week. Her follow-up visits were scheduled for once every three months for the first six months, and then once every 6 months. Her follow-ups were devoid of the usual complications (Figure 4).
Discussion
A lot of studies have been carried out on the Caucasian population about the indications for revision THA, which have established the different causes of failed primary THA (13). Osteonecrosis as a primary diagnosis was the main highlight for the Caucasian population, and primary THA are done at a relatively younger age (6).
Patients who underwent primary hip surgery at an early age faced increased risk for aseptic loosening. Primary THA is affected by the frequency of hip articulation, due to friction between ball and socket surfaces. This wear and tear produces tiny particles that trigger an immune response to produce inflammatory mediators. This in turn leads to bone resorption and destruction, termed ‘Osteolysis’. Aseptic loosening then results overtime due to bone resorption which weakens the prosthetic. It then begins to move freely in the bone, resulting in hip pain.
Other factors leading to failure of primary THA include gender (women tend to have a higher risk for complications due to loosening or instability), infection and periprosthetic fracture (which is more common in men).
The primary aims of revision THA are to acquire instant fixation and long-term steadiness. Hence, we considered a 51-year-old female with a history of bilateral recurrent hip pain for more than 10 years, for revision THA. The main cause of failure of her primary THA was aseptic loosening due to osteolysis, which resulted from previous low quality prosthetic components implanted. The patient’s proximal femur valgus deformity occurred as a result of long term stem loosening. The surgeon then decided to perform an ETO, to prevent femoral fracture and firmly fix distal implant. To determine the length of osteotomy and type of prosthetic stem to be used, anteroposterior and lateral radiograph respectively were taken. For this patient, a cylindrical extensively porous coated femoral stem, was selected to improve the durability of the new joint.
After bilateral revision THA was performed, the outcome was satisfactory, as there were no complications after 1 year of follow up.
Moreover, revision THA is a challenging and time-consuming procedure for surgeons, requiring assessment of all parameters that lead to failed primary THA. Subsequently, postoperative complications and length of hospital stay increases (3). However, the benefits far outweigh the risk.
Conclusions
Although revision THA is a complicated surgical procedure, it is also considered one of the most successful treatment options for failed THA. Yet, risk-benefit ratio must be assessed pre-operatively. Thus, this procedure should be considered only when other treatment modalities have failed. In this case, bilateral revision THA was performed with favorable outcomes, and no complication after one year of follow up.
However, patients ensuing revision THA require long-term follow up and rehabilitation by a multidisciplinary team, which has to be well thought out for rapid recovery.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.05.03). JL serves as an unpaid editorial board member of Annals of Joint from Jun 2016 to May 2018. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Eisler T, Svensson O, Tengstrom A, et al. Patient expectation and satisfaction in revision total hip arthroplasty. J Arthroplasty 2002;17:457-62. [Crossref] [PubMed]
- Kuster MS. Exercise recommendations after total joint replacement: a review of the current literature and proposal of scientifically based guidelines. Sports Med 2002;32:433-45. [Crossref] [PubMed]
- Crowe JF, Sculco TP, Kahn B. Revision total hip arthroplasty: hospital cost and reimbursement analysis. Clin Orthop Relat Res 2003;175-82. [Crossref] [PubMed]
- Springer BD, Fehring TK, Griffin WL, et al. Why revision total hip arthroplasty fails. Clin Orthop Relat Res 2009;467:166-73. [Crossref] [PubMed]
- Lie SA, Havelin LI, Furnes ON, et al. Failure rates for 4762 revision total hip arthroplasties in the Norwegian Arthroplasty Register. J Bone Joint Surg Br 2004;86:504-9. [Crossref] [PubMed]
- Inacio MC, Ake CF, Paxton EW, et al. Sex and risk of hip implant failure: assessing total hip arthroplasty outcomes in the United States. JAMA Intern Med 2013;173:435-41. [Crossref] [PubMed]
- Ong A, Wong KL, Lai M, et al. Early failure of precoated femoral components in primary total hip arthroplasty. J Bone Joint Surg Am 2002;84-A:786-92. [Crossref] [PubMed]
- Vichinsky EP, Neumayr LD, Haberkern C, et al. The perioperative complication rate of orthopedic surgery in sickle cell disease: report of the National Sickle Cell Surgery Study Group. Am J Hematol 1999;62:129-38. [Crossref] [PubMed]
- Sarvilinna R, Huhtala HS, Puolakka TJ, et al. Periprosthetic fractures in total hip arthroplasty: an epidemiologic study. Int Orthop 2003;27:359-61. [Crossref] [PubMed]
- Phillips CB, Barrett JA, Losina E, et al. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg Am 2003;85-A:20-6. [Crossref] [PubMed]
- Furnes O, Lie SA, Espehaug B, et al. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987–99. J Bone Joint Surg Br 2001;83:579-86. [Crossref] [PubMed]
- Malchau H, Herberts P, Eisler T, et al. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am 2002;84-A:2-20. [Crossref] [PubMed]
- Bergh C, Fenstad AM, Furnes O, et al. Increased risk of revision in patients with non-traumatic femoral head necrosis. Acta Orthop 2014;85:11-7. [Crossref] [PubMed]
Cite this article as: Sarwar S, Lu J, Arfat SM, Marcella C, Ji ML, Mohamed ISAS. Revision of bilateral total hip arthroplasty for failed primary arthroplasty: a case report. Ann Joint 2018;3:44.


